With the help of laser vision correction, you can not only correct myopia, farsightedness and astigmatism, but also various pathologies of the cornea. One of the most common among them is its cloudiness. How to get rid of corneal clouding using laser vision correction?
In this article
- Why does corneal clouding occur?
- The use of laser in the treatment of corneal opacities
- Preparing the patient for surgery
- Step-by-step laser correction
- Rehabilitation period after corneal surgery
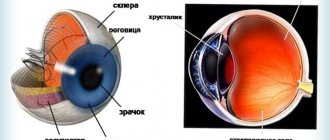
Clouding of the cornea often occurs against the background of untreated keratitis or is a consequence of dystrophy of various origins. Opacities are always accompanied by various types of ametropia, for example, myopia, farsightedness or astigmatism. This pathology of the cornea significantly interferes with high-quality vision correction, not only because of the clouding itself, but also due to the deterioration of light transmission. In addition, the cornea of the human eye loses its originally spherical shape, which also negatively affects the quality of vision.
Why does corneal clouding occur?
Cloudiness of the cornea of the eye can occur under various circumstances. The most common among them are:
- trauma or any physical damage to the cornea;
- damage to the cornea due to burns;
- damage to the cornea by a viral infection.
According to ophthalmologists, the risk of clouding increases significantly if the rules for using contact lenses are violated. For example, if you do not remove them before going to bed, the cornea will most likely become cloudy. The main symptoms of the disorder are: redness of the eyes, photophobia, increased production of tears. Objectively speaking, clouding of the cornea can be noticed by an ordinary person, and not just an ophthalmologist.
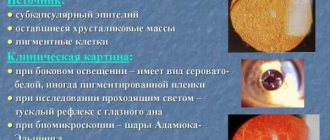
One of the varieties of pathology is a cataract, which is always white in color. As for the decrease in visual functions, they directly depend on the area of the damaged cornea of the eye. In any case, clouding of the eye cornea negatively affects vision.
Contraindications, what is prohibited to do
Unnecessary actions when injuring the cornea of the eye can lead to aggravation of the situation, and even greater damage can be caused to the eye.
Actions prohibited in case of injury to the cornea of the eye:
- Touching eyelids with hands;
- Using dirty bandages;
- Attempts to independently remove a foreign body that has entered the eye;
- Elimination of blood clots, since they can accidentally remove the fallen membranes;
- Use of alcohol tinctures - their use can lead to additional chemical damage;
- Ignoring the problem.
If the cornea is damaged, it is recommended to immediately call an ambulance and take first aid measures.
The use of laser in the treatment of corneal opacities
For the treatment of various corneal diseases, the PRK method (photorefractive keratectomy) is widely used today. This technology was first used in the mid-80s of the last century in Germany.
Today, this excimer technique is used to treat various types of pathologies of the cornea. During PRK, the laser, according to the “instructions” of the computer program, removes the damaged part of the cornea in just a few minutes. This is necessary for further therapeutic effects, including eliminating cloudiness of the eye, as well as increasing the strength of the upper layer of the cornea.
This can be achieved through the formation of a post-laser membrane. If the cloudiness cannot be completely eliminated with the help of PRK, as, for example, often happens when the eye is damaged by herpes viruses or adenovirus, as a result of which scars form on the cornea, then doctors can reduce its intensity.
Scratches and erosions of the cornea
This is one of the most common corneal injuries. Erosion appears due to mechanical damage to the epithelium, edematous, inflammatory and dystrophic changes.
Symptoms of corneal erosion:
- profuse lacrimation;
- photophobia;
- blepharospasm (uncontrolled contraction of the eye muscles);
- blisters or spots on the cornea.
Outpatient treatment of such corneal injuries is recommended. If the damage does not cause infection, the erosion heals quickly. Shallow erosions on the cornea can be cured with the help of anesthetic drops (Dicaine, Lidocaine, Inocaine), healing drugs (Solcoseryl, Actovegin, Korneregel, Emoxipin), antibiotic ointments, drops with hyaluronic acid and artificial tears. To prevent inflammation, sodium sulfacyl and Levomycetin are prescribed. As a rule, erosions disappear quickly and without consequences.
During corneal treatment, it is advisable to avoid animal fats and foods with cholesterol. It is better to stick to a diet with plenty of vegetables, fruits and berries.
Preparing the patient for surgery
The implementation of PRK is based on three main stages, including: the preparatory process, the operation itself and the rehabilitation period. The preparatory process for clouding of the eye cornea is not much different from preparation for any other type of operation; it includes tests and examinations. As a rule, this is blood biochemistry and fluorography. In addition, the patient will need to see a therapist, as well as specialists, such as an endocrinologist or rheumatologist.
Each of them will have to issue their own conclusion about the person’s health status and, accordingly, a referral for additional tests. Photorefractive keratectomy is not performed during periods of exacerbation of chronic diseases, as well as during acute respiratory viral infections and acute respiratory infections.
If the patient previously used lenses, then wearing them must be stopped seven days before surgery. If the ophthalmologist recommended hard lenses to him, then he will have to stop wearing them within two weeks. In order to avoid inflammation after corneal surgery, you should not paint your eyes, eyebrows, or use eye shadow on the day of laser correction.
Penetrating and non-penetrating corneal injuries
With non-penetrating wounds, the integrity of the inner membranes of the eyeball is preserved. Penetrating wounds are accompanied by the release of intraocular fluid and damage to the iris. In especially severe cases, loss of the lens and internal structures of the eye is noted.
Before visiting a doctor, you must instill antibacterial drops and apply a bandage. A severe penetrating wound provokes bleeding, but blood clots cannot be removed, because only they prevent the loss of the internal membranes.
In case of penetrating injury, blood loss must be minimized. If the foreign body is causing significant interference, you can carefully remove it and immediately apply pressure to the wound with a bandage. After this, the victim is immediately hospitalized.
The cut eye injury should be covered with a clean napkin and secured. The other eye should be covered to prevent movement of the eyeballs. In case of a blunt blow, apply a cold bandage or a cooled object.
In the hospital, the wound is treated and subsequent treatment is prescribed. Minor injuries can be treated conservatively, and sometimes the patient is prescribed contact lenses to seal the wound. Gaping wounds with torn edges require through or non-through sutures.
Penetrating injury to the cornea creates an additional danger to the visual system, so antibacterial and anti-inflammatory drugs are prescribed. Depending on the degree of damage, these drugs can be used locally, systemically, parabulbarly or subconjunctivally.
The duration of treatment for a corneal wound depends on the degree and size of the damage. Serious penetrating corneal wounds are treated surgically. Additionally, antibiotics, enzymes and healing drops are prescribed.
Possible complications of corneal injury:
- vitreous prolapse;
- retinal detachment;
- secondary glaucoma;
- cataract;
- hemophthalmos (bleeding into the vitreous body);
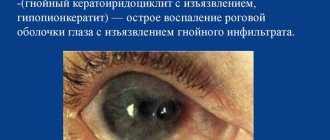
- panophthalmos (acute purulent inflammation of the entire eye);
- endophthalmos (recession of the eyeball);
- thorn.
The most severe complication of penetrating wounds of the cornea is considered to be fibrinoplastic iridocyclitis. This disease causes a sharp deterioration in vision in the healthy eye, therefore, if the damaged eyeball is blinded or there is light perception with incorrect light projection, it is recommended to remove the injured eye in a timely manner.
Step-by-step laser correction
Laser correction of corneal clouding is carried out in the following order.
At the very beginning, the anesthesiologist will drop special drops into the eyes. This method is called drip anesthesia. Next, a special eyelid dilator is installed on the eye whose cornea needs treatment, designed to prevent the patient from closing his eyes during surgery. After this, the doctor asks the patient to concentrate on the luminous point inside the device. If necessary, a special vacuum ring can be installed.
When all the necessary procedures are completed, the doctor removes that part of the corneal epithelium that caused the clouding of the eye. Then the surgeon uses a laser to shape the cornea with the necessary parameters. At the end of the operation, the surface of the eye is treated with a disinfectant, anti-inflammatory medications are instilled, and a temporary lens is installed. Wearing it helps protect the operated eye from external influences.
First aid, treatment
Corneal injuries are common among children and people whose profession is associated with a high risk of eye injury. Parents must be vigilant; compliance with safety regulations is considered primary prevention. If it was not possible to prevent injury, properly provided emergency care will help minimize the risk of complications. First of all, whenever possible, the severity of the problem should be established and the cause of its occurrence should be identified.
If you suspect the presence of a foreign object, you should try to remove it yourself; it is recommended to use clean water, cotton swabs or a handkerchief to wash your eyes. When removing crumbled objects, care must be taken; anti-inflammatory drugs should be instilled into the eyes; tetracycline ointment is prescribed when treating the lower eyelid. In case of primary necrosis, the affected area must be washed, and antibacterial treatment is also carried out.
In case of acute inflammatory process, detoxification and anti-inflammatory drugs, antioxidants, and multivitamins are used in therapy. For trophic disorders and vascularization pathologies, antihypoxic therapy is prescribed, and anti-inflammatory drugs are indicated.
The incised wound must be covered with a clean bandage, the other eye must be immobilized, which will help prevent simultaneous movements of the eyeballs. After this, the patient should be taken to the medical department as quickly as possible. After injury to the cornea with a blunt object, it is recommended to apply bandages pre-moistened in cool water.
A chemical burn should be washed with water, after which the substance that caused the damage is neutralized. Self-removal of metal and other particles from the eye is strictly prohibited. The duration of the recovery period and therapy depends on the nature and severity of the lesion. If a foreign object gets in, and if inflammatory processes develop, taking anesthetics is indicated. The use of ointments will ensure rapid restoration of damage to the membrane. In severe cases, surgery and postoperative treatment are required; the use of antibacterial agents will help prevent complications. The duration of the recovery period is 1-2 weeks, provided that you seek medical help in a timely manner.
Rehabilitation period after corneal surgery
Upon completion of treatment, special attention should be paid to the rehabilitation period.
At this time, you need to eat as many vitamins A and C as possible. Fatty meats, fried foods and alcoholic drinks are prohibited. In addition, it is worth reducing physical activity and not lifting heavy objects. You should also stop using decorative cosmetics. Following these simple recommendations will help restore the cornea.
Causes of peeling eyelids
The most common factors that can be used to explain why the skin on the eyelids peels are:
- allergies or irritation of the epidermis caused by the use of low-quality or expired eye cosmetics;
- seasonal allergies;
- age factor (so-called dry eye syndrome);
- respiratory diseases;
- dry skin;
- hard or chlorinated water;
- contact lenses that were not selected in accordance with all standards, or were stored incorrectly;
- too dry air in the room, where most often there is a person who experiences redness and peeling of the upper eyelid (one or both);
- eye fatigue;
- bad habit of constantly scratching your eyes;
- prolonged sitting at a computer screen;
- using aggressive products to wash or cleanse the skin of the face.
Etiology
Redness in the corners of the eyes on the outside can be caused either by simple fatigue or by some pathological processes, which can only be determined through examination and mandatory diagnostic measures.
In general, the manifestation of such a symptom may be due to the following etiological factors:
- severe fatigue.
- incorrectly selected glasses or contact lenses.
- allergic reactions.
- crack in the corner of the eye.
- inflammatory processes.
- ingrown hairs or abnormal eyelash growth.
- diseases of an ophthalmological nature.
- mechanical damage, cutting, piercing injuries.
- prolonged lacrimation.
- use of inappropriate eye drops, ointments and other medications that are intended for topical use.
It should also be noted that pain when blinking is most often caused by a foreign object or dust or dirt entering the organ of vision, which will be accompanied by the sensation of a hair in the eye. However, you should not try to eliminate this factor on your own, since such actions can only aggravate the situation.
The nature of the pathology will depend on what exactly caused the development of such a clinical sign. Only a specialist can correctly interpret the course of the clinical picture and compare it with a possible disease. You cannot do this on your own.
Eye skin care and hygiene
If the skin on your eyelids is peeling, causing itching, burning, discomfort and watery eyes, you can try to relieve the condition yourself. For this purpose, decoctions of medicinal plants are used that have antiseptic, soothing, anti-inflammatory and bactericidal properties. These herbs include:
- pharmaceutical camomile;
- calendula (marigold);
- series;
- St. John's wort;
- yarrow.
Healing decoctions are prepared from these herbs, which are then used to wipe the eyelids and skin around the eyes. There is nothing complicated in preparing such tonics.
Pour 1 spoon of raw material into 200-250 ml of boiling water and leave (or simmer for 7 minutes). Cool, squeeze out the pulp, filter. Use as directed 4-5 times a day.
Ordinary black tea helps perfectly in the fight against eye diseases (conjunctivitis, barley), in which the skin on the eyelids cracks and peels. Prepare the drink and let it cool to room temperature. Soak cotton wool or applicator in tea and rinse both eyes. A clean cotton swab should be used for each eye.
This manipulation needs to be done at least 5 times a day. Tea helps remove purulent discharge from the eyes due to conjunctivitis, relieves pain and burning in the eyes.
After complete elimination of eye pathologies, the use of decoctions of medicinal plants or tea leaves should be extended for a few more days in order to prevent relapses.
In addition, cucumber water for wiping the skin of the eyelids and around the eyes, as well as tar soap for periodic washing, are good eye hygiene products. Due to their beneficial properties, among which the antiseptic effect should be noted, these components perfectly combat eye fatigue and irritation. It is especially important to use them during the period when the air is literally filled with all kinds of allergens (in mid-spring, at the beginning and end of summer).
If all of the above methods of combating peeling of the eyelid skin are ineffective, be sure to consult an ophthalmologist. Such abnormalities, especially if they occur quite often, can cause serious harm to your health. Perhaps, after undergoing a thorough diagnosis, you will need drug treatment, which can only be prescribed by a qualified specialist!