Features of the anatomical structure of the cornea
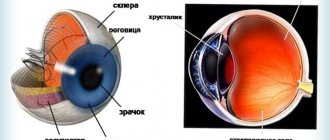
The outer shell of the visual apparatus consists of several layers:
- Epithelium. This is the upper “covering” of the eye, consisting of five or six rows of cells. Its main purpose is to protect the eye from damage and contamination. Has the property of rapid regeneration;
- Bowman's membrane. This is a dense and at the same time thin shell that supports the epithelial layer. Performs a support function;
- Stroma. It occupies the main part of the cornea. The stroma includes keratocytes arranged in a certain sequence. The element is responsible for the transparency of the cornea;
- Descemet's membrane. The densest layer that acts as a frame and prevents damage to the integrity of the structures of the organ of vision;
- The fifth layer includes modified epithelial cells responsible for the circulation of intraocular fluid between the anterior chamber of the eye and the cornea.
| Pathology usually damages the epithelium. There is also such a definition as recurrent erosion. It develops as a result of weak adhesion between the membrane and the surface layer. In this case, the slightest damage is enough for the epithelium to separate from the cornea. |
A little anatomy
The cornea of the eye consists of 5 layers. The protective function is performed by the outer layer (epithelium). This is followed by a thin membrane. Most of the cornea consists of stroma, thanks to the keratocytes present in it, the transparency of the outer layer is ensured. Between the outer and final layers (endothelium) there is Descemet's membrane or a dense membrane. The endothelium is responsible for regulating the influx and outflow of nutrients and fluids between the cornea and the anterior chamber of the eye.
Causes
Most often, the development of pathology is caused by the following factors:
- Penetration of a foreign object into the conjunctiva;
- Mechanical damage to the organ of vision. The integrity of the outer shell can be damaged by tree branches, pet claws, etc.;
- Chemical burn;
- Damage to the cornea as a result of improper use of contact lenses;
- Exposure to high temperatures;
- Effect of ultraviolet radiation;
- Dystrophic pathologies of the cornea;
- Surgical intervention on the visual apparatus;
- Neoplasms on the inner surface of the eyelid;
- Violation of eyelash growth. The anomaly develops against the background of demodicosis;
- Abnormal eye structure.
As you can see, almost all the reasons for the development of erosion indicate that the person himself is to blame for the appearance of the disease. Following basic safety rules and timely contact with an ophthalmologist will help you avoid problems with the cornea. Return to contents
Causes
The largest number of cases of keratitis is associated with viral etiology. In 70% of cases, the causative agents are herpes simplex and herpes zoster viruses (herpes zoster). Adenovirus infection, measles, and chickenpox can also provoke the development of keratitis, especially in children.
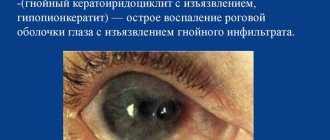
The next large group of keratitis consists of purulent lesions of the cornea caused by nonspecific bacterial flora (pneumococcus, streptococcus, staphylococcus, diplococcus, Pseudomonas aeruginosa, Escherichia coli, Klebsiella, Proteus) and specific pathogens of tuberculosis, salmonellosis, syphilis, malaria, brucellosis, chlamydia, gonorrhea , diphtheria etc.
A severe form of keratitis is caused by an amoebic infection - the Acanthamoeba bacterium; Amoebic keratitis often occurs in people who wear contact lenses and can result in blindness in the long term. The causative agents of mycotic keratitis (keratomycosis) are fusarium, aspergillus, and candida fungi.
Keratitis can be a manifestation of a local allergic reaction due to hay fever, the use of certain medications, helminthic infestation, hypersensitivity to food or pollen. Immune-inflammatory damage to the cornea can be observed in rheumatoid arthritis, polyarthritis nodosa, Sjogren's syndrome and other diseases. When the eyes are exposed to intense ultraviolet radiation, photokeratitis can develop.
In most cases, the occurrence of keratitis is preceded by mechanical, chemical, and thermal trauma to the cornea, including intraoperative damage to the cornea during eye surgery. Sometimes keratitis develops as a complication of lagophthalmos, inflammatory diseases of the eyelids (blepharitis), eye mucosa (conjunctivitis), lacrimal sac (dacryocystitis) and lacrimal canaliculi (canaliculitis), sebaceous glands of the eyelid (meibomitis). One of the common causes of keratitis is failure to comply with the rules for storing, disinfecting and using contact lenses.
Among the endogenous factors favoring the development of keratitis are exhaustion, lack of vitamins (A, B1, B2, C, etc.), a decrease in general and local immune reactivity, metabolic disorders (diabetes mellitus, a history of gout).
Pathomorphological changes in keratitis are characterized by swelling and infiltration of the corneal tissue. Infiltrates formed by polynuclear leukocytes, histiocytes, lymphoid and plasma cells have different sizes, shapes, colors, and unclear boundaries. At the stage of resolution of keratitis, neovascularization of the cornea occurs - the growth of newly formed vessels from the conjunctiva, the marginal looped network, or both sources into the membrane. On the one hand, vascularization helps to improve the trophism of the corneal tissue and accelerate recovery processes, on the other hand, the newly formed vessels subsequently become empty and reduce the transparency of the cornea.
In severe cases of keratitis, necrosis, microabscesses, and ulcerations of the cornea develop. Ulcerative defects in the cornea subsequently scar, forming a cataract (leukoma).
Types and classification
The disease is divided into several forms according to different characteristics:
- Depending on the size, erosion is classified into local and large-scale;
- By location. The pathology may be in the upper or lower part of the membrane;
- By the volume of damage (over all surfaces or affecting one layer);
- According to the duration of the disease (one-time or recurrent).
It is important to distinguish erosion from ulceration. In the first case, there is damage to the epithelium, which can recover on its own. With proper treatment, it does not leave scars and does not impair visual acuity. With an ulcer, recovery does not occur; after the “sore” heals, seals remain on the outer shell.
Corneal erosion is also divided into two forms depending on the cause of the disease.
Recurrent
With such a disease, unpleasant symptoms return over and over again, despite the course of therapy. There are two types of pathology: diffuse (the damage affects the main part of the mucosa) and local (the damage develops in a specific area).
A recurrent anomaly occurs for the following reasons:
- When the conjunctiva is injured, the basal cells responsible for the process of tissue regeneration are affected. As a result of pathology of the cornea, defective cells are formed on its surface, they shrink and expose the lower layers;
- Pathological processes are activated due to inflammation occurring on the outer shell.
The main symptoms of the disease: pain, burning, increased lacrimation.
| The main goal of therapy is to restore the integrity of the basal layer. For this, doctors prescribe fortified ointments that normalize metabolism. Antibacterial medications are used to prevent the cornea from drying out. |
Traumatic erosion
In most cases, the integrity of the membrane is compromised as a result of mechanical impact on the organ of vision. The smooth epithelial layer is damaged when a foreign object penetrates the eye or when contact lenses are used incorrectly. Pathology can also manifest itself due to severe wounds affecting the mucous membrane.
Traumatic erosion is diagnosed when the eye is burned by chemicals or toxins. The disease appears as a result of exposure to high temperatures on the visual apparatus. The integrity of the cornea can be damaged by regular friction of the cilia on the mucous membrane as a result of their improper growth or inversion of the eyelids.
The main symptoms of the disease:
- Painful sensations;
- Photophobia;
- Redness of the conjunctiva;
- Increased lacrimation;
- Feeling of the presence of a foreign object;
- Damage to the central part of the cornea leads to a decrease in visual acuity.
Eye drops and antibacterial medications are used to treat the disease. Return to contents
Traumatic erosion
Most often, the integrity of the cornea is damaged due to rough mechanical impact. The smooth epithelium is injured due to foreign particles entering the eye or a person violating the rules for using contact lenses. Traumatic erosion sometimes occurs due to extensive wounds to the ocular mucosa.
Traumatic erosion of the cornea of the eye occurs due to damage to the cornea by chemical or toxic substances. Thermal burns can also cause traumatic erosion.
Violation of the integrity of the membrane often occurs due to constant friction of the eyelashes against the mucous membrane of the eye due to inversion of the eyelids (entropion).
The main symptoms of the disease: pain, sensation of a foreign body, hypersensitivity to light, redness of the mucous membrane. Increased lacrimation occurs when the cornea is damaged. If the erosion is located in the center of the mucosa, then the patient’s visual acuity decreases.
To treat traumatic erosion, eye ointments and keratoprotective drops, as well as antibacterial drugs, are used.
Consequences of corneal erosion
In some cases, the disease can lead to the development of serious complications. Most often, negative consequences occur in the complete absence of treatment or incorrectly selected therapy. The risk of encountering severe vision problems also increases, provided that the patient consults a doctor when the disease has reached a severe form.
The main danger of corneal erosion is neovascularization of the outer membrane. The anomaly progresses as pathogenic microorganisms penetrate the damaged area. As a result, neoplasms in the form of new vessels form on the cornea. Since such tissues transform into scars over time, there is a high risk of complete loss of vision. Destructive processes can be stopped only at the initial stage, when the cornea has not yet become cloudy.
| The worst scenario for the development of the disease is the formation of a cataract. You can get rid of it only through surgery, during which the damaged cornea is transplanted. |
Recurrent erosion
With recurrent corneal erosion, the mucosal defect occurs again and again, despite the therapy. There are 2 types of disease: diffuse (a large area of the mucous membrane is damaged) and local (the affected area is limited).
Recurrent erosion occurs for the following reasons:
- At the time of injury to the eye mucosa, the basal cells, which regulate epithelial renewal processes, were damaged. As a result of a pathological change in the cornea, defective cells appear on its surface, which shrink and expose the lower layers;
- Dystrophic changes due to the inflammatory process on the cornea.
Symptoms of recurrent erosion: pain, burning in the eyeball, sensation of a foreign body, excessive secretion of tear fluid.
The main goal of treating recurrent corneal erosion is to restore the basal layer of the epithelium. For this, vitamin ointments are used, which improve metabolic processes and regenerate the epithelial layer. Antibacterial drugs are used to prevent drying out of the cornea and protect nerve endings.
Symptoms
The development of pathology is indicated by the appearance of the following signs:
- Pain in the organ of vision where the cornea is damaged. They intensify when blinking;
- Intolerance to bright light;
- Severe and uncontrollable lacrimation, which appears due to irritation of damaged nerve endings;
- With secondary infection, purulent exudate is observed;
- Decrease in visual acuity. A similar symptom occurs if the central part of the membrane is affected or the pathology is of an impressive size;
- Redness of the conjunctiva. In some cases, it signals the onset of inflammatory processes that arise due to the addition of a secondary infection;
- Some patients complain of a feeling as if sand had been poured into their eyes. This indicates that the mucous membrane is involved in the destructive process.
Microscopic damage to the cornea heals on its own, since the epithelium has the ability to regenerate. However, it is not recommended to ignore dangerous symptoms and it is better to seek professional help.
Eed cornea code according to ICD 10
If it is necessary to identify the drug that caused the lesion, use an additional external cause code (class XX).
Excludes: keratopathy (bullous aphakic) after cataract surgery (H59.0)
Descemet's membrane fold
Descemet's membrane rupture
Dystrophy:
- cornea: epithelial
- granular
- lattice
- spotted
Excludes: congenital malformations of the cornea (Q13.3-Q13.4)
Recurrent corneal erosion
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
source
RCHD (Republican Center for Health Development of the Ministry of Health of the Republic of Kazakhstan) Version: Clinical protocols of the Ministry of Health of the Republic of Kazakhstan - 2017
Bullous keratopathy or endothelial-epithelial dystrophy is a polyetiological disease associated with the loss of endothelial cells 1.
The disease is characterized by the development of chronic edema of the cornea with subsequent disruption of its trophism, the formation of persistent opacities, decreased visual acuity, the development of debilitating pain syndrome, and often ends in functional and anatomical death of the eye 7.
In the CIS countries, the terms “secondary EED” and “bullous keratopathy” are used as equals, while in the English-language literature, secondary EED is usually called bullous keratopathy, and primary EED is called Fuchs’ dystrophy [9,10].
In 80% of cases, EED is iatrogenic in nature, associated with previous surgery with opening of the eyeball and, most often, cataract surgery [4,5,8].
ICD-10 and 9 code(s):
| ICD-10 | ICD-9 | ||
| Code | Name | Code | Name |
| H 18.1 | Bullous keratopathy | 11.7101 | Phototherapeutic keratectomy |
| H 18.2 | Other corneal edema | 11.4901 | Crosslinking of corneal collagen |
| H 18.3 | Changes in the membranes of the cornea | 11.62 | Other types of lamellar keratoplasty |
| H 18.4 | Corneal degeneration | 11.64 | Other types of penetrating keratoplasty |
Date of protocol development/revision: 2017.
Abbreviations used in the protocol:
| BC | – | bullous keratopathy |
| IOL | – | intraocular lens |
| MKL | – | soft contact lens |
| ARVI | – | acute respiratory viral infection |
| UPC | – | penetrating keratoplasty |
| Ultrasound | – | ultrasonography |
| FTC | – | phototherapeutic keratectomy |
| EFI | – | electrophysiological studies |
| EED | – | endothelial-epithelial dystrophy |
Protocol users : ophthalmologists, general practitioners.
Patient category : adults.
Level of evidence scale:
| A | A high-quality meta-analysis, systematic review of RCTs, or large RCTs with a very low probability (++) of bias, the results of which can be generalized to an appropriate population. |
| IN | High-quality (++) systematic review of cohort or case-control studies, or High-quality (++) cohort or case-control studies with very low risk of bias, or RCTs with low (+) risk of bias, the results of which can be generalized to an appropriate population . |
| WITH | Cohort or case-control study or controlled trial without randomization with low risk of bias (+). The results of which can be generalized to the relevant population or RCTs with very low or low risk of bias (++ or +), the results of which cannot be directly generalized to the relevant population. |
| D | Case series or uncontrolled study or expert opinion. |
| GPP | Best clinical practice. |
| Stages | Clinical characteristics |
| Risk group | The cornea is transparent, its thickness is normal, the density of endothelial cells is 320-510 cells/mm2 |
| I | The transparency of the cornea is locally reduced, its thickness is locally increased to 0.7 mm, the density of endothelial cells is uneven |
| II | Moderate decrease in transparency, thickness 0.7-0.8 mm, cell contours are blurred, endothelial cell density is low, endothelium covers the entire surface of the cornea, but the cells are sharply enlarged |
| III | Significant decrease in corneal transparency, average thickness 0.82 mm, endothelial cells contact through processes, endothelial microscopy is impossible |
| IV | The transparency of the cornea is significantly reduced, its thickness is 0.97 mm, separate groups of enlarged endothelial cells are determined, endothelial microscopy is impossible |
| V | A sharp decrease in the transparency of the cornea, its thickness is more than 1.15 mm, endothelial cells are single, endothelial microscopy is impossible |
| Stage | Complaints | Visual acuity | Cornea condition | Condition of the iris | Complications | Recommended Treatment Methods |
| I | Inconsequential and impermanent | Not changed | Intermittent local swelling of the endothelium, respectively, single folds of the DM | Not changed | No | Conservative therapy Laser therapy Cryotherapy |
| II | Intermittent foreign body sensation, occasional redness | Changes | Persistent local swelling of the endothelium against the background of diffuse sweating and sputtering of pigment, folds of the DM, local swelling of the posterior layers of the stroma, unstable local swelling of the epithelium | Somewhat edematous | Phenomena of iritis, pigment on the anterior capsule of the lens | Soft contact lenses, conservative therapy, laser therapy, cryotherapy, surgical treatment (synechiotomy, keratoplasty) |
| III | Constant lacrimation, photophobia, inflammation, pain, often stabbing | Reduced | Diffuse edema of the endothelium, deposition of pigment on it, pronounced folding of the DM, diffuse edema of the stroma, persistent bullous edema of the epithelium | Edema, rigid, isolated newly formed vessels, posterior synechiae | Iridocyclitis | Keratoplasty |
| IV | Severe photophobia, lacrimation, inflammation and pain in the eye, headache | Sharply reduced | Severe swelling of all layers, deposition of pigment and exudate on the endothelium, pronounced folding of the DM and stromal edema, bullous edema of the epithelium with erosions, focal infiltration, ulceration, vascular ingrowth | Edema, newly formed vessels, posterior synechiae, pupillary exudative film | Severe iridocyclitis, lens opacification, retrocorneal film | Keratoplasty Biological coating |
| V | Eyeball irritation, constant eye pain, headache | Reduced to light perception | Vascular opacity of the cornea of uneven density - replacement of all layers of the cornea with scar vascular tissue with focal ulcerations | Sub- or atrophic, posterior synechiae, pupillary fusion, obliteration of the anterior chamber angle | Secondary glaucoma | Keratoplasty Keratoprosthetics |
DIAGNOSTIC METHODS, APPROACHES AND PROCEDURES
Complaints: · decreased/lack of vision; · pain; · lacrimation; photophobia;
· sensation of a foreign body, “sand” under the eyelids.
History: · previous surgical/laser intervention; · previous trauma; · previous severe intraocular purulent-inflammatory process;
· previous chronic recurrent intraocular inflammatory processes
Physical examinations: none.
Laboratory tests: no.
Instrumental studies: Visometry: · low visual acuity/no vision, with ineffective optical correction;
· depending on the stage and degree of endothelial damage, visual acuity is from 0.1-0.3 to light projection.
Biomicroscopy : · there is no discharge in the conjunctival cavity; · presence of postoperative scars on the conjunctiva/cornea; · cornea swollen locally/diffusely; epithelium is dull/loose/edematous; · complete epithelization/point defects/local defects/bullas/erosions; · Descemet's membrane folds are single/tender/rough/all over. · anterior chamber medium/deep/shallow/uneven/iridocorneal fusion – localization. · transparent moisture/vitreous fibrils · round/deformed pupil; synechia/photoreaction live/preserved/sluggish/absent; drug-induced/paralytic mydriasis · lens* transparent/cloudy; IOL – posterior chamber / anterior chamber; correct position/dislocation/capture of IOL · vitreous* transparent/opacities/destruction/hema/avitria/silicone · fundus* visualized/not visualized, reflex pink/gray
· *with severe swelling/clouding of the cornea in the central zone – visualization is impossible
Tonometry: · intraocular pressure is within normal limits / increased with concomitant glaucoma.
Ultrasound:
· absence of its own lens/presence of an IOL in the posterior/anterior chamber; · silicone in the vitreal cavity/anterior chamber;
Vitreous destruction/retinal detachment
Keratopachymetry : · presence of local/diffuse corneal edema; from 600 to 1500 microns in the central zone.
Treatment and diagnostic algorithm:
| Diagnosis | Justification for differential diagnostics | Surveys | Diagnosis exclusion criteria |
| primary Fuchs keratopathy | corneal edema | 1. biomicroscopy - diffuse, pronounced edema, bullae / erosions 2. Ultrasound - without visible pathology and consequences of previous operations / injuries 2. Keratopachymetry - pronounced local/diffuse edema of the cornea over 1000 microns in the central, sub-central zone. | 1. There is no indication in the medical history of previous surgical interventions, injuries, acute/chronic intraocular inflammatory processes; 2. The process is always two-way; 3. Genetic predisposition. |
| keratitis | corneal edema | 1. biomicroscopy – swelling is often local, moderate; inflammatory infiltrate, preserved epithelium / de-epithelialization in the infiltrate zone 2. Ultrasound - no visible pathology and consequences of previous operations / injuries 2. Keratopachymetry - mild corneal edema, less than 800/1000 µn in the central / sub-central zone. Perhaps, on the contrary, local thinning. | 1. History indicates previous microtrauma, burn, wearing SCL, poor hygiene, infection, acute respiratory viral infection, etc.; there are no indications of previous surgical interventions. 2. The process is often one-sided; 3. There is no genetic predisposition |
Get advice on medical tourism
Get advice on medical tourism
| Atropine |
| Brimonidine |
| Brinzolamide |
| Sodium hyaluronate |
| Dexamethasone |
| Dexpanthenol |
| Dextrose |
| Levofloxacin |
| Proxymetacaine |
| Riboflavin |
| Sulfacetamide |
| Timolol |
| Tramadol |
| Tropicamide |
| Phenylephrine |
TREATMENT TACTICS AT THE OUTPATIENT LEVEL: · drug therapy: keratoprotective, prevention of secondary infection. With the development of secondary infection - instillation of antibiotics, with an increase in IOP - instillation of antihypertensive drugs. · SCL for the purpose of epithelization of the cornea.
· physical treatment to relieve corneal edema.
Source: https://ckmosstroy.ru/eed-rogovitsy-kod-po-mkb-10/
Diagnostics
In some cases, the disease can be identified during the initial examination. For example, in case of mechanical damage or the presence of a foreign object in the eye. During the examination, the ophthalmologist always turns out the upper and lower eyelids in order to conduct a detailed analysis of the state of the visual apparatus and identify neoplasms on the mucous membrane.
To confirm the diagnosis, biomicroscopy is prescribed. It allows you to determine the size of the damage and the condition of the tear film. If the anomaly has small parameters, then it can only be detected using the unique fluorescein dye.
| If the patient wears contact lenses, the ophthalmologist examines them under a microscope. Since violation of the integrity of the eyepieces can cause damage to the outer shell. |
Return to contents
How is diagnostics carried out?
If there is any suspicion of damage to the cornea, you should immediately contact an ophthalmologist. The doctor will listen carefully to the complaints and ask additional questions to clarify the cause of the lesion. Then a detailed eye examination is performed using instruments. This allows you to detect foreign objects in the eye, see changes in the mucous membrane and determine the nature of the fluid released (purulent or mucous).
Then, biomicroscopy of the eye is performed - examination of the surface of the cornea with a high-magnification device, identifying the slightest surface defects. This helps to identify erosion, its size and the depth of tissue damage.
If signs of erosion are visible, but the lesion is not detected due to the fact that it is small, fluorescein is used - a dye that highlights the defect. Additionally, various methods for measuring intraocular pressure, ultrasound to detect pathologies inside the eyeball or ophthalmoscopy, smears for cytology and cultures are used.
Treatment of corneal erosion
To speed up the healing process of the affected layer, it is necessary to take keratoprotectors. This is a group of medications that restores the integrity of the membrane and strengthens it. These include:
- "Kerakol". Accelerates the process of epithelial regeneration, maintains the level of transparency of the outer shell and strengthens blood vessels;
- "Dakrolux". Moisturizes the surface of the visual apparatus, normalizes the refractive properties of the eye. Eliminates symptoms of inflammation of the conjunctiva;
- "Visit." Forms a protective film on the surface of the cornea that protects it from drying out. Minimizes the risk of swelling and inflammation.
To eliminate erosion, moisturizing eye drops must be prescribed:
- "Systane" It is used three times a day, two drops in each eye. When performing this procedure, make sure that the tip of the pipette remains clean. Allowed for use in patients wearing contact lenses;
- "Oxyal". Twice a day, a couple of drops in each eye. It is prohibited to use simultaneously with other medications of similar effect. An opened bottle is stored for a maximum of sixty days;
- "Vidisik." Injected into the damaged eye three times a day. During the period of use, you should avoid contact lenses;
- "Ophtagel". Apply one drop two to four times a day, depending on the severity of the disease. Use with caution in pregnant women. Contact lenses can be put on only half an hour after the procedure.
The doctor also prescribes antibacterial drugs (Tobrex, Floxal, etc.) to eliminate the risk of infection. The course of treatment lasts from ten days to two weeks.
Surgical therapy
If treatment with medications does not bring results, the doctor prescribes surgery. During keratoplasty, Bowman's membrane is affected and the damaged layer of epithelium is removed using an excimer laser unit.
Erosion can cause clouding of the cornea, which, if left untreated, leads to blindness. Pathology goes through several stages:
- Cloud. A slight clouding of a gray tint, which is not noticeable upon visual inspection;
- Spot. It is clearly visible even with the naked eye. When the anomaly is concentrated in the center of the cornea, a drop in visual acuity is observed;
- Belmo. The outer shell becomes completely or partially matte, visually reminiscent of porcelain glass.
During surgery, the cloudy cornea is removed and replaced with a donor implant. In some cases, a similar procedure is carried out for cosmetic purposes, since spots on the eye do not look very aesthetically pleasing.
| After the intervention, you need to use antibacterial drops for a certain time. To eliminate the risk of relapse, the doctor recommends using a drug from the “artificial tear” category. The recovery period lasts from four to nine days. |
Treatment with folk remedies
“Grandma’s recipes” are not able to replace drug therapy or surgery, but they will improve the health of the visual organ. They are also used to prevent erosion:
- The positive properties of eyebright herb have long been known. Take a tablespoon of the plant and pour a glass of boiled water. Cool the infusion, strain and use as a compress;
- Prepare chamomile decoction in a water bath. Take a crushed spoon of dried flowers and pour a glass of boiling water. Filter the solution and use it for eye baths;
- Lubricate the damaged eye with sea buckthorn or hemp oil twice a day;
- For lotions, use tea bags. Wring it out and apply it to your eyes for fifteen minutes.
Return to contents
Treatment
Corneal erosion therapy is carried out in 2 stages:
- restoration of the upper layer of the epithelium and resumption of metabolic processes;
- moistening the surface to avoid relapse.
At the first stage, keratoprotectors are prescribed in the form of ointments, gels and eye drops:
- Kerakol;
- Dacrolux;
- Visited;
- Vidisik;
- Oftagel.
Drug for moisturizing and protecting the cornea
Eye drops are usually used during the waking period. Gels and ointments - before bedtime. This will help reduce discomfort from their use.
In order to minimize the risk of infection of the affected eye, antimicrobial drugs are prescribed:
- Tobrex eye drops and analogues;
- Phloxal;
- Tetracycline;
- Erythromycin.
At the second stage, moisturizing eye drops are shown:
- Hyphenation;
- Systane;
- Visine is a pure tear.
In some cases, hormonal medications may be necessary. If erosion occurs as a result of allergic conjunctivitis, antihistamines are prescribed.
All components of combination therapy must be combined with each other. Self-medication is prohibited. Medicines can only be used as prescribed by an ophthalmologist. During therapy, you must strictly adhere to the instructions of your doctor.
Inflammation between the sclera and conjunctiva is episcleritis of the eye.
Patients often complain of the appearance of a white veil before the eyes
Instructions for using Erythromycin eye ointment can be found here.
Prognosis and prevention
With timely treatment, doctors give a favorable prognosis for the outcome of the pathology. If you ignore treatment, you may encounter complications such as corneal ulcers or blindness. The duration of recovery depends on many factors, including the area of damage and the general health of the patient.
The erosion may disappear in three to five days. On average, the duration of the illness is a week. The recurrent form lasts a little longer. To minimize the risk of an anomaly, you must follow simple rules:
- On a sunny day, wear tinted glasses to prevent exposure to harmful UV rays;
- Avoid injury to the visual system. When performing hazardous work, use protective equipment;
- Get regular check-ups with an ophthalmologist;
- If a foreign object gets into the eye, it is important to provide timely assistance;
- Observe basic hygiene rules.
If a foreign body penetrates, it is necessary to rinse the eye with plenty of boiled water, blink quickly and apply eye drops. Do not rub your eyesight under any circumstances!