The cornea is made up of layers.
The epithelium covers a dense stroma.
The inside is lined with endothelium.
The cells of the inner layer are responsible for the outflow of eye fluid. The endothelium is not renewed. When damaged, moisture enters the following layers, creating swelling. Bubbles appear in the epithelium. The cornea becomes cloudy, becomes white, matte. The pathological condition is called endothelial-epithelial dystrophy (EDD), Fuchs' dystrophy, pseudophakic bullous keratopathy.
Causes
Austrian physician Ernst Fuchs first described EED in the early 20th century. He considered the cause of destruction of the endothelium to be a malnutrition, blood supply, and hormonal imbalance.
Endothelial degeneration occurs as a result of:
- hereditary genetic disorder;
- cataract extraction operations;
- injuries;
- chronic keratitis without treatment.
Primary dystrophy is caused by heredity. Secondary damage occurs due to disease and mechanical damage. But a prerequisite for the development of edema after operations and injuries is a genetic predisposition.
Types of dystrophies
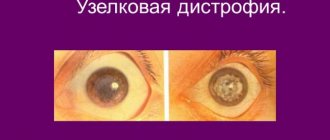
Depending on the location in the structure of the cornea, congenital damage to corneal dystrophy can be as follows:
- epithelial: epithelial basement membrane dystrophy, Meesmann juvenile epithelial dystrophy;
- stromal: cribriform, granular, crystalline Schneider, granular-cribriform Avellino, central cloudy Francois, spotted, posterior amorphous, pre-Descemet dystrophy;
- endothelial: posterior polymorphic, Fuchs dystrophy, congenital hereditary endothelial dystrophy;
- dystrophy of Bowman's membrane: Thiel-Behnke dystrophy, Reis-Boucler dystrophy.
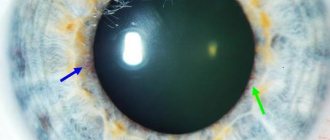
Fig. 2 Epithelial (anterior) corneal dystrophy (with outcome in neovascularization and opacification - cataract)
Although there are many types of corneal dystrophies, they all have similar symptoms and require similar treatment methods. Their main difference lies in the origin of each specific dystrophy in a specific human gene, which can only be determined by conducting complex genetic analysis. An ophthalmologist can determine some differences using a microscope.
Symptoms
The disease occurs without symptoms. Development from initial cellular changes to overt clinical manifestations can take 20 years.
Signs that appear during the course of the disease:
- vision in the morning is worse than in the evening;
- foreign body sensation;
- pain;
- sensitivity to light;
- hyperemia;
- lacrimation;
- swelling, clouding of the cornea;
- bull formation
Bubbles on the surface of the epithelium burst, causing severe pain.
Using confocal microscopy (CM), the state of the corneal endothelium was studied in 65 children aged 5 to 16 years (97 sick eyes) with uveitis of 1 month duration. up to 11 years during the period of disease activity and remission. A high frequency (80%) of changes in the corneal endothelium was found. Changes in the corneal endothelium were revealed, characteristic of the activity and remission of uveitis. The necessity of studying the corneal endothelium in children with uveitis using the CM method for the correction of drug therapy and when planning surgical interventions is substantiated.
In vivo confocal microscopy of corneal endothelium in children with endogenous uveitis
We examined 65 children aged from 5 to 16 years, 97 affected eyes. Using confocal microscopy (CM) we studied corneal endothelial in 65 children aged 5 to 16 years (97 affected eyes) with uveitis (prescription from 1 month to 11 years) in the periods of activity and remission. A high frequency (80%) of changes was found in the endothelium of the cornea. We revealed changes of the corneal endothelium typical to activity and remission of uveitis. We proved the necessity to study the corneal endothelium in children with uveitis by CM while planning surgery and to adjust medicamental treatment.
Changes in the corneal endothelium during endogenous uveitis in children can be associated either directly with the inflammatory process or be secondary in nature due to trophic disturbances due to hypotension, glaucoma, the formation of iridocorneal and lenscorneal adhesions, and postoperative epithelial-endothelial dystrophy. In this case, as a rule, the condition of the cornea is determined by the action of a complex of factors. Changes in the corneal endothelium, according to biomicroscopy, develop in 17-65% of children with anterior, peripheral and panuveitis, and their frequency and nature depend on the course, duration and etiology of uveitis [1, 2]. A thorough and objective examination of the state of the corneal endothelium is important for assessing the degree of activity of uveitis and determining treatment tactics, deciding on the possibility of intraocular correction, as well as determining the degree of influence of changes on visual functions.
Confocal microscopy (CM) is a unique non-contact technique that makes it possible to examine the cornea intravitally at the cellular level, assess the degree of morphological changes in cellular elements and extracellular structures, which makes it possible to judge the disruption of their function and the degree of damage to the cornea as a whole. This technique has not previously been used for uveitis in children. Only a few data have been published on the study of corneal precipitates with uveitis in adults using CM [3-6].
The purpose of our work was to assess the state of the corneal endothelium in endogenous uveitis in children using CM.
Material and methods
Using CM, the condition of the cornea was studied in 65 children aged 5 to 16 years (on average 10) with endogenous uveitis. The duration of the disease ranged from 1 month to 11 years. 97 diseased eyes were examined. At the time of the initial examination, active uveitis was observed in 52 cases and was accompanied by changes in the corneal endothelium (“fogging,” precipitates); remission—the absence of clinical signs of an inflammatory process lasting from 1 month with or without therapy—was noted in 45. CM was performed in 8 patients (13 diseased eyes) over time during the period of activity and remission of uveitis.
Analysis of the biomicroscopic picture showed that in 39 eyes the cornea was transparent, its marginal degeneration was detected in 28, band-like in 25. Aphakia after removal of complicated cataracts was in 18, pseudophakia in 18 cases. Secondary glaucoma was diagnosed in 25 eyes, of which 12 underwent antiglaucomatous operations. In 30 children, an association of uveitis with juvenile idiopathic arthritis was established, in 5 - with herpes group viruses, in 4 - with Vogt-Koyanagi-Harada syndrome, in 1 - with HLA-B27, in 1 - with Ilese disease, in 24 - the etiology of uveitis could not be established (Table 1).
Table 1.
Distribution of children by etiology of uveitis
| Etiology of uveitis | Number of children | Number of diseased eyes | ||
| abs. | % | abs. | % | |
| Rheumatoid | 30 | 45 | 44 | 45 |
| Herpes-associated | 5 | 8 | 8 | 8 |
| Vogt-Koyanagi-Harada syndrome | 4 | 6 | 6 | 6 |
| HLA-B27 associated | 1 | 2 | 1 | 1 |
| Eales disease | 1 | 2 | 2 | 2 |
| Unclear etiology | 24 | 37 | 36 | 37 |
| Total | 65 | 100 | 97 | 100 |
The study was carried out using a ConfoScan 4 confocal microscope from Nidek (Japan) with a magnification of 500. The method allows you to examine an area measuring 440 x 330 µm with layer-by-layer scanning of 5 µm. The design of the device makes it possible to study the central and paracentral areas of the cornea. Of particular value is the ability to determine endothelial cell density and morphometric parameters manually. Vidisic gel was used as an immersion liquid between the cornea and the optical lens of the microscope, and Alcain 0.5% drops were used for epibulbar anesthesia. The results of the study of endothelial cell density were compared with the regulatory framework of the device.
Results and discussion
When layer-by-layer analysis of corneal structures using CM, changes in the endothelium were found in 80% of eyes, somewhat more often during the period of activity (87%) than during remission of uveitis (71%) (Table 2).
Table 2.
Condition of the corneal endothelium in endogenous uveitis in children
| Signs | Activity (n=52) | Remission (n=45) | Total (n=97) | |||
| abs. | % | abs. | % | abs. | % | |
| Norm | 7 | 13 | 13 | 29 | 20 | 21 |
| Hyporeflective defects | 31 | 60* | 18 | 40* | 49 | 51 |
| Precipitates | 31 | 60ˇ | 16 | 36ˇ | 47 | 48 |
| Local hyperreflectivity with blurred cell boundaries | 20 | 38ʹ | 6 | 13 | 26 | 27 |
| Hyperreflective fibrin-like linear deposits | 11 | 21 | 6 | 13 | 17 | 18 |
| Focal cell traction | 14 | 14 | – | – | 14 | 14 |
| Expansion of intercellular spaces | 7 | 13 | 3 | 7 | 10 | 10 |
| Wave-like change in configuration in the frontal plane | 5 | 10 | 2 | 4 | 7 | 7 |
| Small hyperreflective inclusions | 7 | 13 | – | – | 7 | 7 |
| Diffuse cloud-like opacities | 8 | 8 | 1 | 1 | 9 | 9 |
Note. * ˇ ʹ — differences are significant, p<0.05
In half of the children, hyporeflective defects of endothelial cells were found (Fig. 1A), more often against the background of uveitis activity, and their number in the field of view increased with increasing activity of the inflammatory process. These changes are caused by cell apoptosis, which is accelerated by the action of inflammatory mediators on the endothelium.
Figure 1. Endothelial changes during uveitis activity
A - focal cell tractions, hyporeflective defects, local hyperreflectivity with blurred cell boundaries
B - precipitates with unclear boundaries
B - wave-like change in the configuration of the endothelium
As with biomicroscopy data, CM revealed precipitates in half of the examined patients, more often with active uveitis. It must be emphasized that with the help of CM, a more detailed assessment of their morphological features was possible. Active uveitis is characterized by voluminous precipitates with unclear boundaries and branched processes (Fig. 1B), while remission is characterized by clear boundaries of the bodies and processes of precipitates and their translucency (Fig. 2).
Figure 2. Endothelial changes during remission of uveitis. Semi-resorbed precipitates
Local hyperreflectivity with blurred cell boundaries—the CM equivalent of “sweating” of the endothelium—was most characteristic of active uveitis, and its degree correlated with the severity of the inflammatory process (Fig. 1A).
Expansion of intercellular spaces, wave-like changes in the configuration of the endothelium in the frontal plane (Fig. 1B), and diffuse cloud-like opacities were also more often observed during uveitis activity, and their severity depended on the severity of the inflammatory process. Focal cellular tractions (Fig. 1A) and small hyperreflective inclusions were detected only against the background of uveitis activity.
In all 60 non-operated eyes, the density of endothelial cells was within the age norm, however, in 55% of cases, pronounced (more than 33% of cells) polymegatism was found, in 30% - pleomorphism, which were more often observed in chronic and long-term inflammatory processes.
A decrease in endothelial cell density was observed in 5 of 18 (28%) eyes with pseudophakia and in 4 of 18 (22%) eyes with aphakia (by 2.3-14% and 0.3-19.7% of normal, respectively) with examination within a period of 1 month to 4 years after surgery. Unfortunately, a study of the density of endothelial cells before the intervention was not carried out in these patients, and the question of the effect of the volume of surgical intervention on the condition of the cornea in endogenous uveitis in children requires further targeted study.
Thus, assessing the condition of the corneal endothelium is an important component of the examination of patients with uveitis, and the use of the CM method allows for a quick, objective and ultrastructural study of it and assessment of the dynamics of changes.
Our first study of the corneal endothelium in children with endogenous uveitis using CM allowed us to detect a high frequency and wide range of changes not detected by biomicroscopy and establish their connection with the activity of the inflammatory process. It has been established that the activity of uveitis is associated with multiple changes in the endothelium: hyporeflective defects, precipitates with unclear boundaries and the presence of processes, local hyperreflectivity, fibrin-like deposits, focal cellular tractions, expansion of intercellular spaces, wave-like changes in configuration, cloud-like opacities. Despite the normal density of endothelial cells, pronounced polymegatism was found in half of the cases, pleomorphism was found in 1/3, which is caused by the death of endothelial cells and can subsequently lead to a decrease in cell density. Assessing the condition of the endothelium is also important when planning surgical interventions to decide the timing and prevent postoperative complications of the cornea.
conclusions
1. In 80% of children with endogenous uveitis and involvement of the anterior segment of the eye, changes in the corneal endothelium were detected, including against the background of remission of uveitis (71%).
2. Changes in the corneal endothelium characteristic of uveitis activity, not visualized biomicroscopically, were detected (hyporeflective defects, focal cellular tractions, local hyperreflectivity, unclear boundaries of precipitates and the presence of branched processes), which should be taken into account when determining the degree of uveitis activity.
3. A high frequency of polymegatism and pleomorphism of endothelial cells was discovered, due to their death during a frequently recurrent and prolonged inflammatory process, which can lead to a decrease in the density of endothelial cells.
4. Study of the corneal endothelium in children with endogenous uveitis using CM is necessary for the correction of drug therapy, as well as when choosing the timing of surgical intervention, deciding on the implantation of an intraocular lens after cataract extraction.
L.A. Katargina, Yu.P. Shestova, E.V. Denisova
Research Institute of GB named after. Helmholtz Ministry of Health of Russia, Moscow
Shestova Yulia Pavlovna – graduate student of the Department of Eye Pathology in Children
Literature:
1. Katargina L.A., Arkhipova L.T. Uveitis: pathogenetic and immunosuppressive therapy. - Tver: Triad, 2004. - 100 p.
2. Meshkova G.I. The value of modern methods of visualization and assessment of visual functions in the diagnosis and treatment of peripheral uveitis in children and adolescents: abstract of thesis. dis. ...cand. honey. Sci. - M., 2008. - 30 p.
3. Kanavi MR, Soheilian M, Yazdani S et al. Confocal scan features of keratic precipitates in Fuchs heterochromic iridocyclitis // Cornea. - 2010. - V. 29, N 1. - P. 39-42.
4. Mahendradas P, Shetty R, Narayana KM et al. In vivo confocal microscopy of keratic precipitates in infectious versus noninfectious uveitis // Ophthalmology. - 2010. - V. 117, N 2. - P. 373-380.
5. Mocan MC, Kadayifcilar S., Irkec M. Keratic precipitate morphology in uveitic syndromes including Behçet's disease as evaluated with in vivo confocal microscopy // Eye. - 2009. - V. 23. - P. 1221-1227.
6. Wertheim MS, Mathers WD, Planck SJ et al. In vivo confocal microscopy of keratic precipitates // Arch. Ophthalmol. - 2004. - V. 122, N 12. - P. 1773-1781.
Diagnostics
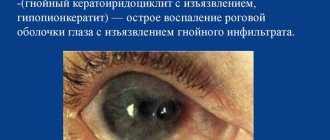
Upon external examination, clouding of the cornea is noticeable, which is sometimes accompanied by dilation of the conjunctival vessels. The diagnosis is confirmed using diagnostic procedures:
- Biomicroscopy. Signs of EED: lack of endothelial cells, swelling, bullous lesions of the epithelial layer.
- Pachymetry. By measuring the thickness of the cornea, the degree of swelling is assessed.
- Confocal microscopy. The method allows us to examine the structure of the endothelium, determine the density and size of its cells, and trace the dynamics of the destructive process. The guttas are also visible using the method. Specific drop-shaped formations are distinguished among endothelial cells by small dark cells with a light center. As the endothelial cells decrease, the gutta merge into large areas.
- Visometry in the morning and evening helps to indirectly determine the swelling inherent in EED and the degree of vision loss.
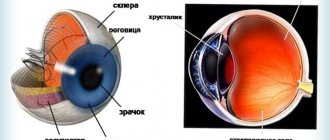
Structure of the cornea
The human cornea has five layers. The outer layer, consisting of 5-6 layers of cells, is the anterior epithelium, which performs a protective function. Beneath the anterior epithelium lies Bowman's membrane, a thin membrane of dense tissue that supports the outer layer.
Fig. 1 Structure of the human cornea
Under Bowman's membrane there is stroma (its volume accounts for up to 95% of the volume of the entire cornea). The stroma is made up of special cells - keratocytes, arranged in a strict order, which ensures the transparency of the cornea.
Recently, Duha's layer (discovered in 2013) has been distinguished in the cornea - a thin layer located between the stroma and Descemet's membrane.
The strongest tissue of the cornea adjacent to the stroma - Descemet's membrane - is a dense membrane that also performs a protective function.
The last layer is the endothelium (posterior epithelium of the cornea), which is a layer of one row of cells that perform the function of a “pump” - they control the flow of fluid into the cornea from the anterior chamber.
Treatment
Conservative therapy program:
- local administration of hypertonic saline solutions;
- the use of drops to improve trophism;
- applying eye ointments to promote healing;
- pain relief with analgesics in the form of drops or tablets;
- cross-linking procedure.
The saline solution traps and removes excess fluid from the tissues. Vision is corrected using optics - glasses, therapeutic contact lenses.
Bullous formations are eliminated using corneal cross-linking:
- The epithelium is removed from the cornea;
- apply riboflavin;
- irradiated with a special ultraviolet spectrum.
As a result, a new frame is formed on the cornea, preventing its deformation.
Surgical treatment - keratoplasty. Indications:
- severe degree of vision loss;
- thinning of the cornea;
- low endothelial density.
Types of keratoplasty:
- end-to-end - complete corneal transplantation;
- layer-by-layer DSEK - transplantation of Descemet's membrane with endothelium.
The damaged cornea is replaced with donor tissue and bioimplants. Layer keratoplasty is performed minimally invasively. The graft is inserted through a small incision, unfolded and fixed to the stroma with a stream of air.
Prevention of pathology
Of course, if your loved ones have corneal dystrophy, and it is inherited, it is difficult to do anything about it. But in other cases, eye tissue should be protected from injury, burns, foreign bodies, and toxic substances.
Be sure to use special safety glasses during construction and repair work and carefully observe hygiene rules when wearing contact lenses.
Useful video
Corneal dystrophy - what is it?