Causes
In most cases, peripheral chorioretinal dystrophy is a hereditary disease. A high risk of development is provoked by the presence of myopia. Rarely, the pathology may occur as a consequence of farsightedness. Such disorders may be systemic or related to ocular pathologies. Main reasons for development:
- genetic predisposition, presence of PVCD in parents;
- myopia;
- inflammatory processes;
- injuries;
- complications after operations;
- diabetes;
- intoxication of the body;
- viral diseases;
- disorders of the cardiovascular system;
- prolonged exposure to the sun without the necessary protection;
- vitamin deficiency.
Young people often face such a lesion due to severe myopia.
Causes of peripheral retinal dystrophy
There are types of dystrophy, the development of which is due to hereditary predisposition. Some are formed under the influence of external factors. It is important to note that the risk group includes people with diabetes mellitus, and also those suffering from myopia (less commonly, farsightedness).
The following can trigger the development of the disease:
- Severe poisoning
- Inflammatory process in the eyes
- Injuries (craniocerebral, visual organs)
- Complications after surgery
- High blood pressure (hypertension)
- Vascular pathologies
- Acute viral infections
- Chronic vitamin deficiency
- Alcohol and smoking abuse.
- Sunburn
The chance of vision impairment due to retinal dystrophy is the same for men and women, and increases with age. Why is that? To answer this question, you need to understand where the disease begins.
Risk group
People who have severe myopia are at risk. With myopia, the eyeball grows in length. The retina also stretches and becomes excessively thin. At the same time, it is exposed to various diseases, especially dystrophic changes.
The risk of developing such lesions is present in older people. Predisposition appears with hypertension and atherosclerosis. Such diseases cause a deficiency of oxygen and nutrition of the retina. Against this background, dystrophy develops.
Causes
Retinal rupture or detachment has dire consequences that should be prevented. But what are the causes of the disease? There are reasons that indirectly indicate the possibility of developing PCVRD and PCRD.
- Received eye injuries that went unattended. After the redness or swelling went away, the patient stopped seeing an ophthalmologist. Meanwhile, the retina may have been damaged.
- Previous infections.
- Inflammatory diseases occurring on the outer and inner eyelids.
- Hereditary predisposition.
- Vascular diseases such as diabetes, hypertension, hypotension and so on.
- Myopia in any form.
It is almost impossible to independently identify dystrophy until irreversible pathological processes begin. Therefore, if the above circumstances occur in your life, be sure to visit an ophthalmologist. This should be done at least once a year as a preventive visit. The fundus of the eye will be examined with a Goldmann lens, which will allow pathologies to be identified at the earliest stages.
At-risk groups
Scientists have found that approximately 40% of people who suffer from myopia (myopia) are at risk for developing PVCD. But why is this happening?
Myopia is a progressive disease. This is why the stretching of the retinal tissue increases. Gradually, the posterior pole of the eye begins to be involved in this process, and because of this, hemodynamics are disrupted. Metabolic processes are also disrupted, resulting in the formation of areas on the retina that rapidly become thinner.
First, there is no proper nutrition in these places, and then ruptures occur. Unfortunately, this process occurs without symptoms. However, when a person begins to realize that he is rapidly losing his vision, at an appointment with an ophthalmologist it turns out that a detachment has occurred.
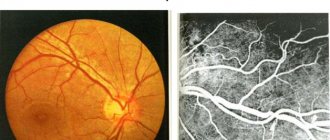
Classification
Considering the nature of the pathology, dystrophic changes are divided into several types. Only an ophthalmologist can do this after a thorough examination of the fundus. With the help of ophthalmoscopy, you can examine the condition of the retina from the inside.
Classification:
- Lattice dystrophy. In most cases, this form of pathology has a disappointing prognosis. With its development, retinal detachment and loss of visual perception are observed. The disease tends to develop slowly. Therefore, progression can last throughout life. This form of lesion gets its name because white stripes, similar to a lattice, appear on the fundus of the eye.
- Type of snail trail. Occurs against the background of severe myopia. Point defects appear on the retina. In appearance, it resembles snail tracks. This type of dystrophy leads to rupture and detachment of the retina.
- Frost-like. Pathology occurs due to genetic predisposition. Frost-like dystrophy is accompanied by the appearance of white deposits on the retina. This visually resembles snow or frost.
- Type of cobblestone pavement. This type of PCRD does not apply to dangerous pathologies. In most cases it affects older people. Not accompanied by severe symptoms.
- Retinoschisis. Hereditary form of the disease. Accompanied by retinal dissection and cyst formation. The danger of damage lies in the absence of symptoms.
- Small cystic. With such a lesion, a large number of small cysts appear that affect the fundus of the eye. The prognosis is favorable.
Symptoms
At the first stage of development, PVCRD is not accompanied by characteristic symptoms. Rarely, floaters may appear before the eyes. If lateral vision is impaired, the patient will not be able to determine the presence of such a pathology for a long time. As it progresses, a person may notice that they need brighter light when reading. Then other signs may appear.
The main symptoms of dystrophic lesions:
- blurred vision;
- decreased visual acuity at night;
- the appearance of black or multi-colored spots before the eyes;
- narrowing of visual fields;
- distortion of the contours of objects.
A tear or detachment of the retina is accompanied by the appearance of bright flashes before the eyes. This interferes with normal vision. If such symptoms occur, you should immediately consult an ophthalmologist. Rarely, both eyes are affected.
Symptoms of chorioretinal dystrophy
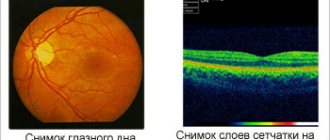
There are two forms of CCRD: non-exudative (dry, atrophic) and exudative (wet).
Dry non-exudative dystrophy is an early form of the disease and occurs in 85-90% of cases. Characterized by metabolic disorders between the vessels and the retina. Between the basal layer formed by the vascular and retinal membranes and the retinal pigment epithelium, colloidal substances (decomposition products) accumulate, pigment redistribution and atrophy of the pigment epithelium occur.
The disease begins asymptomatically and progresses slowly. Visual acuity remains normal for a long time, but curvature of straight lines, bifurcation, and distortion of the shapes and sizes of objects may be noted. Gradually, blurriness of the image appears when looking directly (as if through a layer of water), visual acuity begins to decrease. This process may stabilize at some stage, but can also lead to complete loss of central vision.
In the second eye, the disease begins to develop no later than five years after the first eye is affected. In 10% of cases, dry dystrophy turns into a more severe wet form. In this case, fluid (blood) penetrates through the walls of the newly formed vessels and accumulates under the retina.
Exudative dystrophy has four stages of development:
- Detachment of the pigment epithelium. Visual acuity is preserved, mild manifestations of farsightedness or astigmatism, the appearance of fog or cloudy spots before the eyes are possible. The process may develop in reverse (adhesion of detachment sites).
- Neuroepithelial detachment. To the above symptoms is added a significant decrease in vision, up to the loss of the ability to read and write. Blurred boundaries and swelling of the detachment zone, pathological proliferation of blood vessels are noted.
- Hemorrhagic detachment of pigment and neuroepithelium. Vision remains low. A large pink-brown focus of pigment accumulation with clear boundaries is formed. The cyst-like retina protrudes into the vitreous body. When newly formed vessels rupture, hemorrhages occur.
- Scar stage. At the site of the lesion, fibrous tissue forms and a scar forms.
Diagnostics
Diagnostics is aimed at determining the type of pathology and the reasons for its development. The following examination methods are used:
- determination of visual acuity to exclude or confirm myopia;
- determination of visual fields using perimetry;
- measurement of intraocular pressure;
- electrophysiological examination;
- biomicroscopy;
- use of a Goldmann lens for fundus examination.
After examination, the doctor can determine whether peripheral vitreochorioretinal dystrophy or another type of pathology affects the retina. Once the cause of such changes is determined, drug therapy can be prescribed.
Treatment
The disease has several types. Treatment is prescribed taking into account the form of the pathology and the degree of its damage. A variety of methods are used for treatment:
- wearing glasses or contact lenses to correct vision and make the patient’s life easier;
- laser treatment;
- drug therapy.
Laser treatment is carried out to prevent retinal detachment. This is necessary for patients at risk of developing such complications. Reasons for laser coagulation:
- risk of retinal detachment;
- genetic predisposition to the development of pathology;
- lack of lens;
- presence of an implant;
- severe stage of myopia;
- systemic diseases;
- progression of dystrophy;
- presence of neoplasms.
In other cases, laser treatment is not used. The procedure is carried out exclusively in a hospital. The patient is prohibited from visual stress for a week. For drug treatment, the following drugs are prescribed:
- antioxidants;
- vitamin complexes to improve metabolic processes in the retina;
- drugs to strengthen the walls of blood vessels.
Vitreochorioretinal dystrophy requires special attention from the patient. The success of treatment will depend on this. Physical activity should be limited. This can cause retinal detachment. In some cases, a change in work activity may be necessary.
Patients with such lesions are registered in the hospital. They should visit an ophthalmologist every six months for a routine examination. After laser treatment, it is prohibited to begin work earlier than two weeks. With timely treatment, the result will be successful.
Complications
These pathologies have 2 types of complications – retinal rupture and detachment. If the development of dystrophy is not detected in time, vision may deteriorate. Often this process is irreversible. By regularly visiting an ophthalmologist, the risk of complications is significantly reduced. Therefore, if any symptoms appear, you should consult a doctor.
The development of complications depends on the type of lesion. In some cases, even with timely diagnosis, they cannot be avoided.
Prevention
There are no specific preventive measures to prevent dystrophic changes. With the help of some recommendations, you can only reduce the risk of developing PVCD. The main prevention consists of proper nutrition and timely examination by a doctor. It is also important to do eye exercises, especially after prolonged exercise. In sunny weather, be sure to wear safety glasses. They protect the eyes from ultraviolet radiation, which has a negative effect on vision.
This pathology mainly affects older people. This is associated with the aging of the body and the development of diseases of the cardiovascular system. Dystrophy also occurs against the background of severe myopia. Therefore, it is important to diagnose myopia early and treat it. Correction with optical products may be necessary. They are selected by the doctor individually for each patient.
To treat dystrophy, medications, physiotherapy, laser treatment and surgery are used. Each method is prescribed taking into account the form of pathology and the stage of the lesion. Laser coagulation is considered effective. This method helps stop the development of pathological processes and is considered safe for the patient.
PVHRD during pregnancy
During the gestation period, the immune system weakens, as a result of which the likelihood of developing various degenerative processes increases. If a pregnant woman has been diagnosed with PVCRD of the eye, then laser coagulation is prescribed. In the absence of contraindications, the operation is possible at any time, but it is not recommended to do it later than 31 weeks.
According to medical organizations, by the beginning of the reproductive period, more than 25% of women have myopia, more than 7% of them have a high degree. Against the background of a normal pregnancy, women with myopia experience a narrowing of the retinal vessels.
This occurs due to the increased load on the cardiovascular system and the need for additional blood circulation for the unborn child. Therefore, during pregnancy, patients are examined twice by an ophthalmologist with a complete examination of the fundus.
The need for a cesarean section during pregnancy of a woman with retinal PVCRD is determined one month before the estimated date of birth.
The decision on the need for a cesarean section due to degenerative conditions of the retina is made a month before birth. A high degree of myopia (more than 6.0 diopters) is not an indication for surgery.
Ophthalmologists recommend cesarean section after laser photocoagulation at more than 32 weeks or in the presence of PVCRD in one sighted eye.