Only complex therapy will help eliminate phlyctenular conjunctivitis. This eye damage is characterized by the formation of large or small conflicts on the eyeball. When primary symptoms develop, it is important to adhere to personal hygiene rules and consult a doctor. After carrying out diagnostic measures, the doctor will prescribe treatment that will help the conflicts on the conjunctiva to resolve.
Causes of pathology
Phlyctenular keratoconjunctivitis in children is an allergic reaction to bacterial damage to the conjunctiva and cornea. The disease is classified as an endogenous inflammatory process of a toxic-allergic nature. One of the most common factors in the formation of phlyctenular conjunctivitis is infection of sensitized tissues of the organ of vision with mycobacterium tuberculosis, which are transferred from other parts of the body. Among the microorganisms that can provoke pathology, the following bacteria are most often isolated:
- staphylococcus;
- chlamydia;
- Koch's tuberculosis bacillus.
Children of any age and young people are often susceptible to the development of phlyctenular conjunctivitis.
Spring conjunctivitis.
The disease is most common in southern regions with prolonged solar insolation. Boys and young people under 20 years of age are more often affected. The disease is characterized by frequent exacerbations during sunny periods (usually relapses in March - April, summer months). Complaints of eye fatigue during work associated with visual strain, a feeling of a foreign body in the eyes, and severe itching are typical. Patients cannot be in the sun (photophobia and lacrimation appear). The most characteristic sign of the disease is observed when the upper eyelid is everted: on the conjunctiva of the cartilage of the upper eyelid there are hypertrophied papillae - growths in the form of a “cobblestone street”. The upper eyelid thickens somewhat, the palpebral fissure is narrowed, the eyes seem sleepy, and the conjunctiva of the eyes is cloudy. When blinking, the conjunctival papillae irritate the cornea and may become inflamed. By autumn, clinical manifestations usually subside; in winter, patients do not present any complaints, but with the appearance of the sun in spring they resume again.
Emergency first aid for spring conjunctivitis includes:
- eye protection from the sun (sunglasses) ,
- instillation of a 0.25% solution of zinc sulfate or 1% solution of diphenhydramine ,
- referral to an ophthalmologist.
Treatment is carried out local and general.
- Antihistamines are prescribed locally : 1% diphenhydramine solution, 1-2% hydrocortisone suspension, 0.01-0.1% solutions of dexamethasone, oftan-dexamethasone, 0.5% hydrocortisone ointment, injection of dexamethasone under the conjunctiva.
- Subcutaneous injections of histaglobulin 1 ml every 3 days, a total of 6 injections, give a good effect.
- Diphenhydramine, diazolin, suprastin, tavegil are prescribed internally in dosages appropriate for age, and vitamins.
- Cryoapplication is effective .
Prevention of exacerbation of spring conjunctivitis involves:
- eye protection from the sun,
- prescribing preventive courses of antihistamines (histaglobulin, diphenhydramine, etc.),
- dieting,
- sanitation of foci of chronic infection.
Patient care includes washing the conjunctival sac and following doctor’s orders. It is necessary to ensure that patients do not rub their eyes or stay in the sun.
Pollinous (hay) conjunctivitis
Hay fever includes allergic diseases caused by plant pollen. They occur during the flowering period of cereals. One of the manifestations of hay fever is hay fever (hay) conjunctivitis. It is observed in approximately half of patients with hay fever, isolated eye damage occurs in 8-10% of patients. The most common general manifestations of hay fever with conjunctivitis are acute respiratory disease, asthma, and dermatitis. Sometimes body temperature rises.
An acute onset of the disease is characteristic. There is severe itching of the skin of the eyelids and a burning sensation in the eye, increasing swelling and hyperemia of the conjunctiva of the eyelids and eyeball, papillary growths in the conjunctiva, and scanty transparent mucous discharge is observed, sometimes in the form of threads. With pronounced chemosis, marginal infiltrates may appear in the cornea, often within the palpebral fissure. The disease usually continues throughout the entire flowering period of the plants.
When diagnosing hay fever conjunctivitis, in addition to the clinical picture, it is important to take into account the seasonality of the disease. Difficulties arise in identifying its source. To determine the allergen, appropriate intradermal and conjunctival tests are performed. When identifying the source of the disease, specific hyposensitization of the body is carried out with the corresponding pollen allergens. Before the flowering period of plants, preventive hyposensitization is used. Otherwise, the treatment is the same as for allergic dermatoconjunctivitis.
Causes of eye keratitis
There may be several reasons why keratitis occurs. Depending on them they are divided:
- Infectious (viral, bacterial, chlamydial, fungal and parasitic)
- Traumatic
- Immune keratitis
- Allergic
- Neuroparalytic
- Keratitis caused by metabolic disorders
- Superficial
- creeping ulcer
- Phlyctenulous keratitis
Let's look at them in more detail. Viral keratitis, which is most common, is caused by adenoviruses or the herpes simplex virus. This disease can also develop as a result of chicken pox or measles. This disease is recurrent in nature, since it is impossible to completely get rid of the virus, and when immunity decreases, keratitis returns again.
The main causative agents of bacterial keratitis are coccal flora, Staphylococcus aureus, Pseudomonas aeruginosa and other bacteria that penetrate the body. In addition, the cause of its development can be the usual wearing of lenses.
Fungal keratitis is caused by various types of fungi and occurs against a background of decreased immunity. This disease is accompanied by pronounced pain and redness of the eye.
Traumatic keratitis occurs from negative mechanical, thermal, chemical and radiation exposure.
Keratitis of immune origin includes Morin's corrosive corneal ulcer, sclerokeratitis, corneal pemphigus, dry keratoconjunctivitis in Sjögren's syndrome.
Allergic keratitis can occur with spring catarrh, hay fever, and neuroparalytic keratitis develops due to damage to the trigeminal nerve. Inflammation of the cornea of the eye can also be caused by metabolic disorders (diabetes mellitus, hypovitaminosis).
Superficial keratitis occurs as a result of conjunctivitis or other eye diseases. A gray coating appears on the edge of the cornea, which then degenerates into wounds.
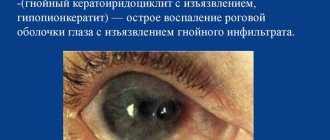
A creeping ulcer occurs as a result of small sharp objects entering the eye and is always accompanied by suppuration. This is a severe form of this disease, since the abscess penetrates deep into the eye, which significantly aggravates the treatment process.
Phlyctenulous keratitis occurs in people with tuberculosis of the lymph nodes. It occurs and is very difficult to treat.
How amblyopia develops in children, causes and treatment methods.
You can read about effective methods of treating retinal macular degeneration in this article.
How to properly treat demodicosis of the eyelids, you will learn by reading the publication at:
Main symptoms: how they manifest themselves
The main symptom of the development of the pathology is the appearance of a yellowish nodule on the cornea of the eye, around which the vessels dilate. Phlyctenucleic keratoconjunctivitis in a child mainly occurs in the acute phase at the initial stage. A phlyctena of the eye develops on the surface of the organ of vision. It is often located on the cornea or conjunctiva. It is a pinkish-yellowish bubble. Unlike tuberculous conjunctivitis, there are no mycobacteria of this genus, and there is also no caseous decay. When a pathological process develops, the following symptoms are present:
- photophobia;
- severe irritation of the organs of vision;
- profuse flow of tears;
- blepharospasm;
- painful sensations.
During the pathological process, conflicts can resolve in different ways. Sometimes it disappears without a trace after 15-20 days, sometimes a residual thin scar forms in this area. But it happens that ulceration may remain on the cornea or conjunctiva. The ulcers are later covered with a layer of epithelium. Options cannot be ruled out when a bubble develops. As a result, it becomes necrotic along with the tissue on which it was formed.
Your dermatologist
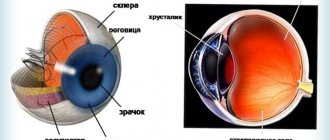
Author: Volokonenko A.I.; Kovalevsky E. I.; Kostyukova T. D.Keratitis (keratitis; Greek: keras, keratos - horn, horny substance) is inflammation of the cornea of various etiologies, accompanied by clouding and decreased vision.
Etiology (causes of occurrence)
The etiology of keratitis is very diverse. Infection is of greatest importance, and pathogens can penetrate the cornea both exogenously and endogenously.
Exogenous keratitis is caused by various microorganisms - pneumococci, Koch-Wicks bacillus, viruses and pathogenic fungi.
The development of keratitis is promoted by chronic diseases of the eyelids, conjunctiva, glands of the cartilage of the eyelids (meibomian glands) and lacrimal ducts.
Keratitis also occurs under the influence of mechanical, chemical and physical environmental factors.
Endogenous keratitis can develop due to chronic infectious diseases of the body - tuberculosis, syphilis, brucellosis, herpetic disease, leprosy, etc., as well as due to metabolic disorders, hypovitaminosis, vitamin deficiencies, and drug allergies.
Classification
The most accepted is the etiological classification of keratitis. There are exogenous and endogenous keratitis.
Exogenous keratitis includes:
- traumatic keratitis caused by the action of mechanical, chemical, thermal factors or the action of radiant energy;
- bacterial keratitis (corneal ulcer, creeping corneal ulcer, etc.);
- keratitis due to diseases of the conjunctiva, eyelids and glands of the cartilage of the eyelids (superficial marginal keratitis);
- keratitis of viral etiology (adenoviral epidemic keratoconjunctivitis, trachomatous pannus);
- fungal keratitis (actinomycosis, aspergillosis).
Endogenous keratitis is divided into:
- infectious (tuberculosis, tuberculosis-allergic, syphilitic, malarial, brucellosis, leprosy);
- viral (herpetic, epidemic keratoconjunctivitis, keratitis due to measles, smallpox);
- neurogenic (neuroparalytic, recurrent corneal erosion);
- hypovitaminous and avitaminous keratitis;
- allergic;
- unknown etiology (rosacea keratitis, filamentous keratitis, corrosive corneal ulcer).
Keratitis is classified according to the depth of damage to the cornea:
- superficial,
- deep.
The article mainly describes the most common keratitis.
Pathological anatomy
The main sign of inflammation of the cornea is the appearance of cloudiness in it due to edema and infiltration of cellular elements. The infiltrate may consist of lymphoid, plasma cells or polynuclear leukocytes penetrating from the marginal looped network of vessels. Infiltration of the cornea is accompanied by various changes in its layers: epithelium, stroma and endothelium.
In severe keratitis, necrosis of the cornea occurs, which leads to softening of the stroma, the formation of an abscess and the development of an ulcer. Sometimes purulent infiltration with disintegration of the entire cornea is observed. With non-purulent keratitis, corneal cells undergo proliferation and degeneration with subsequent decay.
Along with infiltration, newly formed vessels grow into the cornea from the marginal looped network (vascularization); the vessels pass superficially under the epithelium or in the deep layers of the cornea between its plates and are accompanied by strands of connective tissue.
Pathogenesis
In the pathogenesis of keratitis, the general condition of the body, the state of general and local immunity, carried out by humoral antibodies, immune complexes and sensitized lymphocytes, which determine the severity and nature of the inflammatory process in the cornea, are of particular importance.
Clinical manifestations
Characteristic clinical signs of keratitis are:
- symptoms of corneal irritation - lacrimation, photophobia, blepharospasm, and often pain;
- the presence of pericorneal or mixed injection;
- clouding of the cornea, accompanied by a violation of the transparency, shine, specularity, sphericity (smoothness) and sensitivity of the cornea.
Inflammatory infiltrates can have different shapes, sizes and depths of location. They can be pointy, round, have the appearance of branches, streaks, or diffusely cover the entire cornea.
The color of the infiltrate depends mainly on the cellular composition: with a small accumulation of cells of the lymphoid series, the infiltrate has a grayish color, with purulent infiltration it is yellowish, and with significant vascularization it acquires a rusty tint.
The boundaries of the infiltrate are blurred - due to pronounced edema of the surrounding areas of the cornea. Accordingly, the shine and specularity of the cornea disappear above the infiltrate, it becomes rough, and the epithelium sloughs off.
In most cases, keratitis causes vascularization of the cornea by newly formed vessels . With superficial keratitis, the vessels penetrate into it from the vessels of the conjunctiva of the eyeball: they are bright red, branch like a tree and anastomose with each other, pass from the conjunctiva to the cornea through the limbus, heading towards the center of the infiltrate (superficial neovascularization). With deep keratitis, the vessels grow into the thickness of the cornea in the form of tassels, brushes and have a straight course (deep neovascularization). Covered with a relatively thick cloudy layer of infiltrate, they are of a dull, cloudy red color, indistinctly visible and only within the cornea. When the entire thickness of the cornea is affected, vascularization is observed by both superficial and deep vessels.
Simultaneously with the infiltration and ingrowth of blood vessels around the cornea, a pericorneal injection . It comes in varying intensities - from a light pink corolla to a wide dark purple belt covering the cornea. For keratitis, there is also a superficial (conjunctival) injection, but usually it is insignificant.
Outcome of keratitis
The outcome of keratitis depends on the etiology, virulence of the microorganism, the degree of involvement of the cornea and the body's resistance.
Small superficial infiltrates that do not destroy the anterior limiting plate (Bowman's membrane) or are located on the periphery near the pericorneal vasculature can resolve without a trace.
Infiltrates located under Bowman's membrane in the superficial layers of the stroma are partially resolved, and the other part is organized without disintegration, leaving a delicate scar in the form of a cloud-like cloudiness (nubecula) or spot (macula).
Diffuse infiltration of the corneal stroma in the middle and deep layers is usually not prone to decay. It partially resolves and leaves a more or less pronounced scar turbidity.
Purulent infiltrates usually occur with significant tissue necrosis and, as a rule, disintegrate and ulcerate.
Complications arise due to the transition of the inflammatory process to other membranes of the eye - to the iris, ciliary body and sclera with the development of keratoiritis, keratoiridocyclitis and keratoscleritis. In these cases, along with signs of keratitis, the phenomena of iritis, iridocyclitis, and scleritis develop. Due to the toxic effect of microorganisms and their metabolic products, optic neuritis may develop.
In rare cases, perforation of a purulent corneal ulcer can lead to purulent endophthalmitis, secondary glaucoma, subatrophy of the eyeball and sympathetic inflammation of the other eye.
Diagnostics
In typical cases, the diagnosis of keratitis is not difficult and is made on the basis of characteristic clinical symptoms.
Inflammation of the cornea caused by exogenous factors is characterized by superficial keratitis and keratoconjunctivitis with disintegration of the cornea, in particular purulent ulcers.
Endogenous keratitis is characterized by deep parenchymal damage to the cornea without disintegration of its tissue.
A differential diagnostic sign of individual keratitis is the state of corneal sensitivity . A decrease, and sometimes a complete loss of sensitivity, is more often observed with neurogenic and herpetic keratitis. In this case, sensitivity is often lost in the other eye, which indicates a general violation of nerve trophism.
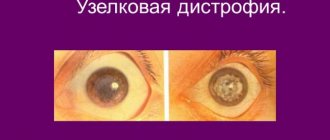
Differential diagnosis
Differential diagnosis is carried out with degenerative processes in the cornea.
Primary corneal dystrophies are usually bilateral, characterized by a chronic course, slowly progressing, photophobia is only sometimes noted, there is no vascularization of the cornea, and its sensitivity is reduced.
To establish the etiology of keratitis, a set of laboratory methods is used, including:
- cytology of the conjunctiva,
- fluorescent antibody method,
- serological methods - complement fixation reaction, neutralization reaction, nephelometry with viral, microbial, tissue and drug allergens,
- intradermal and focal tests with herpes vaccine, tuberculin, brucellin and other antigens.
Treatment
Treatment of keratitis is usually carried out in a hospital setting, especially for acute and purulent keratitis and is aimed at the disease that caused the keratitis.
In order to reduce inflammation and pain , as well as to prevent fusion and fusion of the pupil, early prescription of mydriatic drugs is necessary - instillation of a 1% solution of atropine sulfate 4-6 times a day, 1-2 times a day atropine in an eye medicinal film, at night 1 % atropine ointment, electrophoresis with 0.25-0.5% atropine solution. A 0.25% solution of scopolamine is also prescribed. Both of these remedies can be combined with instillations of a 0.1% solution of adrenaline, which is also used on cotton swabs inserted behind the lower eyelid for 15-20 minutes, or with the introduction of this solution under the conjunctiva in an amount of 0.2 ml.
For the treatment of patients with bacterial keratitis and ulcers of the cornea, sulfonamides and broad-spectrum antibiotics are prescribed in the form of solutions, ointments, and also in ophthalmic medicinal film 2 times a day. The choice of antibiotic is carried out depending on the sensitivity of the pathogenic microflora to it. For severe corneal ulcers, antibiotics are additionally administered under the conjunctiva. If local antibiotic therapy is insufficiently effective, oral antibiotics are prescribed.
After the end of the inflammatory process, osmotherapy and resorption treatment . Apply 2-3% solutions of potassium iodide in the form of electrophoresis. Common remedies include biogenic stimulants (liquid aloe extract, FiBS, peloid distillate, vitreous body, etc.) and autohemotherapy.
For appropriate indications, surgical treatment (keratoplasty, optical iridectomy, antiglaucomatous surgery).
Forecast
The prognosis depends on the etiology of the disease, location and nature of the infiltrate.
With timely and correct treatment, small superficial infiltrates, as a rule, resolve completely or leave slight opacities. Deep and ulcerative keratitis in most cases results in the formation of more or less intense opacities of the cornea and a decrease in visual acuity, especially significant in the case of a central location of the lesion.
However, even with leukomas, one should keep in mind the possibility of returning vision after successful keratoplasty.
Prevention
Prevention consists of preventing eye injuries, timely treatment of blepharitis, conjunctivitis and general diseases that contribute to the development of keratitis.
To prevent adenoviral keratitis, it is necessary to avoid contact with patients, carefully follow the rules of asepsis during medical procedures - individual pipettes and sticks, daily change of medications, disinfection of medical instruments and devices.
Separate forms of keratitis
Traumatic keratitis
Traumatic keratitis develops with non-penetrating injuries to the cornea, foreign bodies entering the eye, burns and penetration of microorganisms into the wound.
Clinical manifestations
The clinical picture depends on the severity of the injury, the type of microorganism and is similar to the clinical picture of bacterial keratitis.
Bacterial keratitis
The most serious disease is a creeping corneal ulcer, which, before the discovery of antibiotics and sulfonamides, often resulted in blindness and death of the eye. The causative agent is most often pneumococcus, less commonly streptococcus, staphylococcus, and Pseudomonas aeruginosa.
The occurrence of an ulcer is almost always associated with a violation of the integrity of the corneal epithelium, which can be caused by small foreign bodies, leaves and branches of trees, sharp spines of cereal plants and grains. Cases of creeping corneal ulcers are especially common in summer and early autumn during agricultural work.
The pathogen is rarely introduced by a foreign body; more often, pneumococcus is located in the conjunctival sac as a saprophyte and, when the integrity of the corneal epithelium is damaged, it penetrates into the damaged cornea, causing, thanks to its powerful proteolytic properties, a violent inflammatory-necrotic process.
The disease begins acutely and is accompanied by severe cutting pain, blepharospasm, photophobia, lacrimation, severe mixed injection and chemosis of the conjunctiva. An infiltrate with a yellowish tint appears in the center of the cornea, as a result of the disintegration of which a disc-shaped ulcer with a purulent crater-shaped bottom is formed. One edge of the ulcer is raised, progressive, undermined, the other is smooth, regressing.
Often, under the influence of proper treatment, the ulcer is cleared and the resulting corneal defect is covered with epithelium, and a depression remains at the site of the ulcer, which is subsequently filled with connective tissue, forming a persistent, intense clouding of the cornea.
In severe cases, the progressive edge of the ulcer quickly increases and within a few days the ulcer can cover most of the cornea. The iris is involved in the process very early. At the same time, its color changes, pus appears in the anterior chamber, the pupil narrows, and posterior synechiae are formed. Lysis of the cornea can lead to perforation. After perforation, the ulcer heals, followed by scarring and the formation of a cataract fused with the iris.
In very severe cases, the cornea quickly melts, the infection penetrates inside, causing an abscess of the vitreous body and then purulent inflammation of all the membranes of the eye, followed by subatrophy of the eyeball. Patients with a creeping corneal ulcer are subject to immediate hospitalization. Active anti-inflammatory local and general treatment should be prescribed using broad-spectrum antibiotics, sulfonamides in instillations, in the form of subconjunctival injections, and in an eye medicinal film.
To increase epithelization of the cornea, instillation of a 2% solution of quinine sulfate is prescribed 5-6 times a day. To prevent iridocyclitis, mydriatics are used: a 1% solution of atropine sulfate in combination with a 0.1% solution of adrenaline and a 3% solution of cocaine. If the inflammatory process cannot be treated within the next 3 days, cryoapplication is recommended.
In extremely severe cases, they resort to diathermocoagulation of the progressive edge of the ulcer with the capture of borderline healthy tissue.
When hypopyon appears, it is recommended to open the anterior chamber of the eye (paracentesis) followed by washing it with a weak solution of antibiotics.
If there is a threat of perforation, in some cases therapeutic keratoplasty is performed.
Superficial marginal keratitis
Superficial marginal keratitis occurs against the background of infectious conjunctivitis or blepharitis and is characterized by the appearance of pinpoint infiltrates along the edge of the cornea. Infiltrates tend to merge and ulcerate; in such cases, a marginal corneal ulcer occurs with a torpid course. The ulcer is gradually replaced by scar tissue.
Treatment
Treatment should first of all be aimed at eliminating the cause that caused marginal keratitis, otherwise it is the same as for all ulcerative keratitis.
Adenoviral epidemic keratoconjunctivitis. Fungal keratitis.
Keratomycosis is a relatively rare disease of the cornea caused by various types of pathogenic fungi that live in the conjunctiva and lacrimal ducts. The use of antibiotics and corticosteroids causes the activation of fungal flora, which acquires pathogenic properties. Most often they are caused by mold fungi, less often by radiant fungus - actinomycetes and yeast fungi.
Infection of the cornea often occurs after minor injuries. At the site of erosion, a grayish-white lesion appears with a crumbly, loose surface with a yellowish border. Fungal keratitis is characterized by the presence of a hypopyon.
The disease can last for weeks, destruction is slow, and vascularization is usually absent. Corneal perforations are rare, although possible.
Diagnosis is difficult. If a corneal ulcer does not respond to antibiotic treatment for a long time, it is necessary to think about a fungal infection. The diagnosis is made on the basis of a microscopic examination of the pathological material, which reveals filaments of mold or drusen of radiata fungus.
It is recommended to remove the affected area of the cornea with a knife, followed by cauterization with a galvanocauter or a 5% alcohol solution of iodine. If there is no effect, they resort to therapeutic keratoplasty. Antifungal agents include amphotericin drops (0.2% solution) 6-8 times a day, trichomycin 1 tablet (50,000 units) 4 times a day, nystatin 1 tablet 4 times a day for 10-14 days. . For actinomycosis, sulfadimezin 0.5-1 g 4 times a day is effective.
Tuberculous keratitis
Tuberculous keratitis is divided into 2 groups different in their pathogenesis:
- hematogenous keratitis arising from bacterial foci of the vascular tract,
- tuberculous-allergic keratitis due to sensitization of the cornea to mycobacteria.
There are two forms of tuberculous hematogenous keratitis:
- deep diffuse,
- sclerosing.
Deep diffuse tuberculous keratitis is characterized by diffuse infiltration of the middle and deep layers of the cornea, against which characteristic denser foci of infiltrate of a yellowish-pinkish color without a tendency to merge stand out. Along with deep vessels, there are also superficial ones in the cornea. As a rule, one eye is affected.
The course is long, remissions alternate with periods of exacerbation, which significantly delays the course.
Sclerosing tuberculous keratitis often develops with deep scleritis. Yellowish-white infiltrates in the form of triangles slowly spread from the limbus to the center of the cornea. Vascularization of the cornea is weak. The process continues for months and even years.
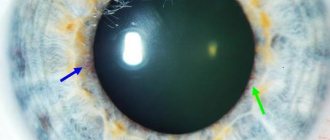
Tuberculous-allergic, or phlyctenulous, scrofulous keratitis is usually observed in children and adolescents and is characterized by a wide variety of clinical forms, duration of course, frequent exacerbations and relapses.
A characteristic symptom of this disease is phlyctena - an infiltration nodule consisting mainly of lymphoid cells and a small number of epithelioid and plasma cells. Unlike true tubercle, phlyctenas contain neither tuberculosis bacilli nor caseous decay.
Phlyctens develop more often at the limbus, but can be on any part of the cornea; they look like grayish translucent elevations. Their number and size are different: from the smallest multiple (miliary) to large single (solitary) conflicts. They are usually approached by a bundle of superficial vessels. Phlyctens sometimes disintegrate, turning into phlyctenulous ulcers.
Treatment
Treatment of tuberculous keratitis is complex. Anti-tuberculosis chemotherapy drugs and antibiotics, etc. are widely used. Specific treatment is carried out against the background of a general desensitizing drug (diphenhydramine, multivitamins, intravenous calcium chloride). Streptomycin 100,000 units, 5% saluzide solution, hydrocortisone and dexazone in drops and under the conjunctiva of the eyeball are prescribed locally.
For phlyctenular keratoconjunctivitis, 1% yellow mercury ointment is effective. In case of deep keratitis, mydriatics and dry heat are indicated to avoid the formation of posterior synechiae.
Treatment
Treatment is carried out against the background of a balanced diet, rich in fats and proteins with limited carbohydrates. Quartz irradiation and climatotherapy are indicated.
Syphilitic keratitis
With congenital syphilis, parenchymal diffuse keratitis is most common, with acquired syphilis, deep punctate keratitis, pustuliform deep keratitis and corneal gumma. In typical cases, parenchymal keratitis has 3 stages of development.
In the initial period (3-4 weeks), diffuse gray opacities appear in the middle and deep layers of the cornea, consisting of individual point infiltrates. They are located on the periphery of the cornea and only later spread to its center.
The second stage (6-8 weeks) is characterized by progression of the process. The infiltration of the cornea sharply increases, and its abundant vascularization appears. The entire cornea becomes diffusely cloudy and sometimes acquires a rich white color.
In the third, regressive stage, irritation phenomena decrease, infiltration resolves. Resorption of infiltrates continues for about 1 year or more.
Treatment
Treatment is carried out depending on the stage of syphilis with antibiotics according to established regimens.
Locally prescribed 1% yellow mercury ointment, mydriatics, corticosteroids in drops and under the conjunctiva. Paraffin baths, UHF, Sollux, and medicinal electrophoresis are useful.
Herpetic keratitis
Herpetic keratitis occurs in the form of herpes corneae simplex and herpes corneae zoster. They are characterized by a sharp decrease or complete absence of corneal sensitivity and the absence or late appearance of its vascularization, as well as a tendency to relapse.
With herpes corneae zoster, damage to the first branch of the trigeminal nerve is observed. The most typical form is deep keratitis; sometimes a deep ulcer is formed with grayish foci of infiltration. Inflammation of the cornea is accompanied by (herpes iridis) or iridocyclitis, and sometimes more extensive eye lesions are observed (scleritis, optic neuritis, paralysis of the eye muscles).
In terms of frequency and severity, herpetic keratitis caused by herpes corneae simplex occupies one of the first places among keratitis of other etiologies.
There are:
- primary herpetic keratitis, which occurs in childhood when the herpes virus first enters the human body,
- developing in adults against the background of a latent viral infection.
Primary herpetic keratitis occurs in the form of epithelial keratitis and keratoconjunctivitis with ulceration and vascularization. Epithelial keratitis is combined with conjunctivitis and is characterized by the appearance of pinpoint whitish or grayish foci of infiltration and the formation of vesicles that lift the epithelium, the rejection of which leads to corneal erosion. With keratoconjunctivitis with ulceration and vascularization, diffuse opacification of the epithelium is observed, followed by its destruction and rejection, leading to the formation of an ulcer. The inflammatory process occurs against the background of pronounced vascularization of the cornea and results in persistent clouding.
One of the most common forms after primary herpetic keratitis are various types of tree-like keratitis - vesicular, stellate, punctate and transitional forms - tree-like with stromal damage and “geographical” (map-like) keratitis. With tree-like keratitis, against the background of acute symptoms of irritation, small gray bubbles appear in the cornea along the nerve trunks, which, when fused, resemble a tree branch.
This form rarely proceeds favorably, ulceration often occurs, the inflammatory process spreads to the stroma and is complicated by the development of iridocyclitis.
Stromal (deep) keratitis is always accompanied by damage to the vascular tract and is therefore called herpetic keratoiritis. Metaherpetic keratitis occurs when dendritic keratitis spreads into the deep layers of the stroma, which is often associated with the widespread use of corticosteroids. The spread of infiltration into the deep layers of the cornea leads to the development of an extensive metaherpetic ulcer with landscape-like outlines.
The process is characterized by a long course, resulting in extensive clouding of the cornea. Discoid keratitis is pathognomonic for herpetic keratitis, although it sometimes occurs in other corneal diseases.
Characteristic is the presence of a deep, round, grayish-white infiltrate in the center of the cornea. The cornea can be sharply thickened, and vascularization appears relatively late. Almost always, iridocyclitis is observed with precipitates on the posterior surface of the cornea, corresponding to the infiltrate disk. Infiltrates, as a rule, do not disintegrate and do not leave defects in the epithelium.
The course is persistent, chronic.
Deep herpetic diffuse keratitis always occurs against the background of severe iridocyclitis, therefore it is more often called keratouveitis. It is accompanied by diffuse opacification of the cornea with edema of the stromal epithelium and endothelium and the formation of inflammatory necrobiotic foci in the stroma, the presence of precipitates, newly formed vessels in the iris, exudate, often the development of a bullous form with the appearance of blisters and erosions in the epithelium, with a frequent increase in intraocular pressure in the acute period of the disease.
The fluorescent antibody method and a focal test with herpetic antigen are of greatest value for the diagnosis of herpetic keratitis.
Treatment is based on the complex use of etiotropic agents aimed at limiting the reproduction of the virus in the tissues of the eye (keretsid, tebrofen, oxolin, florenal), increasing the immunity of cells to infection (interferon, interferonogens), and the use of various means of metabolic and symptomatic action.
For superficial keratitis, one of the antiviral drugs is used - keretsid in drops 6 times a day. Deoxyribonuclease is prescribed 4-5 times a day, oxolinic ointment 0.25% 3 times a day, interferon drops 4-5 times a day (150-200 units of activity), florenal and tebrofen ointments 2-3 times a day at 0. 25-0.5% concentration. Similar treatment is carried out for deep forms of keratitis. Good results have been obtained with the use of various interferon inducers.
Local use of corticosteroids in the form of instillations of a 0.5% hydrocortisone solution is indicated. Corticosteroids can be prescribed only in the absence of defects in the corneal epithelium, with deep stromal forms involving the vascular tract.
Cryotherapy, laser coagulation and physiotherapy (drug electrophoresis, microwave therapy, diathermy, phonophoresis) are used in the treatment of various forms of herpetic keratitis. If there is no effect, therapeutic keratoplasty is performed.
Neuroparalytic keratitis
Neuroparalytic keratitis develops due to primary damage to the trigeminal nerve.
A characteristic symptom of neuroparalytic keratitis is a sharp decrease or complete loss of corneal sensitivity. Photophobia, lacrimation and blepharospasm are usually absent. Severe neuralgia is often observed.
In uncomplicated cases, the process begins with clouding of the surface layers of the cornea and desquamation of the epithelium in the center. In this case, a shallow ulcer is formed that does not heal for a long time. Complications such as secondary glaucoma, endophthalmitis and panophthalmitis may develop.
Treatment
Treatment should be aimed at improving corneal trophism. For this purpose, ATP 1 ml intramuscularly for 25-30 injections, Nerobol 1 tablet 3 times a day for a month, B vitamins are used.
Locally prescribed 1% solution of quinine hydrochloride, 30% solution of sodium sulfacyl, 1% tetracycline ointment.
Hypovitaminous and avitaminous keratitis
Hypovitaminous and avitaminous keratitis most often occur due to a lack of vitamin A in the body, and in rare cases, vitamins B1, B2 and C.
Vitamin A deficiency can manifest itself in the form of xerosis and keratomalacia.
Rosacea-keratitis
Rosacea keratitis develops in older people with facial rosacea. The etiology and pathogenesis have not been fully elucidated. A certain role in the pathogenesis of acne rosacea is played by disruption of the acid-forming function of the gastric glands.
In the cornea, more often at the limbus, grayish-white infiltrates appear, clearly demarcated from the normal corneal tissue and slightly rising above its surface. From the limbus to the infiltrates, superficial vessels grow in the form of several large stems, which break up into small loops only near the infiltrates. The latter may ulcerate to a greater or lesser depth, but perforation of the cornea is rare. In severe cases, the ulcer may progress slowly.
Treatment
Treatment is carried out with corticosteroids in the form of instillations and subconjunctival injections; Vitamins A, B2, B6, desensitizing agents, and novocaine periorbital blockade are prescribed.
Radiation keratitis
Radiation keratitis can occur when the eye is irradiated due to tumor diseases, when working with sources of ionizing radiation, and during experimental studies. After direct irradiation of the cornea, keratitis occurs fairly quickly. The severity of keratitis varies and depends on the radiation dose. The minimum radiation dose that causes keratitis is 200 rad. In this case, the method of eye biomicroscopy can reveal the initial signs of keratitis.
In the mildest cases, photophobia and lacrimation appear; Dotted areas stained with fluorescein appear in the superficial layers of the cornea. In the limbus area, redistribution of pigment may be observed. The sensitivity of the cornea decreases. Superficial erosions and punctate keratitis go away without a trace, unless infection occurs. With application β-therapy, a single dose per eye of about 1000 rad can cause superficial keratitis with clinical recovery by the end of the 3rd week. The transparency of the cornea and its sensitivity are completely restored.
In experiments in rabbits under conditions of fractionated exposure in doses of 5000-10,000 rads, deep keratitis may occur, followed by clouding of the cornea. These opacities are most often round in shape and located under the epithelium. Epithelization proceeds very slowly. The sensitivity of the cornea does not recover for a long time. Its swelling in its severity leads to loss of visual functions of the eye.
With total doses of 20,000 rads and higher, profound changes occur in the cornea in the early stages, manifesting as parenchymal or ulcerative keratitis. There is no corneal sensitivity. As a rule, such keratitis is accompanied by secondary changes in the iris. An abundant proliferation of blood vessels in the cornea may be observed both during the period of irradiation with high doses and in the long term after it. The resulting vascularized corneal cataract can ulcerate. Sometimes corneal necrosis occurs. In rare cases, such severe forms of radiation keratitis can cause death of the eye.
Treatment
Treatment of radiation keratitis is very difficult. It should be aimed at preventing infection and include drugs that improve tissue metabolism of the cornea (vitamins, citral, thiamine ointment, sea buckthorn oil).
For severe keratitis, therapeutic keratoplasty is indicated.
Great Medical Encyclopedia 1979
First aid
With the development of primary symptoms of phlyctenular conjunctivitis in children, certain rules should be followed. It is important to support them both before going to the doctor and after the clinic. Features of behavior when the first signs of the disease appear:
To eliminate microorganisms, if an illness is detected, it is necessary to rinse the organs of vision.
- You should not touch your face, much less the eye area, with your hands.
- You should maintain personal hygiene and not skip procedures.
- It is forbidden to apply bandages to the organs of vision.
- For severe photophobia, it is recommended to use sunglasses.
- Rinsing the eye area regularly will eliminate some bacteria.
- Cleansing the organs will also help get rid of any remaining discharge in the affected area of the eyelashes and in the corners of the eyes.
When washing the visual apparatus, it is recommended:
- Sterilize the water for the procedure by boiling it for at least 60 seconds.
- Pour boiling water over the wash tray to destroy bacteria and dust.
- For best results, you should have separate accessories for each eye, because one of them may be less affected by infection.
- It is advisable to filter the water so that small debris does not damage the surface tissues of the organs.
- To carry out the manipulation, pour the solution, well dissolved in water, into the bath. Then you need to lower the affected eye into the container and blink frequently.
Phlyctenular conjunctivitis in children
The disease most often occurs in children under 3 years of age, including newborns. The primary symptoms of the disease are eye irritation, fear of bright light, and painful sensations. Soon, conflicts appear on the membrane of the eye, to which a nodule of blood vessels approaches. They form around the cornea without affecting the pupil and iris. Signs of the disease may appear in one eye, simultaneously or at short intervals in both eyes. During the course of the disease, phlyctenes transform into ulcers. With timely and proper treatment, they go away without leaving scars.
Due to discomfort and pain, the child practically does not open his eyes. At the same time, tears flow constantly. As a result of this process, cracks appear on the eyelids and outer corners of the eyes, which also cause additional pain.
Phlyctenular conjunctivitis in children may also be accompanied by a symptom such as blepharospasm. This is the process of uncontrolled contraction of the orbicularis oculi muscle.
Sometimes, with the disease, eczema appears in the corners of the mouth, at the wings of the nose and earlobes, and the cervical lymph nodes also become enlarged.
To prescribe treatment for phlyctenular conjunctivitis in a child, an examination and consultation with a phthisiatrician, pediatrician and ophthalmologist will be required. The doctor prescribes restorative and antihistamine and antiallergic drugs. First of all, they fight secondary allergenic factors by deworming, limiting carbohydrates and salts in food, sanitizing the oral cavity, treating infectious diseases, etc.
After diagnosing phlyctenular conjunctivitis in a child, it is necessary to adhere to a number of rules:
- Do not touch your eyes with your hands;
- it is necessary to maintain personal hygiene;
- It is forbidden to apply bandages to the organs of vision;
- You should regularly wash your eyes with special compounds.
In some cases, the transformation of phlyctena into small ulcers can affect the cornea of the eye, disrupting its transparency. As a result, vision loss occurs.
Bacterial keratitis
Creeping corneal ulcer (Ulcus sernens)
The disease is characterized by severe cutting pain in the eye, lacrimation and suppuration, photophobia, blepharospasm, severe mixed injection and chemosis. The infiltrate in the cornea has a grayish-yellowish color. In the first day it disintegrates, resulting in the formation of a disc-shaped ulcer with a purulent crater-shaped bottom (Fig. 91). One edge of this ulcer is regressive, smooth, the other is progressive, undermined, yellow; Diffuse opacities and infiltration of the cornea are always observed in this place. The progressive edge grows rapidly, and within a few days the ulcer covers most of the cornea. Vessels, deep or superficial, usually do not approach the ulcer. In a short period of time, the choroid is involved in the process. Pain in the eye increases, the color of the iris becomes yellow-green, the pupil takes on an irregular shape due to the appearance of powerful posterior adhesions. At the bottom of the anterior chamber, a hypopyon of yellow color and liquid consistency, consisting of fibrin and leukocytes, is formed.
Rice. 91. Creeping corneal ulcer
Lysis (dissolution) of the cornea and its perforation may occur. If the infection enters the eye through the perforation, acute inflammation of all the membranes of the eye develops (panophthalmitis).
Corneal ulcers occur predominantly in children living in rural areas, where the occurrence of ulcers is almost always associated with violations of the integrity of the corneal epithelium during harvesting and threshing of cereal crops, preparing haylage, etc. Plasma-coagulating strains of bacteria located in the conjunctival cavity, most often pneumococci, staphylococci, and streptococci, diplobacillus, Pseudomonas aeruginosa, etc., penetrate into the damaged cornea and, having powerful proteolytic properties, cause a violent, lightning-fast, inflammatory-necrotic process.
Table 23. Differential diagnostic signs of keratitis
Treatment of corneal ulcers consists primarily of general and local application of loading doses of antibiotics and sulfonamide drugs. Pain in the eye should be immediately eliminated (relieved) by instilling anesthetics, preferably a 5% novocaine solution, every hour.
Antibacterial, neurotrophic, regenerative and other drugs in the form of drops and ointments are administered into the conjunctival sac by a forced method every 5 minutes for an hour, followed by an hour break, and then again for an hour and so on 3-4 times a day for 3-5 days, i.e. until the process subsides and epithelization of the ulcer begins. Before instillation, the eyes are washed with weak disinfectant solutions, as well as very weak solutions of acids and alkalis to acidify or alkalize the environment of the conjunctival sac, depending on the properties of the pathogen.
Along with sulfonamide drugs and antibiotics, vitamin drops are used, as well as mydriatics or miotics (2-3 times a day) depending on the depth of the ulcer. If the process progresses quickly, when there is a danger of perforation of the cornea, cryo- and diathermocoagulation of the progressive edge, paracentesis and rinsing of the anterior chamber with broad-spectrum antibiotics are performed; for persistent pain in the eye area and a torpid course of the process, periorbital novocaine blockades are prescribed.
Analgesics (salicylates) and desensitizers (calcium gluconate, suprastin, etc.) are prescribed internally. During the recovery period, absorbable therapy (dionine, lidase, etc.) is carried out in the form of drops and electro(phono)phoresis. Corticosteroids and enzymes are contraindicated in the active stage of the disease, but useful in the regeneration stage. Often in the future (after 6-12 months) the cataract can be eliminated using the most optimal option, keratoplasty or keratoprosthesis.
Catarrhal corneal ulcer (Ulcus catarrhalis)
Catarrhal ulcer of the cornea, or superficial catarrhal keratitis, is characterized by the fact that, against the background of bacterial conjunctivitis, diseases of the eyelid margin (blepharitis, etc.) or lacrimal organs (dacryocystitis), small grayish infiltrates appear along the edge of the cornea concentrically to the limbus. They are located predominantly superficially - in the epithelium and under it. The occurrence of infiltrates is accompanied by pericorneal injection, photophobia, lacrimation and blepharospasm. Pain is often felt. Infiltrates in some cases are prone to reverse development without scarring, in others they merge, become necrotic, after which more or less deep ulcers form in the form of arcuate curved grooves, leaving behind clouding of the cornea. The process is usually sluggish, but long-lasting. The comparatively favorable course of this type of keratitis is due to the weak virulence and pathogenicity of the pathogen and the resistance of the cornea. The etiological diagnosis is based on clinical data and the results of laboratory tests (scraping, culture).
Treatment of catarrhal corneal ulcer consists of general and local use of antibiotics and sulfonamide drugs, to which the bacterial flora is sensitive. Antibiotics, sulfonamide drugs, amidopyrine, vitamins and absorbable agents are prescribed in the form of forced instillations (4-5 cycles per day for 7-10 days). Before instilling these drugs, be sure to administer anesthetics (preferably a 5% novocaine solution) and wash the cavity with a heated solution of one of the antiseptics.
Mydriatics are also prescribed, often short-acting (1% homatropine solution, 0.25% scopolamine solution), 2-3 times a day, vitamin drops and ointments.
During the period of subsidence and reverse development of the disease, more active resorption therapy is carried out in the form of electro(phono)phoresis of enzymes, tissue preparations, etc. General and local desensitizing therapy (corticosteroids, calcium chloride, suprastin, etc.) is also indicated. Measures are taken to eliminate the source of infection.
It must be remembered that each pathogenic flora that causes corneal ulcers develops in a specific environment and is not sensitive to all antibiotics and sulfonamide drugs. For example, for diplobacillary ulcers, antibiotics and sulfonamide drugs are ineffective.
Prescribing them without laboratory results will only delay the use of the necessary medications (zinc sulfate), and therefore create conditions for the worsening of the process. One more example. The development of pneumococcus is promoted by an alkaline environment, therefore, if it is present, eye rinsing with 2% boric acid is indicated. In case of extensive scar changes, keratoplasty or keratoprosthesis can be performed 6-12 months after recovery.
Treatment
Phlyctenular keratoconjunctivitis develops faster than other forms of the disease.
It can get to the point where the main symptoms appear within a few hours and cause severe discomfort and pain.
And in such cases, first aid may be required.
The first action should be instillation of a suspension of hydrocortisone (two drops in each eye), after which a 1% solution of atropine sulfate is instilled and yellow mercury ointment is applied in a 2% concentration .
Keep in mind! For basic treatment, the following drugs are used:
- 10% calcium chloride solution (intravenously);
- streptomycin (intramuscular);
- anti-tuberculosis drugs (saluzide, tubazid);
- dexamethasone 0.1% in the form of drops (up to four times a day);
- Alomide (up to 6 times a day);
- cortisone (in the form and dosage recommended by your doctor);
- multivitamin complexes according to the scheme in accordance with the instructions.
Diagnostics
To make an accurate diagnosis, the doctor will take an anamnesis and prescribe additional tests. During diagnostic procedures, the doctor initially needs to find out exactly the nature of organ damage. To do this, the patient is interviewed about the symptoms accompanying the disease, as well as about the course of the pathological process. To make a diagnosis, your doctor will need the results of the following tests:
- skin scraping;
- immunological reactions;
- cystoscopy from the conjunctival area;
- bacteriological analysis.
Prevention
To prevent conjunctivitis, experts recommend adhering to the following rules of prevention:
- Wash your hands with soap before touching your face and eyes;
- Individual towels;
- In case of allergic conjunctivitis, do not be near the allergen to prevent its contact with the mucous membrane.
- In the professional version, wear glasses, respirators and other protective equipment.
People of different ages experience eye conjunctivitis, and each patient’s disease progresses individually. Therefore, it is very important to consult an ophthalmologist at the first signs to make an accurate diagnosis.
Eye keratitis - symptoms and treatment, photos, causes of the disease in adults and children
Blepharitis - photos, symptoms and treatment in adults
Description:
- There is no specific prophylaxis that could prevent the development of the disease.
- Secondary prevention methods boil down to the fact that allergens must be removed from the surrounding area.
- A person must adhere to a certain diet and lifestyle, which is typical for all allergy sufferers.
- If a person finds himself in potentially dangerous conditions, combination eye drops should be used, which provide an immediate effect that remains effective for half a day.
- During the period of remission, specific immunotherapy is implemented.
Doctor's conclusion and recommendations
Regardless of whether an adult or a child is allergic, it is very important to pay due attention to your health. Experts advise periodically visiting an allergist who will give recommendations based on your actual health condition.
Tuberculous-allergic conjunctivitis.
Tuberculous-allergic conjunctivitis ( scrofulous, phlyctenulous ) is a typical allergic disease that occurs mainly in children and young people suffering from tuberculosis of the lungs or lymph nodes in the presence of additional allergic factors (diathesis, helminthic infestation, etc.).
The disease begins with the appearance of photophobia. (phlyctenae) with a diameter of 1-1.5 mm appear on the conjunctiva of the eyeball Usually there are 2-3 such nodules, rarely more. A feature of this disease is the location of the described nodules on the border between the conjunctiva and the cornea or in close proximity to this border (at the edge of the cornea).
Dilated vessels approach the phlyctenas in a bundle. Severe photophobia, lacrimation, and blepharospasm are very characteristic. The patient cannot open his eyes and hides his head in the pillow. There is often maceration and cracks in the corners of the palpebral fissures, eczematous changes behind the ears, and in the corners of the mouth. After 5-6 days, the conflicts flatten and gradually resolve. In weakened individuals, there may be ulceration of phlyctena followed by epithelization. The disease lasts for 2-4 weeks, with frequent relapses.
Emergency first aid for scrofulous conjunctivitis is usually limited to instilling drops of a 0.2% solution of chloramphenicol or 1-2% emulsion of hydrocortisone, oftan-dexamethasone into the eye. The patient should be referred to an ophthalmologist or phthisiatrician to prescribe a diet and therapeutic measures. As a rule, there is no need to be hospitalized. Treatment should be general and local.
- A diet with limited carbohydrates, food rich in vitamins, sanitation of the oral cavity, deworming, and treatment of infectious diseases are indicated
- At the same time, immediate and active desensitizing and nonspecific anti-inflammatory drug therapy . It consists of prescribing calcium supplements, fish oil or its derivatives, cortisone, diphenhydramine, etc.
- On the recommendation of a phthisiatrician, general specific treatment is carried out - streptomycin, sodium para-aminosalicylate (PAS-sodium), isoniazid (tubazid), etc.
Prevention of phlyctenular conjunctivitis includes carrying out a general medical examination of the population in order to identify tuberculosis with subsequent treatment by a phthisiatrician, observing a diet by patients with tuberculosis, sanitizing their foci of infection, and preventing helminthiasis.
Care for patients with scrofulous conjunctivitis is carried out at the place of treatment (in the hospital, at home). It includes the implementation of all medical procedures (taking medications, installing eye drops), careful monitoring of adherence to the regimen, diet, since the slightest violation of them by the patient is enough for inflammation of the outer membranes of the eye to flare up again.
How are they treated?
Pediatric patients are examined by two doctors simultaneously. To prescribe optimal therapy, you will need to consult a pediatrician and TB specialist, and sometimes an ophthalmologist.
To eliminate pathology, it is necessary to use complex treatment, which is aimed at fighting microbes and strengthening the visual system. Treatment of phlyctenular conjunctivitis is quite specific, therefore, if the doctors are incomplete, side effects may occur. Therapy requires not only eliminating the bacterial infection, but also improving the condition of the visual system. To counteract the inflammatory process, restorative and desensitizing drugs are prescribed. Sometimes a patient with phlyctenular conjunctivitis requires other parallel treatment:
- therapeutic and preventive measures of the oral cavity;
- deworming;
- rehabilitation of the nasopharynx and paranasal sinuses;
- compliance with dietary restrictions.
Complex therapy helps to quickly eliminate the infection, restore normal eye function and strengthen immune abilities. However, repeated outbreaks of the disease cannot be ruled out. Often, as people get older, they appear less frequently, and in adulthood they rarely occur at all.
Allergic conjunctivitis. Spring, atropine, tuberculous-allergic conjunctivitis.
The role of allergic conjunctivitis in eye pathology is increasing every year. Allergic conjunctivitis usually has a chronic course and is mostly bilateral.
The disease occurs in the form of remissions and exacerbations. During an exacerbation of the disease, the leading symptom is itching; during remissions, patients complain of a foreign body sensation, tingling in the eyes, and discomfort during visual work.
Allergies can be caused by:
- external factors, i.e. be of an exogenous nature (the effect of plant pollen, cereal grasses, for example, timothy, bluegrass, fescue, fluff, wool, dust, drug and food allergies), and
- endogenous , that is, internal factors (infectious, helminthic allergies, spring conjunctivitis).