Neovascularization of the cornea occurs as a result of trauma, chemical damage, or ocular ischemia. It is the growth of the choroid plexus onto the outer membrane of the eyeball, which leads to disruption of the passage of sunlight into the pupil. This causes vision loss and changes in the appearance of the eye. The patient also experiences headache, dizziness and fatigue.
Treatment of the pathology consists of surgical laser therapy.
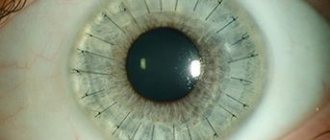
Corneal neovascularization
The proliferation of newly formed vessels is a pathology with a fairly wide distribution in practical ophthalmology. According to statistics, around the world, approximately 40 million people today need a corneal transplant due to complications of this disease. There is evidence that only 0.01% of endothelial cells are at the division stage. With chronic hypoxia, the existing indicator increases literally tens of times. At the same time, a persistent decrease in visual function is observed in 14.5% of patients and in 20-25% of patients there is a high risk of blindness. The incidence of the disease is the same for both males and females. The peculiarity of its geographical distribution has not been identified.
Corneal neovascularization - what is it?
Corneal neovascularization (or neoangiogenesis) is a pathological eye condition that ophthalmologists deal with quite often. With this pathology, blood vessels grow inside the cornea, which normally has a transparent structure and a smooth surface.
According to statistics, approximately 40 million patients in the world require a corneal transplant due to complicated neoangeonesis. The disease is dangerous because in 20-25 percent of cases it leads to complete blindness.
Neovascularization affects men and women equally. There can be many causes of the disease. Among them:
- Eye injuries. These can be burns, penetrating wounds or unsuccessful surgical interventions, as a result of which scar defects are formed, leading to the proliferation of blood vessels.
- Changes of a degenerative-dystrophic nature. This includes erosions, as well as ulcerative defects in the recurrent stage. Neoangiogenesis appears due to thickening of the layers of the cornea and the absence of normal trophism, as a consequence.
- Chronic keratitis. This disease is also a common cause of the appearance of newly formed vessels in the cornea of the eye. Due to long-term treatment, characteristic of keratitis and keratoconjunctivitis, oxygen starvation occurs, and as a result, neovascularization.
- Long-term wearing of contact optics. When using lenses, it is highly recommended not to exceed the permissible service life of the products. Otherwise, corneal hypoxia may occur, which subsequently leads to corresponding complications.
In ophthalmology, there are three main forms of neovascularization:
- Superficial (when the vessels, unchanged, are introduced into the cornea from the limbus area);
- Deep (vessels grow into the thickness of the cornea from the periphery to the center, both the middle and deep layers of the stroma are seriously damaged);
- Mixed (the pathological process affects the entire area of the membrane).
Often with neovascularization, hemorrhages occur in the area of the anterior chamber of the organs of vision. In the final stages of the lesion, a significant decrease in vision clarity may occur.
Method for treating newly formed vessels of the cornea
Laser coagulation of newly formed vessels of the cornea is performed. Laser radiation with a wavelength of 1.54 microns, energy of 130-145 mJ/cm2 and a laser spot diameter of 200 microns is used. The method ensures the restoration of corneal transparency and increased visual acuity.
The invention relates to the field of medicine, and more specifically to the field of ophthalmology, and can be used for the treatment of newly formed vessels of the cornea.
Diseases and damage to the cornea occupy a significant place in the pathology of the organ of vision (up to 30%). One of the reasons for decreased transparency of the cornea is its vascularization or the appearance of newly formed vessels. The reason for this may be wearing contact lenses, burn sores, trauma, penetrating wounds, inflammatory diseases of the cornea, including surgical interventions such as corneal transplantation and keratoprosthesis.
Among traumatic injuries to the eyeball, eye burns account for up to 39%, and 50% of victims become visually impaired. Despite powerful drug therapy, the issue of transparent engraftment of the graft after keratoplasty for a burn sore is extremely relevant. It is the abundant vascularization of the cornea, which causes bleeding during keratoplasty and complicates the course of the operation and postoperative course, that is one of the reasons for transplant opacity. Sometimes vascularization of the cornea occurs already in the postoperative period, 4-6 weeks after corneal transplantation in children and young patients, during repeated interventions or in combination with other operations on the eyeball. In this case, corneal vascularization serves as a poor prognostic sign - one of the manifestations of graft disease, when drug treatment cannot always stop its opacification.
Damage to the cornea during eyeball injuries is usually accompanied by a strong inflammatory reaction. Rehabilitation of patients with corneal injuries is very important, since inflammation rarely leads to clear healing of the cornea.
Currently, contact correction is very widespread throughout the world. The pericorneal tear film during contact lens wear differs in many ways from the intact tear film. With contact correction, the amount of total proteins, total lipids and sialic acids sharply increases, which can cause destruction of the tear film and the development of microbial infiltrative keratitis, aseptic infiltrative keratitis, dry eye syndrome and allergic conjunctivitis. All these complications in every 3 patients lead to pronounced vascularization of the limbus and in every 5 patients - to the ingrowth of blood vessels into the cornea. Long-term drug treatment with corticosteroids does not always eliminate blood vessels and repeated inflammation of the cornea. This forces patients to look for other ways to correct ametropia, and often this can only be spectacle correction, which does not always solve the patients’ professional problems. Many patients with ametropia who have worn contact lenses for a long time are denied keratorefractive surgery precisely because of vascularization of the cornea, which can cause serious complications during surgery and affect the refractive outcome.
Currently, a known method of combating corneal neovascularization is photochemical destruction of blood vessels (Kopaeva V.G., Andreev Yu.V., Ponomarev G.V., Stranadko E.F., Kopaev S.Yu. The first experience of photochemical destruction of blood vessels during neovascularization corneal transplant. Scientific works of the MNTK "Eye Microsurgery", issue 9. - Moscow, - 1998. - P.95-98.). The essence of this method is to fill the vessels with a chemical compound - a photosensitizer and its subsequent activation with light, which leads to the generation of cytotoxic singlet oxygen, which has a toxic effect on the vascular wall. However, the method is quite difficult to apply in practice in the case of local injection of a photosensitizer into a vessel due to, as a rule, the small diameter of the newly formed vessel and the great technical complexity of local injection of a photosensitizer under pressure into a small-diameter vessel, even in an operating room, while the neovascularized network of the cornea is filled only by 40%. The toxic effect of the drug affects the cornea and is manifested by swelling, which is relieved only on the 6th day after the start of treatment. In addition, administration of the drug both intravenously and locally, after introduction into the microcirculatory bed, has a toxic side effect not only on the iris and retina, but on the entire body, which greatly limits the widespread use of this method in practice.
Therefore, the search for effective methods for treating newly formed vessels of the cornea is very important.
The objective of the invention is to develop a safe and effective method for treating newly formed vessels of the cornea
The technical result of the invention is the elimination or reduction of newly formed vessels of the cornea, restoration of its transparency and increased visual acuity.
The technical result is achieved by the fact that in the method of treating newly formed vessels of the cornea according to the invention, laser coagulation of the newly formed vessels is carried out, exposing the cornea along the limbus to laser radiation with a wavelength of 1.54 μm, an energy of 130-145 mJ/cm2, and a laser spot diameter of 200 μm.
The treatment method according to the invention is carried out as follows.
Laser coagulation is performed using laser installations "LIK-100" or "Glasser", using radiation from an infrared laser on ytterbium-erbium glass with a wavelength of 1.54 microns, energy 130-145 mJ/cm2, pulse exposure 0.5-1, 0 ms, beam diameter 200 µm; in a non-contact manner, under local anesthesia. Working invisible radiation is directed to the cornea through a screen-printed radial-ring mesh along the aiming beam of a built-in low-power helium-neon laser.
The choice of this 1.54 µm laser source for the treatment of an eye patient with corneal vascularization depends on many circumstances. The therapeutic (surgical) effect of laser radiation appears only if it is absorbed by pathological tissues. This depends both on the wavelength of the radiation and on the composition and physical characteristics of the tissues being irradiated. An ytterbium-erbium laser with a wavelength of 1.54 microns, a radiation energy of 130-145 mJ/cm2 and a spot diameter of 200 microns makes it possible to obtain a coagulation effect strictly within the pathological focus and without damaging nearby intact layers of the cornea. This ensures not only radical treatment, but also implements the principle of the most gentle approach when carrying out laser treatment, which is especially important in the treatment of corneal diseases.
The choice of energy parameters and the amount of work performed on the Lik-100 and GlassEr installations is determined by the depth of the newly formed vessels in the corneal stroma and their volume. For their superficial localization, 130 mJ/cm2 and a coagulum diameter of 200 μm are used, and if they are located in deeper layers of the stroma, 140-145 mJ/cm2 with the same coagulum diameter are used. Only the corneal arteries are subjected to laser photocoagulation. In case of pronounced vascularization of the cornea, for the purpose of preoperative preparation for keratoplasty, coagulates are applied along the limbus in a continuous chain in order to reduce bleeding during surgery and to prevent possible subsequent vascularization of the graft. In the case of a small number of vessels, coagulation leads to blood stasis in them, followed by obliteration and desolation of the venous bed, usually after a single exposure. For extensive vascularized corneal cataracts, to reduce the degree of irritation of the eyeball, laser coagulation is usually performed in 2-3 sessions with intervals of 2-3 weeks between them.
The degree of eye irritation and the timing of epithelization were largely determined by the size and depth of the laser exposure. The short duration of thermal exposure on the cornea during surgery (0.5 ms) explains the low-traumatic nature of the procedure and contributes to the rapid completion of epithelization. On average, this process takes 3-5 days. As the inflammatory process subsides and epithelization is completed, the vascularization of the cornea decreases and visual acuity increases. Locally prescribed 0.25% chloramphenicol, 0.01% citral, 0.1% diclof 2-3 times a day for 10 days, then 0.1% descamethasone (prenacid) for 2-3 weeks according to the scheme: first week - 3 times a day, the second week - 2 times a day, the third week - 1 time a day.
There were not a single case of inflammatory or degenerative inflammation of the cornea, as well as damage to the deeper underlying media of the eye. The loss of PEC did not exceed 2%. The choice of laser treatment parameters was confirmed by experimental studies on donor eyes, electron microscopy results and computer analysis of the quantitative and qualitative state of corneal endothelial cells.
The present invention is illustrated by the following examples:
Example 1. Patient A., 70 years old. Diagnosis: OI - pseudophakia. OD - corneal opacification. OS - condition after penetrating keratoplasty, graft disease. There is a history of repeated inflammatory diseases of the cornea.
Visual acuity of the right eye is 0.3 uncorrectable, keratometry 52.25 x 10°, 43.87. PEC = 1500 cells/sq.mm. Visual acuity of the left eye is 0.05 sph + 3.75 cyl - 6.0 ax 32° = 0.1, keratometry 53.25 ax 32°, 40.87. PEC = 1900 cells/sq.mm. PEC = 1200 cells/sq.mm.
During the OD, the patient, under local anesthesia with a solution of dicaine, underwent non-contact laser coagulation of vessels along the limbus (in the clouding sector) with a radiation energy of 135 mJ/cm2 and a coagulum diameter of 200 μm. 2 rows of coagulates were applied. The distance between adjacent laser applications was at least one coagulum diameter.
During the OS, the patient, under local anesthesia with a solution of dicaine, underwent non-contact laser coagulation of vessels in 1-2 rows along the entire limbus with a radiation energy of 135-140 mJ/cm2 and a coagulum diameter of 200 μm.
After the operation, the eyes are moderately irritated, there is no pain, epithelization is completed within 3 days. At discharge, visual acuity OD was 0.4, visual acuity OS was 0.2. 6 months after the operation, visual acuity OD - 0.5-0.6 uncorrectable, keratometry 48.62 x 2°, 46.00, visual acuity OS - 0.2 uncorrectable, keratometry 53.00 x 146°, 43 ,52. PEC OI is unchanged, at the site of laser exposure, biomicroscopy reveals barely noticeable opacities, the graft on the OS has restored its transparency.
1 year after surgery, visual acuity of the OP remains the same. Biomicroscopically, barely pronounced opacities in the operation area are determined. The loss of PEC was no more than 0.5%.
Example 2. Patient M., 39 years old. Diagnosis: high degree of myopia, complex myopic astigmatism, wide limbus, partial vascularization of the cornea. The patient has a history of contact correction for 10 years and repeated inflammatory diseases of the cornea.
Visual acuity of the right eye 0.05 sph - 6.75 cyl - 2.5 ax 18° = 0.8; keratometry: 45.87 x 105°, 44.15, refractometry under conditions of cycloplegia sph - 7.00 cyl - 2.5 x 15°, endothelial cell density (ECD) = 2150 cells/sq.mm. Visual acuity of the left eye 0.02 sph - 6.5 cyl - 1.75 ax 188° = 0.9; keratometry: 46.15 x 95°, 44.75, refractometry under cycloplegia sph - 6.25 cyl - 2.0 x 180°, endothelial cell density (ECD) = 2100 cells/sq.mm.
The patient, under local anesthesia with a dicaine solution, underwent laser coagulation of newly formed arterioles along the limbus on the right and left eyes with a radiation energy of 135 mJ/cm2 and a coagulum diameter of 200 μm. The treatment was carried out in 2 sessions with an interval of 1 week between them. A total of 12 coagulates were applied on the right eye and 10 coagulates on the left eye. The distance between adjacent laser applications is at least one coagulum diameter.
After the operation, the eyes are practically calm, pinpoint coagulates with “ties” between them are biomicroscopically determined, there is no pain, epithelization is completed within 3-4 days.
At discharge, visual acuity of the right eye was 0.08 sph - 6.5 cyl - 2.5 ax 18° = 0.9; keratometry: 45.85 x 105°, 44.25, visual acuity of the left eye 0.05 sph - 6.5 cyl - 1.5 x 18° = 1.0; keratometry: 46.50 ax 105°, 44.55. PEC = no change. Biomicroscopy determines coagulates at the site of laser exposure and emptying of the corneal vessels. The patient was prescribed spectacle vision correction. 0.5 years after the operation, the visual acuity of the OP remains the same; barely pronounced opacities in the area of application of coagulates were biomicroscopically detected. The loss of PEC was 0%. A year after laser coagulation of the newly formed vessels of the cornea, after complete recovery, at the request of the patient, due to professional necessity and the impossibility of contact correction, refractive surgery was performed to eliminate myopia and astigmatism.
Example 3. Patient A., 28 years old. Diagnosis: OS - post-traumatic vascularized corneal opacification, complicated cataract. The patient is preparing for a corneal transplant with OS lens replacement.
Visual acuity of the right eye is 1.0. Visual acuity of the left eye is 0.02, uncorrectable, keratometry 47.05 x 89°, 38.25. PEC = 1900 cells/sq.mm.
The patient, under local anesthesia with a solution of dicaine, underwent non-contact laser coagulation of the corneal vessels along the limbus of the 2nd row with a radiation energy of 145 mJ/cm2 and a coagulum diameter of 200 μm. The distance between adjacent laser applications was at least one coagulum diameter.
After the operation, the eye is moderately irritated, there is no pain, epithelization is completed within 4 days. Upon discharge, visual acuity of the left eye is the same; coagulates and empty vessels of the cornea are biomicroscopically determined. The loss of PEC was 1%. 3 months after laser coagulation of the corneal vessels, the patient underwent penetrating keratoplasty with eye lens replacement and vitrectomy. There were no complications during the operation. The postoperative period was uneventful, the graft healing was transparent. At discharge, the visual acuity of the left eye was 0.3 uncorrectable, keratometry 48.75 x 78°, 43, 15. A year after the corneal transplant, the graft retains its transparency, and barely pronounced opacities are detected at the site of laser exposure at the limbus. The patient was prescribed spectacle vision correction.
Thus, the proposed method of treating newly formed vessels of the cornea using laser units “LIK-100” and “Glasser” with a wavelength of 1.54 microns is safe and effective. Laser coagulation using a wavelength of 1.54 μm provides a therapeutic effect with minimal trauma to the surrounding tissues of the cornea and a virtual absence of complications in the postoperative period, unlike the prototype. The use of the proposed method, both as an independent type of treatment and in preparation for surgery, contributes to the social and professional rehabilitation of patients.
A method for treating newly formed vessels of the cornea, including laser coagulation of newly formed vessels, characterized in that laser radiation with a wavelength of 1.54 microns, an energy of 130-145 mJ/cm2 and a laser spot diameter of 200 microns is used.
Treatment of corneal neovascularization
In the early stages, elimination of the etiological factor eliminates the progression of the disease or reduces the severity of clinical manifestations. Newly formed arterioles become empty and take on the appearance of barely noticeable “ghost vessels”. Conservative therapy is reduced to instillation of glucocorticosteroids into the conjunctival cavity or to parabulbar and subconjunctival administration. Surgical treatment is used for advanced forms and includes:
- Penetrating keratoplasty
. The technique is used when blood vessels grow into the cornea in a limited area. After removing the altered area of the cornea, donor material is sutured in its place. - Keratoprosthetics
. This is the method of choice in the treatment of patients with a deep form of neovascularization or with a complicated course of pathology due to the occurrence of a total vascular lesion. The keratoprosthesis is installed only 3 months after implantation of the support plate. - Laser coagulation of neovessels
. A step-by-step coagulation of endothelial channels and capillaries is carried out from the central part to the periphery. The technique is more effective for the superficial version of the disease. In the late postoperative period, recanalization of blood vessels is possible. - Photodynamic therapy
. The method is based on light-induced chemotherapy. The photosensitizer selectively accumulates in tissues with increased proliferative activity.
Causes
Many factors can lead to the development of this pathology. However, they all have common features, since increased neovascularization is a compensatory response of tissues to a lack of oxygen. Experts include the following as the main causes of excessive angiogenesis:
- Traumatic injuries. After eye injuries (wounds, burns) or ophthalmological operations involving the cornea, conjunctiva and limbus, rough scars often occur, leading to the proliferation of newly formed vessels.
- Chronic keratitis. Long-term inflammatory processes (keratitis, keratoconjunctivitis) are complicated by hypoxia of the eye membranes, which gives rise to the onset of neoangiogenesis.
- Degenerative and dystrophic changes. Numerous ulcerations and recurrent erosions become a stimulus for the occurrence of vascular proliferation, which is caused by thickening of the cornea and a lack of oxygen reaching the deep layers of the eye.
- Long-term use of contact lenses. Lenses become a mechanical barrier to the flow of oxygen. The appearance of the first symptoms of neovascularization is a signal for the patient to use lenses with high oxygen permeability, or better yet, to abandon them and use glasses.
Causes of corneal neovascularization
The development of this pathological condition can be associated with a number of reasons, including injuries and burns of the eyeball. Altered vessels are also formed in the corneal tissue as a result of severe inflammation, degenerative and dystrophic processes in this area. In addition, neovascularization is one of the postoperative complications and can also occur with uncontrolled and prolonged use of contact lenses.
With all these diseases, so-called tissue hypoxia occurs, which is accompanied by insufficient oxygen concentration. As a result, specific active substances are produced, which leads to the growth of new blood vessels. This reaction of the body is universal and occurs in response to damage. These altered vessels must provide the damaged tissue with oxygen and other necessary substances. In addition to the formation of new vasculature, connective tissue fibers (fibrous tissue) often grow in the corneal tissue, which leads to scar formation. Due to this, the recovery process in case of burn, injury or inflammation is accelerated, that is, the outcome of the injury becomes more favorable. However, against the background of the formation of a vascular network and scar tissue, a decrease in the transparency of the cornea is observed, that is, the acuity and quality of vision decreases. If the central zones are involved in the pathological process, then the risk of complete loss of vision increases.
Causes of pathology
There are quite a lot of factors that cause corneal neovascularization, among them, first of all, injuries and burns of the eye. At the same time, the appearance of newly formed vessels can provoke serious inflammatory and degenerative processes of the cornea, surgical interventions on the eyes and long-term wearing of contact lenses.
The process of neovascularization is triggered due to corneal hypoxia - lack of oxygen. Oxygen deficiency is a sufficient stimulus for the synthesis of specific substances that act as a growth factor for newly formed blood vessels. This reaction is universal and occurs in response to lesions leading to oxygen starvation of tissues in any part of the body. The task of the newly formed vessels is to provide oxygen and nutrition to the hypoxic area. Simultaneously with the newly formed vessels, dense fibrous tissue often grows into the cornea - a scar. Its appearance is very favorable during recovery from inflammatory processes, burns, injuries, because scarring helps the healing process, which means a favorable outcome of the disease.
However, with the cornea it is different. Its main quality is transparency, ensuring the unhindered passage of light rays. The growth of newly formed vessels and scar tissue seriously reduces the transparency of the cornea. This causes a deterioration in the quality of vision, and if the process of neovascularization affects the central zone of the cornea, a decrease in visual acuity can become fatal, including blindness.
Reasons for development
Neovascularization of the cornea can be provoked by the following factors on the human body:
- injury;
- burn;
- surgical intervention;
- exposure to toxic substances;
- chronic or long-term keratitis;
- disturbance of innervation;
- blockage of blood vessels supplying the eye;
- ischemia of the organ of vision;
- prolonged or improper wearing of contact lenses;
- cigarette smoke getting into the eye.
Over time, the disease leads to decreased or loss of vision.
The development of the disease is due to the fact that the cornea, which normally does not contain blood vessels and is nourished by the network supplying the limbus, becomes overgrown with arteries. This is due to prolonged ischemia of the membrane of the eye, which provokes proliferation and increased growth of endothelial cells and the germination of blood vessels over the pupil and all other structures. This leads to complete or partial loss of vision by the patient.
Pathogenesis
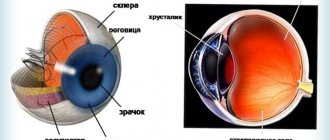
The cornea of the eye is the anterior convex membrane that does not have blood vessels. At the same time, blood supply and trophism are provided by the vascular network located in the limbus area. The trigger for the onset of the disease is local hypoxia, due to which the cornea is deprived of the required amount of oxygen. This causes increased production of nitric oxide, leading to the dilation of blood vessels between the sclera and cornea, as well as an increase in their permeability. Proliferation of endothelial cells is also promoted by activation of plasminogen and proteolytic degradation of the basement membrane. That is, corneal neovascularization occurs due to increased formation of endothelial cells, mobilization of smooth muscle cells and pericytes.
Causes of newly formed vessels
The number of reasons leading to corneal neovascularization is quite wide and includes, first of all, injuries and burns of the eye. In addition, inflammatory processes of the cornea (keratitis), as well as corneal dystrophy, can be factors leading to this condition. The development of neovascularization is also possible after surgical interventions or prolonged uncontrolled use of contact lenses.
The result of such effects is a deficiency of oxygen entering the cornea, with the development of tissue hypoxia. The state of hypoxia is a powerful stimulus for the body to produce specific substances that cause the growth of new blood vessels, designed to restore the supply of oxygen and nutrition to tissues. This reaction is a universal response to any damage. However, the newly formed vessels of the cornea begin to grow where anatomically they should not be, and besides, along with them, dense fibrous tissue resembling a scar grows on the cornea. Of course, such growth makes possible a speedy recovery from burns, injuries and inflammatory processes and the outcome of the disease itself becomes favorable. However, the main property of the cornea is its transparency, and with the formation of new vessels and the proliferation of fibrous tissue, its transparency is significantly reduced, which entails a decrease in the quality of vision, sometimes to its complete loss, when the central zone of the cornea is involved in the process.
Classification
From a clinical point of view, experts distinguish the following types of corneal disease:
- Superficial neovascularization . The vessels of the limbus pass into the cornea unchanged.
- Deep neovascularization . The vessels, directed from the periphery to the center, grow into the thickness of the cornea. In this case, the middle and deep stromal layers are affected. The vessels of the sclera and episclera look like parallel threads.
- Mixed neovascularization . The entire thickness of the membrane is involved in the process of neovascularization.
Signs of the disease
Excessive angiogenesis causes blood vessels to grow along the corneal surface, thereby impairing its transparency. The first stages of the disease are not accompanied by significant loss of visual acuity. A person loses it only when the process of neovascularization moves to the central zone of the cornea. When the visual field is narrowed, a disturbance in spatial perception occurs, accompanied by photopsia and metamorphopsia. With neovascularization of the cornea, patients, in most cases, note the appearance of dark spots or veils before the eyes, and complain of rapid eye fatigue during visual work.
If only one eye is involved in the neovascularization process, binocular vision is impaired. In mature patients, this causes a lot of difficulties, since if the optical part is damaged, it is almost impossible to adapt to monocular vision. Due to the incessant discomfort caused by interference in front of the eyes, headaches may begin. To reduce the degree of visual changes, some patients resort to the use of colored lenses, which further aggravates the symptoms. With long-term neovascularization, the radius of curvature of the cornea changes, it thickens, due to which the refractive index increases, and vision is distorted.
Corneal neovascularization: treatment, consequences - About vision
In normal condition, the cornea of the eye is transparent and has an absolutely smooth surface. With a pathology such as neovascularization, changes occur in the tissues of its membrane: newly formed vessels appear. In the article, we will look at why this condition is dangerous, and we will also figure out whether it can be treated.
Corneal neovascularization - what is it?
Corneal neovascularization (or neoangiogenesis) is a pathological eye condition that ophthalmologists deal with quite often. With this pathology, blood vessels grow inside the cornea, which normally has a transparent structure and a smooth surface.
According to statistics, approximately 40 million patients in the world require a corneal transplant due to complicated neoangeonesis. The disease is dangerous because in 20-25 percent of cases it leads to complete blindness.
Neovascularization affects men and women equally. There can be many causes of the disease. Among them:
- Eye injuries. These can be burns, penetrating wounds or unsuccessful surgical interventions, as a result of which scar defects are formed, leading to the proliferation of blood vessels.
- Changes of a degenerative-dystrophic nature. This includes erosions, as well as ulcerative defects in the recurrent stage. Neoangiogenesis appears due to thickening of the layers of the cornea and the absence of normal trophism, as a consequence.
- Chronic keratitis. This disease is also a common cause of the appearance of newly formed vessels in the cornea of the eye. Due to long-term treatment, characteristic of keratitis and keratoconjunctivitis, oxygen starvation occurs, and as a result, neovascularization.
- Long-term wearing of contact optics. When using lenses, it is highly recommended not to exceed the permissible service life of the products. Otherwise, corneal hypoxia may occur, which subsequently leads to corresponding complications.
In ophthalmology, there are three main forms of neovascularization:
- Superficial (when the vessels, unchanged, are introduced into the cornea from the limbus area);
- Deep (vessels grow into the thickness of the cornea from the periphery to the center, both the middle and deep layers of the stroma are seriously damaged);
- Mixed (the pathological process affects the entire area of the membrane).
Often with neovascularization, hemorrhages occur in the area of the anterior chamber of the organs of vision. In the final stages of the lesion, a significant decrease in vision clarity may occur.
What symptoms would indicate neovascularization of the cornea?
Neovascularization of the cornea, which is not treated promptly, can lead to complete blindness.
At the initial stages of development, the disease has practically no effect on refraction (vision, if it decreases, is insignificant, which is practically imperceptible).
However, the growth of blood vessels in the cornea can be visually determined by the correct symptom: the transparency of its surface begins to decrease.
At different time intervals, dark spots and veils may appear before the eyes. In this case, patients often note excessive fatigue, impaired binocular vision, headaches provoked by overexertion due to constant interference in front of the eyes.
As the pathology progresses, the patient experiences a narrowing of the visual fields, as well as difficulties with spatial perception.
Often, patients with neovascularization begin to use colored contact lenses to hide visible defects, completely covering the cornea and giving it a normal appearance.
However, the desire to hide aesthetic inaccuracies only aggravates the situation, since the oxygen and moisture permeability of such optics is reduced, which means that the cornea, which is already susceptible to hypoxia, suffers even more from a lack of trophism. This promotes the progression of neoangiogenesis.
Corneal neovascularization: treatment, drugs
The main task pursued by the attending physician who has identified neovascularization of the cornea in a patient at an early stage is to reduce the severity of the clinical manifestation of the disease and prevent its further progression. Classic conservative therapy involves instillation of glucocorticosteroids into the cornea and other drugs.
In other cases, treatment comes down to surgical methods. Depending on the characteristics of the disease, the following is prescribed:
- Penetrating keratoplasty. This method is effective if neoangiogenesis has affected a separate area of the cornea, which is removed during surgery and replaced with donor material.
- Laser coagulation. This technique has proven effective in cases where the disease is superficial.
- Keratoprosthetics. The treatment method is used in the late stages of neovascularization, in which a vascular eyesore appears.
- Photodynamic therapy. This method involves light-induced chemotherapy.
Neovascularization does not threaten the patient's life, but, depending on the degree of eye damage, the prognosis for visual functions can be very different. With timely diagnosis and correctly prescribed treatment, complete restoration of visual acuity can be achieved.
Compliance with safety rules as part of the work process in production, proper wearing of contact lenses - all this will help to avoid the risks of developing corneal neovascularization.
It is also important to visit an ophthalmologist at least once a year (this advice is especially relevant for people who regularly use contact lenses). This will help monitor eye condition and diagnose diseases in the early stages.
There are no specific measures to prevent this pathology.
On the Ochkov.Net website you can profitably buy contact correction products from the most popular brands. We advise you to pay attention to the products of Acuvue, Air Optix, Biofinity, etc.
Source:
Corneal neovascularization - treatment in Naro-Fominsk
A disease in which limbal blood vessels grow into the corneal stroma is called corneal neovascularization.
Among the signs of pathology, experts highlight: visualization of blood vessels in the form of “red branches” on the surface of the cornea, impaired binocular vision, a significant decrease in visual acuity, sometimes even to the point of blindness.
Confirmation of the diagnosis of “corneal neovascularization” requires eye biomicroscopy, visometry, keratometry, OCT or ultrasound of the eye.
In conservative treatment of the disease, drips of glucocorticosteroids are used into the conjunctival sac; it is also possible to administer them under the conjunctiva and parabulbarly. Surgical methods for treating the disease include: laser coagulation of newly formed vessels, photodynamic therapy, keratoprosthetics and keratoplasty.
Corneal neovascularization
The proliferation of newly formed vessels is a pathology with a fairly wide distribution in practical ophthalmology. According to statistics, around the world, approximately 40 million people today need a cornea transplant due to complications of this disease. There is evidence that only 0.01% of endothelial cells are at the division stage.
With chronic hypoxia, the existing indicator increases literally tens of times. At the same time, a persistent decrease in visual function is observed in 14.5% of patients and in 20-25% of patients there is a high risk of blindness. The incidence of the disease is the same for both males and females.
The peculiarity of its geographical distribution has not been identified.
Causes
Many factors can lead to the development of this pathology. However, they all have common features, since increased neovascularization is a compensatory response of tissues to a lack of oxygen. Experts include the following as the main causes of excessive angiogenesis:
- Traumatic injuries. After eye injuries (wounds, burns) or ophthalmological operations involving the cornea, conjunctiva and limbus, rough scars often occur, leading to the proliferation of newly formed vessels.
- Chronic keratitis. Long-term inflammatory processes (keratitis, keratoconjunctivitis) are complicated by hypoxia of the eye membranes, which gives rise to the onset of neoangiogenesis.
- Degenerative and dystrophic changes. Numerous ulcerations and recurrent erosions become a stimulus for the occurrence of vascular proliferation, which is caused by thickening of the cornea and a lack of oxygen reaching the deep layers of the eye.
- Long-term use of contact lenses. Lenses become a mechanical barrier to the flow of oxygen. The appearance of the first symptoms of neovascularization is a signal for the patient to use lenses with high oxygen permeability, or better yet, to abandon them and use glasses.
Pathogenesis
The cornea of the eye is the anterior convex membrane that does not have blood vessels. At the same time, blood supply and trophism are provided by the vascular network located in the limbus area. The trigger for the onset of the disease is local hypoxia, due to which the cornea is deprived of the required amount of oxygen.
This causes increased production of nitric oxide, leading to the dilation of blood vessels between the sclera and cornea, as well as an increase in their permeability. Proliferation of endothelial cells is also promoted by activation of plasminogen and proteolytic degradation of the basement membrane.
That is, corneal neovascularization occurs due to increased formation of endothelial cells, mobilization of smooth muscle cells and pericytes.
Classification
From a clinical point of view, experts distinguish the following types of corneal disease:
- Superficial neovascularization . The vessels of the limbus pass into the cornea unchanged.
- Deep neovascularization . The vessels, directed from the periphery to the center, grow into the thickness of the cornea. In this case, the middle and deep stromal layers are affected. The vessels of the sclera and episclera look like parallel threads.
- Mixed neovascularization . The entire thickness of the membrane is involved in the process of neovascularization.
Signs of the disease
Excessive angiogenesis causes blood vessels to grow along the corneal surface, thereby impairing its transparency. The first stages of the disease are not accompanied by significant loss of visual acuity.
A person loses it only when the process of neovascularization moves to the central zone of the cornea. When the visual field is narrowed, a disturbance in spatial perception occurs, accompanied by photopsia and metamorphopsia.
With neovascularization of the cornea, patients, in most cases, note the appearance of dark spots or veils before the eyes, and complain of rapid eye fatigue during visual work.
If only one eye is involved in the neovascularization process, binocular vision is impaired. In mature patients, this causes a lot of difficulties, since if the optical part is damaged, it is almost impossible to adapt to monocular vision.
Due to the ongoing discomfort caused by visual disturbances, headaches may begin. To reduce the degree of visual changes, some patients resort to the use of colored lenses, which further aggravates the symptoms.
With long-term neovascularization, the radius of curvature of the cornea changes, it thickens, due to which the refractive index increases, and vision is distorted.
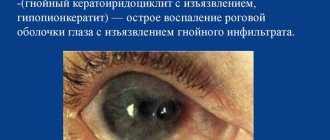
Possible complications
A particularly common complication of corneal neovascularization is total vascular opacity.
When it occurs, the normal color of the affected eye changes and the resulting cataract becomes the cause of blindness.
In addition, patients with corneal neovascularization are at risk for the occurrence of inflammatory and infectious processes in the ocular media (keratoconjunctivitis, keratitis).
Abnormal neovascularization is often accompanied by hemorrhages in the anterior chamber of the eye. In rare cases, hemophthalmos is observed. At advanced stages of the disease, polymegatism develops, with the occurrence of irreversible changes in the size and shape of endothelial cells.
What symptoms would indicate neovascularization of the cornea?
Neovascularization of the cornea, which is not treated promptly, can lead to complete blindness. At the initial stages of development, the disease has practically no effect on refraction (vision, if it decreases, is insignificant, which is practically imperceptible). However, the growth of blood vessels in the cornea can be visually determined by the correct symptom: the transparency of its surface begins to decrease.
At different time intervals, dark spots and veils may appear before the eyes. In this case, patients often note excessive fatigue, impaired binocular vision, headaches provoked by overexertion due to constant interference in front of the eyes.
Symptoms of corneal neovascularization
Increased angiogenesis leads to the proliferation of blood vessels on the surface of the cornea, which entails a decrease in its transparency. In the initial stages of the disease, visual acuity decreases slightly. If the process of neovascularization reaches the central zone, the patient completely loses vision. The narrowing of the visual fields is accompanied by a violation of spatial perception. Photopsia and metamorphopsia may occur. Patients with corneal neovascularization complain of the appearance of dark spots or “veils” before the eyes, and note increased fatigue when performing visual work.
Hemorrhoids kill the patient in 79% of cases
With a unilateral process, binocular vision is impaired. Adaptation to monocular vision with damage to the optic part is difficult in mature patients. Due to constant discomfort caused by interference in front of the eyes, headaches occur. Many patients use colored lenses to reduce the severity of visual changes, which further aggravates clinical symptoms. The long course of the disease leads to a change in the radius of curvature of the cornea, its thickening, which causes an increase in the refractive index and distortion of vision.
Possible complications
A particularly common complication of corneal neovascularization is total vascular opacity. When it occurs, the normal color of the affected eye changes and the resulting cataract becomes the cause of blindness. In addition, patients with corneal neovascularization are at risk for the occurrence of inflammatory and infectious processes in the ocular media (keratoconjunctivitis, keratitis).
Abnormal neovascularization is often accompanied by hemorrhages in the anterior chamber of the eye. In rare cases, hemophthalmos is observed. At advanced stages of the disease, polymegatism develops, with the occurrence of irreversible changes in the size and shape of endothelial cells.
Consequences
Overgrowth of blood vessels causes the development of a cataract in the patient.
In severe cases, vascularization of the cornea can cause complete vascular opacity. It leads to changes in the color of the eye, the appearance of a cataract, which causes insufficient light to reach the pupil and blindness. In addition, for patients suffering from this pathology, the risk of developing various inflammatory lesions of the cornea increases significantly. Increased angiogenesis increases the likelihood of hemorrhages and complete loss of vision for the patient.
Types of corneal opacities
Depending on the size and intensity of the turbidity, several main types of pathology are distinguished.
- Cloud (I degree of turbidity)
- a slight grayish turbidity with unclear boundaries.
The formation is almost indistinguishable; it is detected during examination with a slit lamp. A slit lamp
is an optical device that allows for microscopic analysis of the eyelids, conjunctiva, sclera, cornea, iris and lens. If the cloud is localized in the center of the cornea, then vision may decrease. - Spot (II degree of turbidity)
- white (gray) intense turbidity with clearly defined boundaries. The pathology is clearly visible without additional diagnostics. When located in the optical zone, it significantly impairs the acuity and quality of vision. - A cataract (III degree of turbidity)
is a white (gray, yellow) dense formation, in some cases accompanied by germination into the vessels. Cloudiness can occupy the entire surface of the cornea, leading to blindness.
Diagnostics
At the Vision Correction Center, only the most advanced, new diagnostic equipment is used to make a diagnosis of corneal neovascularization. The examination carried out includes:
- External inspection. It reveals visually detectable germination of newly formed vessels in the form of “red threads”.
- Visometry. This is a basic diagnostic method - determining visual acuity using special tables. Visual acuity can vary from a slight decrease to complete loss of visual functions, which is due to the degree of vascular proliferation.
- Biomicroscopy. The use of this technique is very informative for studying the transparency of the optical media of the organ of vision, identifying potentially possible processes of an inflammatory and dystrophic nature. With superficial neovascularization, it helps to identify blood flow in abnormal vessels.
- Keratometry. This procedure allows you to determine the radius of curvature of the cornea and examine its structural changes.
- Ultrasound (B-scan). The purpose of the study is to identify complications and secondary changes caused by the progression of the neovascularization process.
Diagnosis and treatment of corneal neovascularization
In the case when the vessels cover the central area of the cornea, the patient notes a deterioration in vision. In this case, sprouting vessels can be visually identified on the cornea in the form of red branches.
Timely initiation of treatment helps prevent the progression of neovascularization and pronounced changes in the cornea. Quite complex surgical techniques are used: keratoplasty (replacement of the surface layer of the cornea or its entire thickness with donor tissue), keratoprosthesis (removal of the cornea with replacement with a transparent lens). But after the operation there is still a risk of further vascular sprouting, because the intervention itself is a provocation of neovascularization. In order to empty the formed vessels, methods such as diathermocoagulation, laser coagulation, cryotherapy, photodynamic therapy can be used, that is, methods that disrupt the blood flow in the newly formed vessels of the cornea.
Treatment
When patients contact the Eye Clinic on Kurzenkova in the early stages of corneal neovascularization, specialists will help eliminate the etiological factor of the disease. This will reduce the severity of existing clinical manifestations and eliminate the possibility of progression of the pathological process. At the same time, the existing newly formed arterioles become empty, which become slightly noticeable “ghost vessels”. This is achieved by conservative therapy using drip glucocorticosteroids, which are instilled into the conjunctival cavity. In some cases, instillations are replaced/supplemented with parabulbar and subconjunctival steroid injections.
In advanced forms of the disease, patients of the Eye Clinic on Kurzenkova will be able to help with surgical treatment of the disease. To do this, we perform:
- Photodynamic therapy . This is a method of light-induced chemotherapy. The photosensitizing agent selectively accumulates in tissues that have increased proliferative activity.
- Laser coagulation of abnormal vessels . It is performed in stages, from the center to the periphery with coagulation of capillaries and endothelial channels. This technique is especially effective for the superficial form of the disease. In the delayed postoperative period, cases of vascular recanalization are known.
- Penetrating keratoplasty . Surgical intervention is recommended for patients with a limited area of vascular ingrowth into the cornea. It aims to remove the affected area of the cornea and replace it with a donor graft.
- Keratoprosthetics . This method is suitable for patients with deep neovascularization or when the pathology is complicated by the occurrence of a total vascular cataract. A special feature of the operation is that it is performed in two stages. The keratoprosthesis can be installed only three months after the installation of its support plate.
Treatment of vascularization
In the early stages, a course of conservative therapy is carried out. Hormonal drugs are prescribed into the conjunctival cavity.
At later stages of vascularization use:
- Laser coagulation of endothelial channels and capillaries in the direction from the central part to the periphery. A procedure for restoring vascular patency is indicated;
- Photodynamic therapy to introduce a photosensitizer into areas with abnormal proliferative activity;
- Keratoprosthetics for the treatment of individuals with complex forms of neovascularization;
- Penetrating keratoplasty when removing a damaged area of the cornea with suturing instead of donor material.
Our advantages
The Moscow Eye Clinic has world-class specialists specializing in the diagnosis and treatment of eye diseases. These include Professor Alexey Yuryevich Slonimsky and Sergey Alexandrovich Tsvetkov.
Our ophthalmology center offers its patients not only the possibility of laser coagulation of newly formed vessels of the cornea, but also high-tech penetrating keratoplasty. This treatment method is available in only a few clinics in Moscow. We have our own bank of corneal grafts and perform the operation without tedious waiting!
High-precision modern equipment from leading global manufacturers allows us to solve vision problems even in the most severe cases.
Prognosis and prevention
The prognosis for visual function with corneal neovascularization is directly related to the degree of disease and the intensity of vascular growth. Visual acuity can be fully restored only with timely treatment. This is very important, since there are still no specific preventive measures to prevent the disease.
Nonspecific forms of preventing corneal neovascularization include: compliance with safety precautions at work and at home (avoiding eye injuries), monitoring the duration of wearing contact lenses. In addition, patients using contact lenses are recommended to undergo an ophthalmological examination at least once a year to identify early signs of corneal neovascularization and timely, adequate treatment.
Prices for treatment for corneal neovascularization
The cost of treatment for neovascularization of the cornea at MGK is calculated individually and will depend on the volume of therapeutic and diagnostic procedures performed. You can find out the cost of a particular procedure by calling in Moscow 8 (499) 322-36-36
or online using the appropriate form on the website.
There are many reasons that can provoke the germination of blood vessels into the cornea. Most often, this pathology develops as a result of injuries, burns, inflammatory processes and degenerative diseases of the cornea. Neovascularization of the cornea can also occur after surgical interventions in this tissue, as well as uncontrolled long-term misuse.
All of these pathological processes lead to insufficient supply of oxygen and nutrients to the cornea. Hypoxia stimulates the production of substances that provoke angiogenesis. This is a universal protective reaction in the body, which ensures the restoration of damaged tissue in all organs. Newly formed vessels deliver trophic substances and oxygen to the tissue. But this process in the cornea reduces transparency. In addition, along with the vessels, dense fibrous tissue resembling scar tissue grows into the cornea. It is also a protective reaction that allows for faster recovery from injury. However, the decrease in corneal transparency caused by this fibrous tissue and the vessels themselves significantly impairs vision. If the central zone of the cornea is involved in the pathological process, complete loss of vision is possible.