TRADITIONAL OPINION OF TEACHERS
Traditionally, little time has been devoted to eye examination in the curriculum. However, some findings obtained during physical examination can be extremely important, and practitioners should be aware of this. All methods of eye examination - from measuring visual acuity to ophthalmoscopy - provide chain information and can help in revealing important secrets not only of the eye, but also of the body as a whole.
| TYPE OF EYE EXAMINATIONS | TRADITIONAL OPINION | |
| Visual acuity | ↑ | By analogy with basic physiological indicators (heart rate, temperature, blood pressure), visual acuity is measured and recorded at the very beginning of the eye examination |
| Visual field examination | ↑ | This method allows you to identify (and differentiate) important neurological and ocular diseases |
| Pupil examination | ↑ | May provide invaluable clinical information |
| External examination of the eye | ↑ | Many outdoor examinations are performed using a flashlight pen. Pay attention to the orbits of the eyes, the position of the eyelids, the conjunctiva, the anterior chamber of the eye, the corneal reaction to light |
| Ophthalmoscopy | ↑ | The key to mastering this method is practice: the more often you perform ophthalmoscopy, the better results you will achieve |
| Redness of the eyes | ↑ | A common symptom that requires special attention |
VISUAL ACUITY
Visual acuity is one of the most important vital signs of the eye. Without an initial measurement of visual acuity, nothing can be said about the condition of the eye.
1. What is needed to measure visual acuity?
4 simple and easily accessible items are needed: Snellen chart, foramen obturator, pocket charts for testing near vision, charts for testing color vision.
2. What is the Snellen chart?
This is a standard wall table, on which lines of black characters (letters, numbers, or for illiterate people - the letter E) are applied. The characters increase in size from minimum (at the bottom of the table) to maximum (at the top).
3. Who is Snellen?
Hermann Snellen (1834-1908) - Dutch ophthalmologist. He graduated from the university in Utrecht and taught there. Created his famous table in 1862. This was the first attempt to standardize visual acuity measurements.
4. How is visual acuity measured?
Closing one eye at a time, the patient, at the doctor's request, reads a well-lit Snellen chart from a distance of 20 feet (6 m). It is customary to examine the right eye first. The examination can be carried out using glasses for distance vision. Visual acuity is determined by the smallest line on which the patient sees more than half of the letters. In addition, it is necessary to note the number of missing letters on this line. For example, 20/20 - 1 or 20/40 - 2.
5. What does 20/20 mean?
20/20 means that the patient can read from a distance of 6 m (20 ft) the letters that a person with standard vision can read from a distance of 6 m. 20/40 means that the patient can distinguish letters from a distance of 6 m, which can normally be read from 12 m, etc. The numerator here is the distance at which the Snellen chart is located, and the denominator is the distance from which a person with standard vision. The denominator also indicates the smallest line in the table on which the patient was able to read more than half of the letters.
6. Can visual acuity be better than 20/20?
Yes. Although 20/20 is the standard visual acuity, most people can have visual acuity better than 20/20. The patient's visual acuity is recorded as follows: 20/15, 20/12, etc.
7. How is visual acuity measured in illiterate people?
For illiterate people and children, tables containing only the letters E are used. The patient is asked to indicate the direction of the outline of the letter E.
8. How is visual acuity measured in bedridden patients?
Near visual acuity is measured in each eye in turn using special pocket cards - the Rosenbaum Pocket Visual Screener. It can be purchased at any medical equipment store. The card is held 14 inches (35 cm) from the patient's eyes. In this case, one eye of the subject must be closed. Visual acuity is determined by the line with the smallest number of characters, which the patient can clearly distinguish. During the examination, the patient may wear glasses for reading or distance vision. If he does not have glasses or cannot distinguish a nearby card, the examination is replaced by counting the fingers on his hand (see below).
9. How is visual acuity assessed if the patient cannot read a single letter in the table?
If the patient cannot read a single letter in the table, the distance between him and the table is reduced. The reduced distance is recorded in the numerator of the visual acuity formula (for example, 5/70). This expression can be translated into a more familiar notation (for example, 20/280). If the patient cannot read the largest letters on the Snell chart at a distance of 3 feet (1.5 m), visual acuity is assessed by counting the fingers. The researcher indicates the distance from which the patient accurately names the number of fingers shown to him. If this type of measurement of visual acuity is not possible, the assessment is carried out based on the patient’s ability to distinguish between hand movements and flashes of light. The final stage of vision loss is the lack of light perception.
10. What is stenopeic vision?
This is vision through a hole in the obturator. If the patient is unable to read the 20/20 line, an obturator is placed in front of the patient's eye. The stenopeic foramen allows only axial rays to pass through. Peripheral rays, which cause blurring of visual fields in case of refractoriness disorders, do not enter the hole. Thus, an obturator with a stenopeic foramen improves vision in cases where it can be corrected with glasses. For other ocular or neurological diseases (for example, retinal diseases or opacities of the transparent media of the eye), the obturator with a stenopeic foramen does not affect vision. The following diseases can be corrected with glasses: hyperopia (in which the axial length of the eyeball is too short), myopia (in which the axial length of the eyeball is too long) and astigmatism (in which the refractory power of the cornea and lens in one meridian differs from the same indicators in another meridian).
11. Who needs to have visual acuity examined and when?
Measuring visual acuity is the same as assessing the vitality of the eye. Without measuring visual acuity, it is impossible to say anything definite about the condition of the eye. For normal vision, not only the preservation of eye function is required, but also sufficient blood supply and innervation. Visual acuity testing is of great importance during clinical examination. It is performed on all patients complaining of visual impairment. Because loss of visual acuity in one or both eyes may occur unnoticed by the individual, it should be assessed in all adult patients. Impaired visual acuity is usually not accompanied by pain. An exception is diseases accompanied by redness of the eyes (see below). In children, visual acuity should be measured as early as possible (usually after three years of age). This allows amblyopia to be detected at an early age.
12. What does decreased visual acuity mean?
Decreased visual acuity may indicate the presence of any of the following processes.
- Refractive errors that can be corrected (myopia, astigmatism and presbyopia).
- Treatable and reversible blindness (cataract or uveitis).
- Ocular manifestations of systemic diseases that progress without treatment (multiple sclerosis or gliomas).
- Congenital diseases (rubella or toxoplasmosis).
- Infectious diseases (cytomegalovirus retinitis or toxoplasmosis).
13. How are various options for vision loss confirmed?
- Refractive errors correctable with glasses are usually suspected if vision improves with the use of a stenopeic foramen obturator.
- Cloudiness of the light-transmitting media is usually diagnosed by studying the red reflex or during ophthalmoscopy.
- Neurological diseases or retinal lesions - usually detected during ophthalmoscopy, with fluctuations in flashes of light or determination of visual fields.
- Amblyopia is usually confirmed by a history of decreased visual acuity and is often accompanied by strabismus.
14. Which patients with newly diagnosed vision loss are referred to an ophthalmologist?
- Patients with vision complaints.
- Patients with no visual complaints and visual acuity of 20/40 or worse in one or both eyes.
- Patients with a difference in visual acuity between the eyes of two or more lines.
- Middle-aged or elderly patients with presbyopia, even if the distance of visual acuity is preserved (for the selection of reading glasses), as well as for examination for glaucoma.
- Patients with a defect of afferent pupillary fibers.
15. What are tables for studying color vision?
These are pseudochromatic tables in which numbers or figures are presented among colored dots. This combination of colors usually confuses the patient with impaired color discrimination.
16. How is color vision examined?
Color vision charts are presented to the patient sequentially (one eye at a time) and the results are recorded as a fraction (the numerator indicates the number of correct answers and the denominator indicates the number of charts presented). When testing unilateral dyschromatopsia, a simpler but still reliable method is used: the patient is asked to close the affected eye and look at a red object (for example, the red cap of a bottle of mydriatic solution). The patient is then asked to look at the same object with the other eye (the good eye is closed at this time) and report whether the red color looks the same. In patients with dyschromatopsia, the affected eye sees red as gray or washed out.
17. What is dyschromatopsia?
Dychromatopsia (from the Greek dys - pathological, chroma - color, opsis - vision) is a violation of color vision. Dychromatopsia refers to acquired color vision deficiency, as opposed to congenital color blindness.
18. What are the causes of dyschromatopsia?
These are diseases of the optic nerve, as well as toxic or degenerative lesions of the macula.
TRADITIONAL OPINION OF TEACHERS
Visual field testing can reveal important neurological or ocular diseases, but the terminology is very confusing.
19. How are visual fields examined?
The doctor sits at a distance of 1.5 m from the patient and asks him to close one eye with his palm, and fix the other on the doctor’s nose or opposite eye. While the patient fixes his gaze on the indicated point, the doctor extends his hand and quickly raises 1, 2 or 5 fingers. They are held alternately in each square and the patient is asked to name the number of fingers that he sees. The test is then carried out on the other eye. Thus, visual field testing is based on comparison (a rough comparison of the physician's visual fields with the patient's visual fields - see Fig. 19.1).
20. What are the differences between visual field defects in neurological and ocular diseases?
Visual field defects caused by neurological diseases are usually bilateral and spare the vertical midline. Visual field defects resulting from ocular diseases are predominantly unilateral and often do not extend to the horizontal midline.
21. What is the most important step after detecting a visual field defect in one eye?
Check the visual field of the other eye. As mentioned above, unilateral visual field defects are associated with eye diseases. Bilateral visual field defects are usually caused by intracranial (neurological) processes.
22. What is bitemporal hemianopsia?
Hemianopia is understood as the loss of half of the visual fields in both eyes (from the Greek hemi - half, an - deficiency, opsis - vision). Bitemporal hemianopsia is a visual impairment in which the temporal fields of vision of both eyes are lost (bitemporal). Often found with chiasmal tumors (craniopharyngioma in children and pituitary tumors in adults).
23. What is the homonymous hemianopsia?
This is a visual impairment in which the visual fields of both eyes on one side (of the same name) are lost. For example, if the temporal field of the left eye (the left part of the visual field of the left eye) falls out, then the nasal field (the left part of the visual field of the right eye) of the right eye will fall out. Hemianonsia of the same name usually occurs with lesions of the cerebral cortex.
24. What are tunnel fields?
These are severely narrowed visual fields, which are characteristic of advanced glaucoma, retinal pigmentary degeneration and other rarer diseases. Tunnel fields are also found in the simulation of eye diseases.
TRADITIONAL OPINION OF TEACHERS
Extremely valuable information can be obtained by observing the shape, size of the pupils and their response to external stimuli.
25. How are pupils examined?
Ideally, the room should be darkened. The patient fixes his gaze on some distant object. At this time, the doctor illuminates from below with a pen flashlight. Normally, the pupils should be round and equal in size.
26. What do you mainly pay attention to when examining the pupils?
The shape, size and reaction of the pupils to external stimuli are of primary importance. The latter include the reaction of the pupils to light (direct and friendly) and the reaction of accommodation.
27. What are the most common irregularities in the shape of the pupils?
- The most common cause of irregular, pear-shaped pupils is eye surgery (for example, cataract surgery).
- After blunt trauma, tear fluid may collect in the iris sphincters, causing the pupil to appear larger and slightly irregular in shape.
- Inflammation of the iris (iritis) can lead to adhesion (adhesions) of the iris and the anterior lens capsule, and the pupil becomes irregularly shaped.
- Coloboma of the iris is a congenital disease associated with incomplete closure of the embryonic fissure of the optic disc recess. The affected iris has a keyhole shape with a defect in the inferior nasal position.
28. What is hippus?
Hippus is a physiological condition in which the size of the pupils constantly changes. The name comes from the Greek word hippos (horse), reflecting the bouncing motion of a galloping horse. As is normal, with hippus the first reaction of the pupils to light is constriction. This reaction allows one to distinguish hippus from a defect of afferent pupillary fibers (see below).
On a note. With a defect in the afferent pupillary fibers, in response to the approaching light, the pupil first dilates, and with hippus, it narrows.
29. What are the most common causes of uneven pupils?
- The most common cause is physiological anisocoria (from the Greek an - deficiency, iso - equal and core - pupils). This variant of the norm is present in 20% of the population and is characterized by a functional difference in muscle tone in the sphincters of the right and left pupils. With physiological aisocoria, the degree of difference between the pupils does not change with changes in lighting. With physiological anisocoria, there is no ptosis or dissociation in low beam.
- Another common cause of anisocoria is pharmacological dilation. The patient may deliberately or accidentally drop a mydriatic (dilating) solution into the eye, causing pupil dilation. Pharmacologically dilated pupils do not constrict to light even after instillation of cholinergic eye drops (eg, pilocarpine).
- Anisocoria also occurs in Horner's syndrome (see figure on next page). The pupil of the affected eye is smaller in size (miotic). Miosis is accompanied by ipsilateral ptosis and alhidrosis. In anisocoria caused by Horner's syndrome, the degree of difference in pupil size varies depending on the lighting. For example, the difference in pupils is more noticeable in a darkened room (impaired dilatation) and less noticeable in bright light (the ability to constrict is not impaired).
- Anisocoria in patients with third cranial nerve palsy is caused by mydriasis (dilation) of the pupil on the affected side. With third nerve palsy, ptosis and weakness of all external ocular muscles are also detected, with the exception of the rectus lateral and superior oblique muscles. The dilated pupil constricts when cholinergic eye medications are instilled. With anisocoria associated with third cranial nerve palsy, the difference between the pupils is more noticeable in bright light (the ability to constrict is impaired).
- Other causes of anisocoria include inflammatory processes (unilateral iritis), old trauma, an acute attack of closed-angle glaucoma, previous eye surgeries and various neurological diseases.
Rice. 4.1. Ptosis and miosis on the left (Horner's syndrome) . Note that the left lower eyelid is located above the right lower eyelid. This inversion ptosis occurs due to a violation of the sympathetic innervation of the muscle of the lower eyelid - an analogue of the Müller muscle. (Reproduced with permission from: Vander JF, Gault JA: Ophthalmology Secrets. Philadelphia, Hanley and Belfus, 1998.)
30. What is the reaction to accommodation?
Constriction of the pupil occurs following a shift in gaze fixation from a distant object to a closer one. To test the accommodation response, ask the patient to look at a distant point and then quickly focus on a much closer object (for example, the examiner's finger). Returning the gaze to a distant point causes rapid dilation of the pupil.
31. What is a reaction to light?
When you shine light into the eye, the pupil constricts. The reaction to light can be direct (when it occurs in the same eye into which the light is directed) or conjugate (develops on the opposite side).
32. What are Argyll Robertson's pupils?
Argyll Robertson's pupils constrict only in response to accommodation, but do not constrict to light (low beam dissociation). Characteristic of tertiary syphilis. They are also found in diabetes mellitus and alcoholism (Wernicke encephalopathy) and in patients with various neoplastic, infectious and degenerative processes in the central nervous system. Argyll Robertson's pupil always indicates a pathological process.
33. Who is Argyll Robertson?
Argyll Robertson (1837 - 1909) was a Scottish physician. Passionate golfer. Studied in Berlin. After returning to his native Scotland, he founded and
Headed the Department of Ophthalmology at the University of Edinburgh. Was Marcus Gunn's teacher and mentor (see question 39).
34. What is Eday's pupil?
This is a tonic pupil that usually does not constrict to either accommodation or light. After a long attempt at accommodation, the pupil eventually contracts, but always slowly. When the tension expended on accommodation is relieved, the pupil slowly dilates again. Adai's pupil is usually observed on one side, is often dilated, oval in shape and is always benign. Hypersensitive to pilocarpine solution (0.125%).
Rice.
4.2. Edai's tonic pupil on the right. A. Anisocoria: the right pupil is larger than the left. B. The right pupil constricts in response to accommodation. B. The right pupil reacts poorly to light. D. The right pupil constricts markedly when 0.125% pilocarpine is instilled, whereas the left pupil does not constrict. (Adapted with permission from: Tasman W., Jaeger E. A. (eds): The Wills Eye Hospital Atlas of Clinical Ophthalmology. Philadelphia, Lippincott-Raven, 1996, p 298.)
35. Who is Adai?
William Aday (1886 - 1935) was an Australian who studied medicine at Edinburgh and graduated at the outbreak of the First World War. He was drafted into the army and fought honorably in France, where he saved several young soldiers from a gas attack using a makeshift urine-soaked cloth mask. He fell ill with measles in time, and this saved him from the subsequent bloody massacre, during which his entire regiment died. He returned to England, where he taught and practiced medicine until his death. His name is associated not only with the description of Eday's pupil, but also with the first description of narcolepsy. Adai was a charismatic teacher, an avid skier, and an amateur bird watcher. He died suddenly at the age of 49 from a myocardial infarction.
36. What is the oscillating light flash test?
This pupillary light response test is usually performed to quickly diagnose a Marcus Gunn pupil or an afferent pupillary fiber defect. The patient is asked to look at some distant object. Using a pen-flashlight, first one and then the other eye are illuminated. When hesitating
light from one eye to the other, each pupil quickly narrows. When the optic nerve is damaged or there is massive damage to the retina of one eye, the pupil dilates to light rather than constricts.
The pupil of Marcus Gunn is characterized by a defect in the afferent pupillary fibers and preservation of the efferent pathways. Afferent stimulation of the healthy eye is stronger than afferent stimulation of the affected eye. Therefore, when light moves from the healthy eye to the diseased eye, the stimulus for pupil constriction (coming from the healthy eye) is suppressed. As a result, when light moves from the normal eye to the affected eye, the latter's pupil dilates. In such cases, it is usually said that a Marcus Gunn pupil (MGP) or afferent pupillary fiber defect (APD) is observed.
Rice. 4.3. DAZV on the left. A. In dim lighting, the pupils are the same size. B. Light directed into the left eye causes a partial and delayed constriction of each pupil. B. Light directed into the right eye causes a lively normal reaction in both pupils. D. Light quickly directed into the left eye causes both pupils to dilate. (Adapted with permission from: Tasman W., Jaeger E. A. (eds): The Hospital Atlas of Clinical Ophthalmology. Philadelfia, Lippincott-Raven, 1996, p 297.)
37. What is the reaction of Marcus Gann's pupil to initial exposure to light?
When the affected pupil is initially exposed to light (the first stage of the study with oscillating flashes of light), the pupil slightly constricts. On the other hand, when light fluctuates from one eye to the other, Marcus Gunn's pupil dilates.
38. What is the common cause of Marcus Gann pupil?
The usual cause is optic neuritis. However, not only any asymmetric lesion of the optic nerve, but also massive damage to the retina (for example, occlusion of the central retinal artery) can lead to the development of a defect in the afferent pupillary fibers.
39. Who is Marcus Gunn?
Robert Marcus Gunn is a Scottish ophthalmologist. He was personally acquainted with another famous Scot, Robert Louis Stevenson. He was attracted to the study of ophthalmology by Argyll Robertson (see above). He became widely known for his mastery of the ophthalmoscope.
Is eye loss in dogs literal?
It is important to note that eyeball prolapse in dogs should be understood figuratively and not literally. In fact, the organ itself still remains inside the eye socket, but is displaced from its original position and comes out from under the eyelids. Because of this, it seems that it is about to fall out.
When the position of the eyeball changes, its cornea, conjunctiva and retina are most vulnerable to external factors. Without timely help, their tissues begin to die, leading to partial and then complete loss of visual function.
OUTER EYE
TRADITIONAL OPINION OF TEACHERS
Many outdoor studies are carried out using a flashlight pen. You should carefully examine the orbits, the position of the eyelids, the conjunctiva, the anterior chamber of the eye and examine the corneal reaction to light.
Tears
40. What is the Schirmer test?
The Schirmer test aims to measure tear production. It is carried out to determine dry eyes due to keratoconjunctivitis or Sjögrep syndrome. Sjögren's syndrome is an autoimmune disease characterized by dry eyes and dry mouth. Often accompanied by other autoimmune disorders.
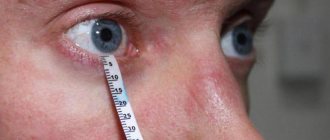
41. What is the Schirmer test?
Under local anesthesia, the doctor inserts a small strip of filter paper under the lower eyelid on the medial or lateral side. The test strip should not be in the center. After 5 minutes it is removed. The wet spot formed by tears is measured in millimeters. Normally, its dimensions correspond to 15 mm (before 40 years) and 10 mm (after 40 years). A distance of less than 5 mm usually indicates decreased tear production. A distance from 5 to 10 mm is suspicious for its decrease.
42. Who is Schirmer?
Otto Schirmer (1864-1917) was a German ophthalmologist.
Brows
43. What is the significance of thinning or absence of the lateral portion of the eyebrows?
Thinning or absence of the lateral portion of the eyebrows is a common symptom of hypothyroidism (often called the “Queen Anne sign” after a famous patient). However, it may also be a variant of the norm. The appearance of eyebrows can also be the result of cosmetic manipulation (plucking). Other causes include medications, skin diseases, and lupus.
Eyelids and orbits
44. What is xanthelasma?
Xanthelasma (from the Greek words xanthos - yellow and elasma - forged metal plate) is a yellowish fatty deposit located on top of the eyelid. Most patients with xanthelasma do not have lipid metabolism disorders. However, xanthelasmas occur in 25% of patients with type 3 hyperlipoproteinemia and also occur in the more common types 2 and 4 hyperlipoproteinemia. If xanthelasmas are a cosmetic problem, they are removed surgically.
Rice. 4.4. A patient with xanthelasmas on all four eyelids. (Reproduced with permission from: Tasman W., Jaeger E.L.: The Wills Eye Hospital Atlas of Clinical Ophthalmology. Philadelphia, Lippincott - Raven, 1996.)
45. What is ectropion?
This is eversion (outward turning) of the lower eyelid. Often found in older people. In this case, the edge of the dorsal conjunctiva opens to external stimuli. Exposed corneas and keratinization of the exposed conjunctiva can lead to eye irritation.
46. What is entropion?
This is an inversion (inward folding) of the lower eyelid. Often occurs in old age. May also cause mechanical irritation to the eye due to contact with eyelashes.
47. What is barley?
This is an acute focal inflammatory process in one of the glands located along the edge of the eyelid (for example, a hair follicle). Classic signs are redness, swelling, tenderness and sometimes purulent discharge.
48. What is blepharitis?
This is a diffuse inflammatory process that involves the edge of the eyelid. Characterized by swelling and redness. Blepharitis is usually caused by Staphylococcus aureus or Staphyloccocus epidermidis and may be hypersusceptible. The edge of the eyelid may become crusty, covering the eyelashes. Patients often complain of dry eyes.
49. What is ptosis?
Ptosis (fall in Greek) is the drooping of the upper eyelid. Can be one- or two-sided.
Rice. 4.5. Involutional (aponeurotic) ptosis, too mild to smooth out the depth of the eyelid folds. The function of the levator muscle is usually preserved. (Reproduced with permission from: Tasman W., Jaeger E.A.: The Wills Eye Hospital Atlas of Clinical Ophthalmology. Philadelphia, Lippincott - Raven. 1996.)
50. What are the causes of ptosis? How are they differentiated?
Common reasons include age (1); consequences of injuries and surgical procedures (2) and congenital causes (3). Less commonly, ptosis is caused by myasthenia gravis (1), Horner's syndrome (2), and third cranial nerve palsy (3). These reasons differ from the first three in the presence of a combined pathology: changes in the size of the pupils and paresis of other cranial nerves.
51. What is proptosis?
Proptosis (or exophthalmos) is an abnormal protrusion of one or both eyeballs (from the Greek word proptosis, meaning prolapse forward). Normally, the eyeballs can protrude forward by 19 - 24 mm, depending on race and gender. If one eye protrudes forward by more than 2 mm compared to the other eye, we speak of unilateral exophthalmos.
52. What are the most common causes of proptosis in adults?
The most common cause of unilateral exophthalmos is thyroid ophthalmopathy (Graves' disease). In second place are space-occupying formations (metastatic or primary tumors, malignant and benign). The main cause of bilateral exophthalmos is also Graves' disease. Next come cancer.
53. What are other signs of ophthalmopathy in thyrotoxicosis?
- Retraction of the eyelids (thyroid gaze).
- The upper eyelid lags behind when looking down (van Greif sign).
- Conjunctival edema (chemos) and hyperemia.
- Rare blinking and proitosis (Stellwag's sign).
- Slight tremor of loosely closed eyes (Rosenbach's sign).
- Violation of eye convergence following accommodation from a distance of 12.5 cm (Moebius sign).
- Weakening of extraocular mobility.
- Ulceration of the cornea.
- Compression of the optic nerve, leading to swelling and loss of vision.
Rice. 4.6. Ophthalmopathy in thyrotoxicosis with proptosis and eyelid retraction. (Reproduced with permission from: Vander JF, Gault JA: Ophthalmolo do Secrets. Philadelphia, Hanley and Belfus, 1998.)
54. What is the most common cause of unilateral proptosis in children?
The most common cause is cellulitis. Of the space-occupying lesions, unilateral exophthalmos in children is most often caused by rhabdomyosarcoma.
55. What are the differences between preseptal and orbital cellulitis? Preseptal cellulitis affects only the eyelids, which become red and swollen. The process does not affect either the orbital septum or its structures. There is no impression that the patients' ocular system is affected. Vision, pupils, conjunctivae and eye mobility remain normal.
In contrast, orbital cellulitis is an emergency. It affects not only the eyelids, but also the orbital structures. Patients give the impression of being systemic patients. Numerous symptoms include pain with eye movement (O); redness and swelling of the eyelids (2); conjunctival injection and chemosis (swelling) (3); limited eye movement on the affected side (4); proptosis (5); decreased vision (6 ); defect of afferent pupillary fibers (7).
56. What are the signs of an orbital fracture?
This is a fracture of the orbital floor (which is also the roof of the maxillary sinus). The inferior orbital rectus muscle may become impinged. In patients with blunt orbital trauma, the orbital rim should be palpated for mobility or discontinuity. The surrounding soft tissue should also be carefully palpated for subcutaneous crepitus. The latter is caused by air coming from the damaged maxillary sinus. Air bubbles are sometimes visible on the conjunctiva when illuminated with a flashlight. Patients also need to check the sensitivity on the side of the injury in the area of distribution of the 5th cranial nerve. Loss of sensation indicates a fracture. When the inferior rectus muscle is pinched, the patient cannot look up or complains of diplopia when looking up.
57. What is enophthalmos?
Enophthalmos is the opposite of exophthalmos (literally falling inward). The eyes are immersed in the orbits rather than protruding from them. Enophthalmos may result from extensive fracture of the orbit.
Rice. 4.7. Pseudoptosis in a patient with an orbital fracture. (Reproduced with permission from: Tasman W., Jaeger E.L.: The Wills Eye Hospital Atlas of Clinical Ophthalmology. Philadelphia, Lippincott - Raven, 1996.)
Causes and symptoms of eye loss
Although there are benefits, any dog can be affected, so it is important to know the main causes of eye loss and the symptoms of the disease.
The following factors can provoke proptosis:
- sudden jumps;
- ophthalmological diseases that weaken or deform the muscles of the eyeball;
- an excessively tightened collar or sharp tugging on the leash. Remember that your index finger should fit freely between the collar and the animal's neck.
- eye injuries caused by contact with a dry branch or blade of grass;
- prolonged constipation;
- mechanical injuries to the temporal part of the skull or cervical spine;
- using the scruff of the neck to lift an adult animal. Only puppies can be carried by the scruff of the neck; in other cases, the animal will suffer a cervical injury. Special attention should be paid to Shar Pei owners.
- insect bites;
- high temperatures;
- stressful situations.
Be sure to contact your veterinarian if:
- eye bleeding;
- photophobia;
- increased blinking frequency;
- protrusion of at least one eyeball;
- puffiness or swelling of the conjunctival membrane;
- dryness on the cornea;
- anxious and depressed state.
If your pet's breed is at risk, it should be examined if there is any suspicion.
Otherwise, the dog may develop strabismus, lose visual acuity, or remain completely blind.
Small animals easily get serious injuries when falling from sofas or getting caught in the corner of an open door
Extraocular movements
58. What is the diagnostic value of studying extraocular movements?
Small. Although no eye examination is complete without measuring these movements, the informative value of this test is very low (especially if there are no complaints of double vision). On the contrary, if an adult suddenly develops squint or complains of double vision, this may indicate a serious illness. Therefore, such patients should be immediately referred to a specialist. For information on strabismus and pseudostrabismus, see the Corneal Response to Light section in this chapter.
Nystagmus
59. What is nystagmus?
This is a neurological simititis characterized by pathological rhythmic movements of the extraocular muscles. The Greek word nystagmos literally means rocking. Rocking movements can be observed in both horizontal and vertical planes and include fast and slow phases.
60. What is the clinical significance of nystagmus?
Nystagmus usually indicates dysfunction of one or more of three structures: the cerebellum (1), the vestibular system (2), or the oculomotor system (3). Dysfunction may be associated with toxic-metabolic causes or anatomical damage, and may also be congenital.
61. What are the main types of nystagmus?
The classification of nystagmus is based on the direction of eye movement. There are three types of nystagmus: horizontal, vertical and rotational. On the other hand, physiological nystagmus is fast and slow eye movements that can be observed in a person on the road (especially on a train). The traveler's gaze is fixed on quickly approaching objects (for example, telephone poles). This nystagmus is a normal reaction of the eyes. It can be induced by asking the patient to stare at a rapidly rotating drum with vertical stripes (optokinetic nystagmus).
What to do if your eyeball falls out
Only surgery can save your beloved pet. Before going to the veterinarian, you can help the animal.
Metis (dog): what is it, a cross between different breeds
What the owner can do:
- calm down yourself and calm the dog;
- rinse the damaged area with clean water;
- for 10 min. apply a cold compress to the sore spot;
- put a surgical (Elizabethan) collar on your pet;
- moisten the bandage with saline solution and bandage the wound. Moisten the bandage periodically to prevent it from drying out.
If your dog's eyes have fallen out, you need to go to the veterinary clinic as soon as possible. This disease can only be cured by surgery. The veterinarian will perform surgery on the animal: realign the eyeballs and tighten the extraocular muscles.
Important! Under no circumstances should you attempt to treat your dog yourself.