Main reasons for development
Dystrophic processes in corneal tissues are often caused by hereditary predisposition, therefore they are mainly diagnosed in children at an early age. Factors that trigger the progression of the disease:
- advanced ophthalmological pathologies;
- neurological disorders that negatively affect the trophism of tissues of the organs of vision;
- mechanical or chemical injury;
- chronic infectious bacterial inflammation.
Classification
Considering the etiology, the following types of disorders are distinguished:
- primary;
- secondary.
The disease can occur in a nodular type. Depending on the nature of the course and the severity of symptoms, there are types of dystrophy, such as:
- nodular;
- microcystic epithelial;
- endothelial;
- marginal pellucidal;
- mesodermal;
- band-shaped corneal dystrophy.
Atrophy of the corneal structures is often observed in old age. This is due to a violation of lipid metabolism in the body, as a result of which the cornea rapidly becomes cloudy, and the person loses vision. This ophthalmological pathology, which arises as a result of age-related changes, is called senile arch; the predisposing factor in its development is heredity.
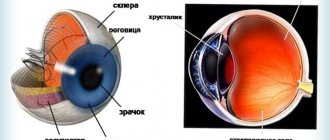
Anatomy of the cornea
- Function
- Composition of the cornea
- Structure of the cornea
- Physiology of the cornea
The cornea, or cornea, is convex in front and concave in back, a transparent, avascular plate of the eyeball, which is a direct continuation of the sclera. The human cornea occupies approximately 1/6 of the outer layer of the eye. It looks like a convex-concave lens, the place where it transitions into the sclera (limb) looks like a translucent ring up to 1 mm wide. Its presence is explained by the fact that the deep layers of the cornea extend posteriorly somewhat further than the anterior ones.
The diameter of the cornea is 11-12 mm in the horizontal plane and 9-11 in the vertical plane. In the center its thickness is 450-600 microns, and at the periphery - 650-750 microns. This indicator also correlates with age: for example, at 20-30 years old, the thickness of the cornea is 0.534 and 0.707 mm, and at 71-80 years old - 0.518 and 0.618 mm.
Distinctive qualities of the cornea:
- Spherical (radius of curvature of the front surface ~7.7 mm, rear surface 6.8 mm)
- Mirror shiny
- Lacking blood vessels
- Has high tactile and pain, but low temperature sensitivity
- Refracts light rays with a power of 40-43 diopters.
Function
The cornea is the optical structure of the eye; its refractive power is, on average, 45D (diopters) in children in the first year of life, and by the age of 7, as in adults, it is about 40D. The refractive power of the cornea in the vertical meridian is slightly greater than in the horizontal one (physiological astigmatism).
Dimensions
- The horizontal diameter in adults is 11 mm (in newborns - 9 mm).
- Vertical diameter - 10 mm, in newborns - 8 mm.
- The thickness in the center is 0.4-0.6 mm, in the peripheral part - 0.8-1.2 mm.
- The radius of curvature of the anterior surface of the cornea in adults is 7.5 mm, in newborns - 7 mm.
The cornea grows by thinning and stretching the tissue.
Composition of the cornea
The corneal epithelium develops from the ectoderm, all other elements of the cornea - from the neuroectoderm (neural crest). After invagination of the lens, the corneal stroma is formed in the form of a layer of loose collagenous substance between the ectoderm and the lens. At approximately 6 weeks of intrauterine development, mesenzymal cells from the perilimbal cell mass begin to form endothelium, and the stroma is populated by perilimbic fibroblasts (future keratocytes). By the time of birth, the cornea is relatively enlarged relative to other structures of the eyeball; corneal growth ends by 2 years of age.
The cornea contains water, collagen of mesenchymal origin, mucopolysaccharides, proteins (albumin, globulin), lipids, and vitamins. The transparency of the cornea depends on the correct location of the structural elements and the same refractive indices, as well as the water content in it (normally up to 75%; an increase in water above 86% leads to clouding of the cornea).
Changes in the cornea in old age
- the amount of moisture and vitamins decreases,
- globulin fractions of proteins predominate over albumin fractions,
- calcium salts and lipids are deposited.
In this regard, the area of transition of the cornea into the sclera, the limbus, changes first of all: the surface layers of the sclera seem to move onto the cornea, and the internal ones lag behind somewhat; the cornea becomes like glass inserted into a watch bezel. Due to metabolic disorders, a so-called senile arch is formed, and the sensitivity of the cornea decreases.
Structure of the cornea
- The surface layer of the cornea is squamous stratified epithelium, which is a continuation of the connective membrane of the eye (conjunctiva). The thickness of the epithelium is 0.04 mm. This layer regenerates well and quickly when damaged, without leaving cloudiness. The epithelium performs a protective function and is a regulator of water content in the cornea. The corneal epithelium, in turn, is protected from the external environment by the so-called liquid, or basal, layer.
- The anterior limiting plate - Bowman's membrane is loosely connected to the epithelium, so in case of pathology the epithelium can easily be torn off. It is structureless, inelastic, homogeneous, has a low level of metabolism, and is not capable of regeneration, so when it is damaged, opacities remain. The thickness in the center is 0.02 mm, and less at the periphery.
- The cornea's own substance (stroma) is a thick, transparent middle layer consisting of thin connective tissue, regularly located plates containing collagen fibrils, in which single wandering cells are located - fibroblasts and lymphoid elements that perform a protective function. They are parallel and overlap each other like the pages of a book. To better connect them, mucoprotein is located in the spaces between the layers. The stroma is up to 0.5 mm thick, nonvascular, and composed of approximately 200 layers of mostly type I collagen fibrils.
- The posterior limiting elastic lamina (Descemet's membrane) is a thin acellular layer that serves as the basement membrane of the corneal endothelium, from which all cells develop. This layer consists mainly of type IV collagen fibers, which are more elastic than type I collagen. The thickness of this layer is about 5-20 microns, depending on the age of the patient. Anterior to the Descimet membrane is a very thin but quite strong Dua layer, the thickness of which is only 15 microns, and the load capacity is from 1.5 to 2 bar of pressure, according to research.
- The endothelium is the inner part of the cornea, facing the anterior chamber of the eye and washed by the intraocular fluid. It consists of a single-layer squamous or cubic epithelium, the cells are rich in mitochondria, the thickness of the layer is about 0.05 mm. This layer protects the stroma from the direct effects of aqueous humor, simultaneously ensuring metabolic processes between it and the cornea, and has a pronounced barrier function (unlike the epithelium of the surface layer of the cornea, the endothelium does not regenerate; instead, there is a continuous division process that compensates for dead cells); participates in the formation of the trabecular apparatus of the iridocorneal angle.
Physiology of the cornea
The temperature of the cornea is approximately 10°C lower than body temperature, which is due to direct contact of the moist surface of the cornea with the external environment, as well as the absence of blood vessels in it. With closed eyelids, the temperature of the cornea at the limbus is 35.4 °C, and in the center 35.1 °C (with open eyelids ~30 °C).
In this regard, the growth of mold fungi with the development of specific keratitis is possible.
Since there are no lymphatic and blood vessels, nutrition and metabolism in the cornea occurs by osmosis and diffusion (due to tear fluid, anterior chamber moisture and pericorneal blood vessels).
The absence of blood vessels in the cornea is compensated by abundant innervation, which is represented by trophic, sensory and autonomic nerve fibers. Metabolic processes in the cornea are regulated by trophic nerves arising from the trigeminal and facial nerves.
The high sensitivity of the cornea is provided by a system of long ciliary nerves (from the ophthalmic branch of the trigeminal nerve), which form the perilimbal nerve plexus around the cornea. As they enter the cornea, they lose their myelin sheath and become invisible. Three tiers of nerve plexuses are formed in the cornea - in the stroma, under the basal (Bowman's) membrane and subepithelial. The closer to the surface of the cornea, the thinner the nerve endings become and the denser their interweaving. Almost every cell of the anterior corneal epithelium is provided with a separate nerve ending. This explains the high tactile sensitivity of the cornea and the pronounced pain syndrome when the sensitive endings are exposed (epithelial erosion).
The high sensitivity of the cornea underlies its protective function: when you lightly touch the surface of the cornea and even when the wind blows, an unconditioned corneal reflex occurs - the eyelids close, the eyeball turns upward, moving the cornea away from danger, and a tear fluid appears, washing away dust particles.
The afferent part of the corneal reflex arc is carried by the trigeminal nerve, and the efferent part is carried by the facial nerve. Loss of the corneal reflex occurs with severe brain damage (shock, coma). The disappearance of the corneal reflex is an indicator of the depth of anesthesia. The reflex disappears with some lesions of the cornea and upper cervical spinal cord.
The rapid direct response of the vessels of the marginal lemniscus to any irritation of the cornea occurs due to the fibers of the sympathetic and parasympathetic nerves present in the perilimbal nerve plexus. They are divided into 2 endings, one of which passes to the walls of the vessel, and the other penetrates the cornea and contacts the branched network of the trigeminal nerve.
General information
Synonyms for familial hypercholesterolemia are primary, hereditary hypercholesterolemia. It is not an independent disease, but a state of predisposition to cardiovascular diseases - vascular atherosclerosis, coronary artery disease, acute myocardial infarction. Data on the prevalence of FH have a wide range, since in many cases the pathology remains undiagnosed. The frequency of the heterozygous form, in which the patient has one defective gene of a pair, is 1 case per 108-300 people. The homozygous form, characterized by the presence of two mutation genes in the allele, is more severe and occurs much less frequently - in 1 person out of 1 million. Among all types of hypercholesterolemia, familial hypercholesterolemia accounts for 10% of cases.
FH is a hereditary autosomal dominant pathology that is caused by mutations in the genes responsible for the metabolism of LDL and the activity of its receptors. If there is one defective gene in a couple, heterozygous hypercholesterolemia occurs - a mild to moderate disorder of lipid metabolism. In rare cases, patients have two paired altered genes (from the mother and from the father), and homozygous hypercholesterolemia develops - a severe disorder of lipid metabolism with a malignant course. Familial hypercholesterolemia is caused by a mutation in one of the following genes:
- LDLR .
The gene determines the functionality of the LDL receptor, located mainly on the surface of liver cells. When mutation occurs, its activity decreases, the process of binding and removing circulating lipoproteins from the bloodstream is disrupted. More than 1,600 types of LDLR gene mutations have been identified. Their share in the total number of SGHS is 85-90%. - APOB .
The gene defect leads to a change in the structure of apolipoprotein B100, which is part of LDL, ensuring their binding to the receptor. Mutational changes in APOB are present in 5-10% of patients with hereditary hypercholesterolemia. They cause a less pronounced increase in LDL than LDLR mutations. - PCSK9.
This gene encodes the enzyme proprotein convertase subtilisin-kexin type 9, which enhances the destruction of LDL receptors. Mutations in the PCSK9 gene increase the activity of the enzyme, resulting in a decrease in the number of receptors. This type of pathology occurs in 5% of cases of FH.
Signs
Hypercholesterolemia is a laboratory indicator that is determined during a biochemical blood test.
Patients with hypercholesterolemia often develop xanthomas - skin neoplasms from altered cells, which are compacted nodules containing lipid inclusions inside. Xanthomas accompany all forms of hypercholesterolemia, being one of the manifestations of lipid metabolism disorders. Their development is not accompanied by any subjective sensations, in addition, they are prone to spontaneous regression.
Source: estet-portal.com
Xanthomas are divided into several types:
- eruptive - small yellow papules, localized mainly on the thighs and buttocks;
- tuberous - have the appearance of large plaques or tumors, which, as a rule, are located in the buttocks, knees, elbows, on the back of the fingers, face, and scalp. New growths may have a purple or brown tint, a reddish or cyanotic border;
- tendinous - localized mainly in the area of the extensor tendons of the fingers and Achilles tendons;
- flat - most often found in the folds of the skin, especially on the palms;
- xanthelasmas are flat xanthomas of the eyelids, which are yellow plaques raised above the skin. More often found in women, they are not prone to spontaneous resolution.
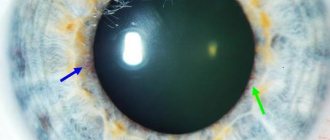
Another manifestation of hypercholesterolemia is cholesterol deposits along the periphery of the cornea of the eye (lipoid arch of the cornea), which look like a white or grayish-white rim. Lipoid arc of the cornea is more often observed in smokers and is almost irreversible. Its presence indicates an increased risk of developing coronary heart disease.
With the homozygous form of familial hypercholesterolemia, a significant increase in the level of cholesterol in the blood is observed, which is manifested by the formation of xanthoma and lipoid arch of the cornea already in childhood. During puberty, such patients often develop atheromatous lesions of the aortic mouth and stenosis of the coronary arteries of the heart with the development of clinical manifestations of coronary heart disease. In this case, acute coronary insufficiency cannot be ruled out, which can cause death.
The heterozygous form of familial hypercholesterolemia, as a rule, remains undetected for a long time, manifesting itself as cardiovascular failure in adulthood. Moreover, women develop the first signs of pathology on average 10 years earlier than men.
Hypercholesterolemia can lead to the development of atherosclerosis. In turn, this causes damage to blood vessels, which can have various manifestations.
An increase in cholesterol levels in the blood provokes the development of atherosclerosis, which, in turn, is manifested by vascular pathology (mainly atherosclerotic lesions of the blood vessels of the lower extremities, but damage to the brain, coronary vessels, etc. is also possible).
How does it manifest?
EED of the cornea may not appear in the initial stages of progression, but over time the patient will feel discomfort and other unpleasant symptoms, such as:
With this pathology, a person’s vision may become worse.
- sensation of a foreign object in the eye;
- pain;
- swelling formation;
- blurred vision, which may be a symptom of retinal detachment;
- deterioration of visual functions;
- photophobia;
- increased lacrimation;
- the appearance of a corneal arc around the iris of the eye.
Types of disease
Creptopathy can be either congenital, in most cases hereditary, or acquired, due to various reasons. The hereditary form is characterized by the death of corneal cells due to genetics, vesicles form in the affected area, both eyes are affected and vision gradually deteriorates until complete loss. The acquired form most often affects one eye, and development usually occurs at a rapid pace, but the pathology can be cured with timely diagnosis. The disease includes the following types:
- The bullous form appears as blisters with clear liquid on the cornea.
- Lipoid is characterized by the appearance of fatty deposits on the cornea.
- Ribbon-shaped appears in the form of deposits of calcium salts on the membrane.
- Pinpoint can be manifested by the feeling of a foreign body on the cornea.
Diagnostics
In order for the treatment of pathology to be effective and correct, it is first necessary to determine an accurate diagnosis and find out the reasons under the influence of which such defects arose. For dystrophic eye lesions, you must make an appointment with an ophthalmologist. After an external examination and history taking, the doctor will give a referral for diagnostic tests such as:
- corneal microscopy;
- biomicroscopy;
- pachymetry;
- visometry.
Defects in the ocular membrane can be identified using its microscopy. Microscopic diagnosis will show clouding of the corneal layer, the formation of small nodules and other inclusions. The marginal area of the cornea is transparent, there are no signs of vascularization. At a progressive stage, the cornea becomes thin, the endothelium is also thinned, and with extensive swelling on the surface of the cornea, bullae are formed, which are a symptom of the onset of the development of bullous keratopathy. Senile corneal arch lipoidia is diagnosed during a physical examination using a slit lamp.
Causes and treatment of corneal dystrophy
A disease in which degeneration and death of the endothelial cells of the eye occurs is called epithelial endothelial dystrophy of the cornea.
This defect is accompanied by severe symptoms that require immediate response.
The causes of dystrophic changes in the corneal epithelium are varied, therefore, before starting treatment, it is necessary to find out what factor triggered the development of ophthalmological pathology.
According to the international classification of diseases ICD 10, the pathology is assigned code H18.4 “Corneal degeneration” and H18.5 “Hereditary dystrophies”.
Main reasons for development
Dystrophic processes in corneal tissues are often caused by hereditary predisposition, therefore they are mainly diagnosed in children at an early age. Factors that trigger the progression of the disease:
- advanced ophthalmological pathologies;
- neurological disorders that negatively affect the trophism of tissues of the organs of vision;
- mechanical or chemical injury;
- chronic infectious bacterial inflammation.
Classification
Considering the etiology, the following types of disorders are distinguished:
The disease can occur in a nodular type.
Depending on the nature of the course and the severity of symptoms, there are types of dystrophy, such as:
- nodular;
- microcystic epithelial;
- endothelial;
- marginal pellucidal;
- mesodermal;
- band-shaped corneal dystrophy.
Atrophy of the corneal structures is often observed in old age. This is due to a violation of lipid metabolism in the body, as a result of which the cornea rapidly becomes cloudy, and the person loses vision. This ophthalmological pathology, which arises as a result of age-related changes, is called senile arch; the predisposing factor in its development is heredity.
How does it manifest?
EED of the cornea may not appear in the initial stages of progression, but over time the patient will feel discomfort and other unpleasant symptoms, such as:
With this pathology, a person’s vision may become worse.
- sensation of a foreign object in the eye;
- pain;
- swelling formation;
- blurred vision, which may be a symptom of retinal detachment;
- deterioration of visual functions;
- photophobia;
- increased lacrimation;
- the appearance of a corneal arc around the iris of the eye.
Diagnostics
In order for the treatment of pathology to be effective and correct, it is first necessary to determine an accurate diagnosis and find out the reasons under the influence of which such defects arose. For dystrophic eye lesions, you must make an appointment with an ophthalmologist. After an external examination and history taking, the doctor will give a referral for diagnostic tests such as:
- corneal microscopy;
- biomicroscopy;
- pachymetry;
- visometry.
Defects in the ocular membrane can be identified using its microscopy.
Microscopic diagnosis will show clouding of the corneal layer, the formation of small nodules and other inclusions. The marginal area of the cornea is transparent, there are no signs of vascularization.
At a progressive stage, the cornea becomes thin, the endothelium is also thinned, and with extensive swelling on the surface of the cornea, bullae are formed, which are a symptom of the onset of the development of bullous keratopathy.
Senile corneal arch lipoidia is diagnosed during a physical examination using a slit lamp.
Drugs
At the initial stage of development, corneal dystrophy is treated conservatively. For this purpose, special eye drops are used, which must be prescribed by the doctor after making an accurate diagnosis.
Decongestants and vitamin and mineral complexes are often used. If an inflammatory complication develops, antibiotics must be prescribed. You cannot do without medications that improve the regeneration and nutrition of damaged eye tissue.
The following products have proven themselves to be effective:
- ointment "Solcoseryl";
- gel "Actovegin";
- Visomitin drops.
Laser stimulation will enhance the effect of the medications used.
Laser stimulation, during which the cornea is exposed to a low-energy laser beam, will help improve the effect of drug therapy.
After the procedure, restoration processes are activated, due to which the progression of the pathology is suspended.
Senile senile arch does not require special treatment; the patient is prescribed a diet and medications that will help normalize cholesterol levels in the blood.
Surgical
It is not always possible to cure this disease with medication. If corneal dystrophy progresses and the patient’s vision rapidly deteriorates, the doctor decides to perform surgery, after which the corneal layer will begin to gradually recover.
Patients with this degenerative disease often undergo keratoplasty, during which the damaged corneal tissue is replaced with a donor graft.
At the end of the operation, stitches are applied, then a rehabilitation period will follow, during which it is important to protect the eyes from the negative effects of external factors, wear a special bandage, and use restorative medications.
Therapy with folk remedies
The patient's body's defenses will improve when consuming propolis tincture.
You can use non-traditional methods to treat corneal dystrophy only after consultation with an ophthalmologist, since self-medication can provoke dangerous complications.
Home remedies are recommended to be used as an addition to primary drug therapy. To strengthen the corneal layer and increase the body's protective functions, it is useful to take courses of propolis tincture, which you buy at the pharmacy or prepare yourself.
The recipe for natural medicine is simple:
- Grind 80 g of bee glue with a knife and combine with 300 ml of vodka, heated to 40 °C.
- Place the ingredients in a dark glass container and leave to infuse in a dark place for 2 weeks.
- The product needs to be shaken periodically.
- Take the finished tincture 20 drops. 3 rubles/day for 30 min. before meals.
A folk remedy in the form of a medicinal ointment, which is prepared as follows, has also proven itself well:
- Combine 1 tsp. fresh honey and royal jelly.
- Mix the products well, then add 1 spoon of chilled boiled water to them and mix again until smooth.
- Take the resulting medicinal mixture into a new syringe without a needle and place it under the eyelid as an ophthalmic ointment.
- Carry out the procedure 2-3 times a day until the negative symptoms disappear.
Complications
If left untreated, homozygous primary hypercholesterolemia promotes the development of atherosclerosis up to 20 years of age; the life expectancy of patients does not exceed 30 years. Untreated patients with a heterozygous form of the pathology have a high risk of developing coronary artery disease; by the age of 60, the diagnosis is confirmed in 85.5% of men and 53% of women. Average life expectancy for men is 53 years, for women – 62 years. IHD causes the death of half of men with hereditary heterozygous hypercholesterolemia. About 20% of myocardial infarction cases under 45 years of age are associated with the presence of FH.
What treatment is prescribed?
Drugs
At the initial stage of development, corneal dystrophy is treated conservatively. For this purpose, special eye drops are used, which must be prescribed by the doctor after making an accurate diagnosis. Decongestants and vitamin and mineral complexes are often used. If an inflammatory complication develops, antibiotics must be prescribed. You cannot do without medications that improve the regeneration and nutrition of damaged eye tissue. The following products have proven themselves to be effective:
- ointment "Solcoseryl";
- gel "Actovegin";
- Visomitin drops.
Laser stimulation will enhance the effect of the medications used. Laser stimulation, during which the cornea is exposed to a low-energy laser beam, will help improve the effect of drug therapy. After the procedure, restoration processes are activated, due to which the progression of the pathology is suspended. Senile senile arch does not require special treatment; the patient is prescribed a diet and medications that will help normalize cholesterol levels in the blood.
Surgical
It is not always possible to cure this disease with medication. If corneal dystrophy progresses and the patient’s vision rapidly deteriorates, the doctor decides to perform surgery, after which the corneal layer will begin to gradually recover. Patients with this degenerative disease often undergo keratoplasty, during which the damaged corneal tissue is replaced with a donor graft. At the end of the operation, stitches are applied, then a rehabilitation period will follow, during which it is important to protect the eyes from the negative effects of external factors, wear a special bandage, and use restorative medications.
Diagnostic methods
The main methods for diagnosing corneal pathology are the following laboratory and instrumental studies:
- blood analysis;
- ophthalmoscopy;
- biomicroscopy;
- histochemical analysis;
- perimetry.
Additionally, liver tests, vascular angiogram and lipid profile may be prescribed. To confirm the diagnosis, the ophthalmologist can use special drops that dilate the pupils, with which you can study in detail the condition of the eye vessels.
Forms of hypercholesterolemia
Hypercholesterolemia is divided into primary and secondary.
In accordance with the classification of the World Health Organization, the following forms of hypercholesterolemia are distinguished:
- type I (hereditary hyperchylomicronemia, primary hyperlipoproteinemia) - incidence 0.1%, occurs with lipoprotein lipase deficiency or defects in the activator protein of this enzyme, manifested by an increase in the level of chylomicrons, which transport lipids from the intestine to the liver;
- type IIa (hereditary hypercholesterolemia, polygenic hypercholesterolemia) – frequency of occurrence is 0.2%, can develop against the background of poor nutrition, and can also be polygenic or hereditary, manifested by xanthomas and early onset of cardiovascular pathology;
- type IIb (combined hyperlipidemia) - incidence 10%, occurs due to excessive production of triglycerides, acetyl-CoA and apolipoprotein B or slow clearance of low-density lipoproteins; accompanied by an increase in the blood content of triglycerides in the composition of very low density lipoproteins;
- type III (hereditary dys-beta-lipoproteinemia) – frequency of occurrence is 0.02%, can develop with homozygosity for one of the isoforms of apolipoprotein E, manifested by an increase in the level of intermediate density lipoproteins and chylomicrons;
- type IV (endogenous hyperlipemia) – frequency of occurrence is about 1%, manifested by an increase in triglyceride concentrations;
- type V (hereditary hypertriglyceridemia) - manifested by increased levels of very low-density lipoproteins and chylomicrons.
Rarer forms of hypercholesterolemia that are not included in this classification include hypo-alpha lipoproteinemia and hypo-beta lipoproteinemia, the incidence of which is 0.01–0.1%.
Familial hypercholesterolemia can be homozygous or heterozygous.
The main method for detecting hypercholesterolemia is a biochemical blood test.
Therapy with folk remedies
The patient's body's defenses will improve when consuming propolis tincture. You can use non-traditional methods to treat corneal dystrophy only after consultation with an ophthalmologist, since self-medication can provoke dangerous complications. Home remedies are recommended to be used as an addition to primary drug therapy. To strengthen the corneal layer and increase the body's protective functions, it is useful to take courses of propolis tincture, which you buy at the pharmacy or prepare yourself. The recipe for natural medicine is simple:
- Grind 80 g of bee glue with a knife and combine with 300 ml of vodka, heated to 40 °C.
- Place the ingredients in a dark glass container and leave to infuse in a dark place for 2 weeks.
- The product needs to be shaken periodically.
- Take the finished tincture 20 drops. 3 rubles/day for 30 min. before meals.
A folk remedy in the form of a medicinal ointment, which is prepared as follows, has also proven itself well:
- Combine 1 tsp. fresh honey and royal jelly.
- Mix the products well, then add 1 spoon of chilled boiled water to them and mix again until smooth.
- Take the resulting medicinal mixture into a new syringe without a needle and place it under the eyelid as an ophthalmic ointment.
- Carry out the procedure 2-3 times a day until the negative symptoms disappear.
Treatment
Treatment is carried out taking into account the individual characteristics of the disease and the individual patient.
First aid
Knowing what to do in an emergency can save valuable time and possibly prevent vision loss.
In all cases of visual contact with chemicals:
- Immediately flush the eye with water or any other drinkable liquid. Keep your eyes open as wide as possible while flushing. Rinse for at least 15 minutes.
- If the contact lens is in the eye, rinse the lens.
- Don't bandage your eyes.
- Seek emergency medical attention immediately after flushing.
For traumatic injuries:
- Apply a cold compress.
- Get emergency medical help if there is pain, blurred vision, or bleeding in the eye.
For cuts and punctures of the eye:
- Do not wash your eyes with water or any other liquid.
- Do not try to remove an object that is stuck in your eye yourself.
- Seek emergency medical attention immediately.
Drug therapy
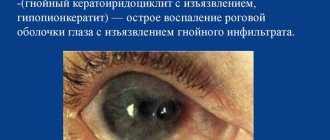
Infections are treated with medicated eye drops (antibiotics, antivirals, and antiparasitics) and, in some cases, oral medications. For example, herpetic stromal keratitis is a recurrent swelling that develops after a herpetic infection and is treated with anti-inflammatory steroid eye drops.
Folk remedies
Folk remedies are recommended to be used after consultation with a doctor, when the patient has already been diagnosed. At home, eye treatment with folk remedies can help in the fight against various ailments: dry eye syndrome; inflammatory processes; redness and swelling. Sea buckthorn oil quickly eliminates the symptoms of keratitis. Infusion of woodlice (chickweed) is instilled into the eyes when the cornea is clouded.
Surgical methods
If the cornea has been damaged, a corneal transplant, clinically known as keratoplasty, may be required. A corneal transplant can restore vision, reduce pain, and improve the appearance of a damaged cornea.
Diseases that require surgery:
- Keratoconus.
- Fuchs' dystrophy.
- Scarring on the cornea from infection or injury.
- Cloudiness of the cornea.
- Corneal edema.
- Corneal ulcer.
In addition, there is laser treatment. To treat some corneal pathologies, doctors may use a type of laser treatment called phototherapeutic keratectomy to reshape the cornea, remove scar tissue and make vision clearer.
Forecasts and methods of prevention
Early diagnosis and timely adequate treatment provide the most positive prognosis for successful recovery and return to work. Otherwise, a person risks completely losing his sight and remaining disabled for life. There are no specific preventive methods to prevent corneal degeneration. People with a genetic predisposition are advised to protect their visual organs from traumatic and irritating external factors, promptly treat various ophthalmological pathologies, and undergo preventive medical examinations by an ophthalmologist.
Prevention
The risk of corneal infections caused by bacteria and viruses can be reduced by protecting the eye from injury and limiting physical contact with people who have infectious forms of conjunctivitis.
Advice! Avoid sharing eye makeup, contact solution, lens cases, and eye drops with infected people. Wash your hands thoroughly with soap and warm water for at least 15 seconds after touching an infected person.
Useful video
Keratitis - causes, symptoms, treatment, inflammation of the cornea: