Glomerulonephritis is a series of immunoinflammatory diseases with different morphologies, in which the glomeruli are mainly affected with the obligatory involvement of tubules and interstitial tissue. These can be either independent diseases or part of systemic diseases, such as systemic vasculitis, systemic lupus erythematosus, infective endocarditis, etc.
- Classification (types) of glomerulonephritis
- Etiology (causes)
- Acute post-streptococcal glomerulonephritis Symptoms and diagnosis
- Treatment
- Treatment of complications
- Clinical examination
Classification (types) of glomerulonephritis
There are many divisions of these diseases, which can be based on the following parameters:
- variant of the course (acute, chronic and rapidly progressive)
- main syndrome (nephrotic, hypertensive, mixed, hidden/latent)
- type of morphological changes
According to morphology there are the following types:
- mesangioproliferative
- intracapillary
- focal segmental glomerulosclerosis
- mesangiocapillary
- minimal change nephropathy
- membranous nephropathy
- rapidly progressive
As a result of each of the above forms, the development of generalized fibrosis of the renal tissue is likely, which clinically corresponds to chronic renal failure.
↑ Pathological anatomy
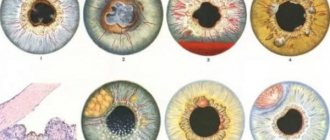
According to the topography of the process, intra- and extracapillary forms are distinguished; according to the nature of inflammation - exudative, proliferative (productive) and mixed.
↑ Intracapillary glomerulonephritis
Intracapillary glomerulonephritis, which is characterized by the development of a pathological process in the vascular glomerulus, can be exudative, proliferative or mixed. Intracapillary exudative glomerulonephritis is spoken of when the mesangium and capillary loops of the glomeruli are infiltrated by neutrophils, and intracapillary proliferative (productive) is when proliferation of endothelial and especially mesangial cells is noted, the glomeruli increase in size and become “fingered.”
↑ Extracapillary glomerulonephritis
Extracapillary glomerulonephritis, in which inflammation develops not in the vessels, but in the cavity of the glomerular capsule, can also be exudative or proliferative. Extracapillary exudative glomerulonephritis can be serous, fibrinous or hemorrhagic; Extracapillary proliferative glomerulonephritis is characterized by proliferation of glomerular capsule cells (nephrothelium and podocytes) with the formation of characteristic crescents.
Based on the prevalence of the inflammatory process in the glomeruli, diffuse and focal glomerulonephritis are distinguished.
Morphological changes in the kidneys during glomerulonephritis concern not only the glomerular apparatus, although glomerulitis is the leading one in assessing the process, but also other structural elements - tubules, stroma, vessels. In this regard, glomerulonephritis is distinguished with a tubular, tubulo-interstitial or tubulo-interstitial-vascular component. Depending on the nature of the course, as already mentioned, acute, subacute and chronic glomerulonephritis are distinguished. The pathological anatomy of each of them has its own characteristics.
↑ Acute glomerulonephritis
Acute glomerulonephritis, which is usually caused by streptococcus (post-streptococcal, bacterial, glomerulonephritis), and the pathogenesis is associated with circulating immune complexes (immune complex glomerulonephritis), can last 10-12 months. In the first days of the disease, glomerular hyperemia is pronounced, which is quickly joined by infiltration of the mesangium and capillary loops by neutrophils. It reflects the reaction of leukocytes to heterologous complement-containing immune complexes. All renal glomeruli are involved in the process. Soon proliferation of endothelial and especially mesangial cells appears, and the exudative reaction decreases. When leukocytes predominate in the glomeruli, they speak of an exudative phase; when proliferation of glomerular cells is combined with leukocyte infiltration, they speak of an exudative-proliferative phase; with a predominance of proliferation of endothelial cells and mesangiocytes, they speak of a proliferative phase of acute glomerulonephritis.
Sometimes in severe cases, acute glomerulonephritis has morphological changes characteristic of necrotizing glomerulonephritis: fibrinoid necrosis of the capillaries of the glomerulus and afferent arteriole along with capillary thrombosis and infiltration of neutrophilic leukocytes.
In acute glomerulonephritis, the kidneys are slightly enlarged and swollen. The pyramids are dark red, the bark is grayish-brown with small red speckles on the surface and cut or with grayish translucent dots (variegated bud). However, in some cases (death in the first days of the disease), the kidneys at autopsy may appear completely unchanged and only histological examination reveals diffuse glomerulonephritis.
Kidney changes characteristic of acute glomerulonephritis are often completely reversible. However, in some cases they persist for more than a year (acute extended glomerulonephritis) and can transform into chronic.
↑ Subacute glomerulonephritis
Subacute glomerulonephritis develops due to damage to the glomeruli of the kidneys by both circulating immune complexes and antibodies. It progresses quickly (rapidly progressive glomerulonephritis), and renal failure occurs early (malignant glomerulonephritis). Extracapillary productive changes in the glomeruli are characteristic - extracapillary productive glomerulonephritis. As a result of proliferation of the capsule epithelium (nephrothelium), podocytes and macrophages, crescent formations (“crescents”) appear, which compress the glomerulus. The capillary loops undergo necrosis, and fibrin thrombi form in their lumen. Fibrin masses are also found in the capsule cavity, where they enter through microperforations of the capillary membranes. Accumulations of fibrin in the cavity of the glomerular capsule contribute to the transformation of epithelial “crescents” into fibrous adhesions or hyaline fields. Changes in the glomeruli are combined with severe degeneration of nephrocytes, edema and infiltration of the renal stroma. Sclerosis and hyalinosis of the glomeruli, tubular atrophy and fibrosis of the renal stroma occur early.
The kidneys in subacute glomerulonephritis are enlarged, flabby, the cortex is wide, swollen, yellow-gray, dull, speckled with red and well demarcated from the dark red medulla of the kidney (large variegated kidney) or red and merges with the full-blooded pyramids (large red kidney ").
↑ Chronic glomerulonephritis
Chronic glomerulonephritis is an independent disease that occurs latently or with relapses, sometimes stretching for many years and ending in chronic renal failure. The cause of the development of chronic glomerulonephritis is usually unclear, but the mechanism of its development is well studied: in 80-90% of cases it is associated with circulating immune complexes. Chronic glomerulonephritis is represented by two morphological types - mesangial and fibroplastic (sclerosing).
↑ Mesangial glomerulonephritis
Mesangial glomerulonephritis develops due to the proliferation of mesangiocytes in response to deposits under the endothelium and in the mesangium of immune complexes. In this case, there is an expansion of the mesangium of the vascular bundle of the glomeruli and the accumulation of matrix in it. During the proliferation of mesangiocytes, their processes migrate to the periphery of the capillary loops (interposition of mesangium), which leads to “detachment” of the endothelium from the membrane and under a light microscope is defined as thickening, double-circuiting or splitting of the basement membrane of the capillaries. Depending on the severity and nature of changes in both the mesangium and the walls of the glomerular capillaries, mesangioproliferative and mesangiocapillary variants of mesangial glomerulonephritis are distinguished.
In mesangioproliferative glomerulonephritis, the clinical course of which is relatively benign, proliferation of mesangiocytes and expansion of the mesangium are noted without significant changes in the walls of the glomerular capillaries. Mesangiocapillary glomerulonephritis, characterized by the rather rapid development of chronic renal failure, is characterized not only by pronounced proliferation of mesangiocytes, but also by diffuse damage (thickening and splitting) of the glomerular capillary membranes due to mesangial interference. Sometimes, due to the proliferation of mesangiocytes and an increase in the mesangial matrix in the center of the lobules, the capillary loops are shifted to the periphery and compressed, which determines early hyalinosis of the vascular lobules of the glomeruli. In such cases, we speak of lobular glomerulonephritis as a type of mesangiocapillary.
Mesangial glomerulonephritis is characterized by changes not only in the glomeruli, but also in the tubules (dystrophy, atrophy) and stroma (cellular infiltration, sclerosis).
Kidneys with mesangial glomerulonephritis are dense, pale, with yellow spots in the cortex.
↑ Fibroplastic glomerulonephritis
Fibroplastic (sclerosing) glomerulonephritis is a collective form in which sclerosis and hyalinosis of capillary loops and the formation of adhesions in the capsule cavity complete the changes characteristic of other morphological types of nephritis. In cases where the majority of glomeruli undergo fibroplastic transformation, they speak of diffuse, and some of the glomeruli - of focal fibroplastic glomerulonephritis. With fibroplastic glomerulonephritis, especially diffuse, dystrophic and atrophic changes in the tubules, sclerosis of the stroma and blood vessels of the kidneys are pronounced.
Kidneys with fibroplastic (diffuse) glomerulonephritis may be slightly reduced, with small recesses emerging on the surface; they are usually dense, gray-red.
Chronic glomerulonephritis, as a rule, undergoes evolution into secondary (nephritic) shrinkage of the kidneys (secondary shrinkage of the kidneys). The size of the buds decreases, they become dense, their surface is fine-grained (with uniform wrinkling - smooth). The granular nature of the surface of the kidneys is explained by the fact that areas of sclerosis and atrophy (retraction) alternate with areas of hypertrophied nephrons (bulging). On the section, the layer of renal tissue is thin, and the cortical substance is especially thinned; The kidney tissue is dry, anemic, gray in color.
On microscopic examination, atrophy of the glomeruli and tubules and their replacement with connective tissue are noted in the sunken areas. The glomeruli turn into scars (glomerulosclerosis) or hyaline balls (glomerulohalinosis). In the bulging areas, the glomeruli are somewhat hypertrophied, their capsule is thickened, and the capillary loops are sclerotic. The lumen of the tubules is expanded, their epithelium is flattened. Arterioles are sclerotic and hyalinized. In small and medium-sized arteries, fibrosis and intimal hyalinosis are observed, sclerosis and histiolymphocytic infiltration of the stroma are pronounced.
With glomerulonephritis, especially chronic, not only the kidneys are affected; a number of extrarenal changes appear. Because of arterial hypertension, hypertrophy of the heart, mainly the left ventricle, and changes in blood vessels develop - arteries (elastofibrosis, atherosclerosis) and arterioles (arteriolosclerosis) of the brain, heart, kidneys, retina, etc. In this regard, it should be emphasized that changes in the kidneys in chronic glomerulonephritis are associated not only with glomerulitis and its evolution into glomerulosclerosis, but also with nephrogenic arterial hypertension, arteriolosclerosis. With secondary shrinkage of the kidneys, the presence of arterial hypertension, cardiac hypertrophy and vascular sclerosis, the differential diagnosis of chronic glomerulonephritis and the renal form of hypertension is sometimes very difficult.
Etiology (causes)
In most cases of acute glomerulonephritis and only in 5-10% of cases of the chronic form of this disease, the cause can be identified. In other cases, the etiology remains in question.
Bacterial infections can cause the disease in question:
- staphylococcal
- streptococcal
- malaria
- tuberculosis
- syphilis, etc.
In recent years, the role of viruses in causing glomerulonephritis has been considered: HIV, herpes, hepatitis B and C. Toxic substances can also be the cause:
- alcohol
- organic solvents
- mercury compounds
- narcotic substances
- lithium compounds
- lead compounds
Among the reasons are also:
- exogenous Ag
- medicines
- endogenous Ag (DNA, tumor)
The triggering factor in the onset and exacerbation of the disease is cooling the body. Insolation may also be important.
Diagnostics and treatment at the clinic of Professor Gorbakov
Our clinic employs experienced doctors, it is possible to carry out any types of tests, and promptly carry out the necessary research. To avoid the development of the disease, consult a doctor at the first signs of illness in your child.
Glomerulonephritis is an inflammation of the kidneys, which is often a consequence of an infectious disease. Due to improper treatment and due to a weakened immune system, an infection from the sinuses, throat or any other part of the body through the blood can enter the kidneys and disrupt the urinary system, which is one of the most vulnerable in children.
Acute poststreptococcal glomerulonephritis
This is a diffuse immune complex inflammation of the renal glomeruli, which develops two or three weeks after antigenic exposure, and manifests itself as acute nephritic syndrome. A picture appears similar to that of proliferative intracapillary glomerulonephritis.
The disease is mainly diagnosed in young people. But in recent years, more and more cases have been recorded among elderly and old people. Men are most often affected - almost 2 times more often than women. Until now, contamination of the external environment with appropriate strains of streptococcus can provoke epidemics of acute post-streptococcal glomerulonephritis.
Causes and pathogenesis
Acute post-streptococcal glomerulonephritis is caused by nephritogenic strains of group A beta-hemolytic streptococcus. In the acute phase, immune complexes are formed on the glomerular basement membrane and/or in the mesangial tissue, which contain streptococcal Ag. The most important are endostreptosin and nephritogenic plasmin-binding protein.
After 2-3 weeks, an immune response develops, which is accompanied by activation of humoral inflammatory systems. Proinflammatory cells attracted to the site release active oxygen metabolites and damaging lysosomal enzymes, etc. Hemodynamic, hemocoagulation disorders, and cellular mechanisms are important. General and local hemodynamic disturbances during the acute nephritic stage are explained mainly by the vasoconstrictive effect of leukotrienes C4 and B4, thromboxane A2, and angiotensin II.
Pathomorphology
During the form of glomerulonephritis under consideration, the following phases are distinguished:
- exudative
- exudative-proliferative
- proliferative
- residual effects
The size of the glomeruli increases, and the vascular loops occupy the entire capsule cavity. The capillary loops are clogged with proliferating and swollen endothelial and mesangial cells and infiltrated with polymorphonuclear leukocytes. Electron microscopy shows deposits of electron-dense material on the epithelial side of the glomerular basement membrane, which are medically called humps. Changes in podocyte processes are also typical.
Symptoms and diagnosis
The development of the disease is acute, 2-3 weeks after streptococcal infection, which happens, for example, with scarlet fever. Acute nephritic syndrome develops, which includes sodium-volume-dependent arterial hypertension, edema and hematuria. In all cases, cylindruria, proteinuria, and in some cases, oliguria are recorded. Oliguria refers to a decrease in the amount of urine excreted by the kidneys.
The main symptom that occurs in all patients is hematuria. In 50% of cases, gross hematuria is observed: the urine looks like meat slop. Proteinuria is mainly of the subnephrotic level. In less than 30% of cases, nephrotic syndrome is likely to develop. In parallel with hematuria or a little later, signs of a decrease in the filtration capacity of the kidneys develop, up to acute renal failure. Oliguria or anuria (complete absence of urine) is observed, azotemia develops, and a decrease in GFR is noted.
Swelling first appears on the face, then becomes more pronounced, and its prevalence increases. They are caused by hypervolemia due to a pronounced decrease in the filtration function of the kidneys and sodium retention. Arterial hypertension is associated mainly with hypervolemia; in more than half of the cases it is characterized as moderate or severe.
With severe hypertension, the following complication may occur:
- swelling of the optic nerve with decreased vision,
- cerebral edema with manifestations of eclampsia,
- displacement of the left border of the heart laterally,
- HF with the development of tachycardia
Circulatory disorders in many cases develop in a small circle. There may be hydrothorax and hydropericardium. Acute post-streptococcal glomerulonephritis with typical development has a cyclical course, including three periods:
- acute nephritic
- reversal of symptoms
- clinical and laboratory remission
But in recent years, a latent or latent form of the disease has become more common, in which urinary syndrome (cylindruria, proteinuria <1 g/day, microhematuria) and moderate unstable arterial hypertension are manifested. In 20-30 cases out of 100 there may not be high blood pressure; in fact, in such cases there is no acute nephritic syndrome.
Often, the form of the disease in question ends with complete recovery after one and a half or two months. The course is considered protracted if certain symptoms do not go away for half a year or more. A long course suggests that the form of glomerulonephritis has become chronic; this happens in 5-10% of cases.
Such factors worsen the prognosis:
- development of nephrotic syndrome
- anuria or persistence of oliguria for more than 3 weeks
- a decrease over eight weeks or longer in the more general hemolytic activity of complement or its C3 fraction
- persistent arterial hypertension
- history of kidney disease or in family members
Laboratory research
The doctor prescribes a general blood test for the patient. ESR can be moderately increased, and during severe hypervolemia, hemoglobin concentration decreases, because the blood in the body is diluted. A biochemical blood test is important for diagnosis. For acute post-streptococcal glomerulonephritis, the following changes are typical:
- serum protein concentration is normal or slightly reduced due to hypervolemia
- increasing the concentration of nitrogenous wastes and electrolytes
- hypergammaglobulinemia (in some cases)
The development of nephrotic syndrome is accompanied by such changes as hypoproteinemia, hypoalbuminemia, dysproteinemia, hypercholesterolemia. GFR is often below normal. Monitoring glomerular filtration rate is important to select the correct dose of medication for treatment.
A method such as a coagulogram in severe cases of the disease and the addition of nephrotic syndrome reveals hyperfibrinogenemia. Immunological tests show a decrease in the overall hemolytic activity of complement and especially the concentration of the S3 fraction, an increase in the titers of antibodies to streptococcal Ag (antistreptohyaluronidase, antistreptokinase, antistreptolysin O).
A general urinalysis is another diagnostic method used, which in the disease in question reveals hematuria, proteinuria and cylindruria (can be either mild or severe). At the onset of the disease, aseptic leukocyturia may be severe. Urinalysis by Nechiporenko makes it possible to find out about the severity of hematuria, leukocyturia and cylindruria.
Daily proteinuria is a quantitative method that takes into account daily diuresis (urine output) and accurately assesses the dynamics of proteinuria (including during therapy). Proteinuria is non-selective. Zimnitsky's test shows that the relative density of urine in the initial stages of the disease remains preserved. Bacteriological examination of a throat smear or skin rash can detect streptococcus.
Instrumental studies
The electrocardiography (ECG) method is used. Detects or does not detect changes in the position of the electrical axis of the heart, signs of overload of the left parts of the heart, etc. Echocardiography may show dilation of the heart chambers, increased pulmonary artery pressure, and fluid in the pericardium.
A diagnostic method such as chest x-ray is used to identify signs of congestion in the pulmonary circulation and interstitial edema. An ultrasound shows that there are no changes in the kidneys, but only in some cases. Sometimes they can be increased in size, and there may be swelling of the parenchyma. Doppler mapping reveals signs of ischemia. Examination of the fundus can detect changes that occur due to hypervolemia and hypertension:
- hemorrhages
- papilledema
- phenomenon of pathological arteriovenous crossing
- constriction of arterioles
Differential diagnosis
Acute post-streptococcal glomerulonephritis during diagnosis must be distinguished from:
- pyelonephritis
- acute interstitial nephritis
- kidney damage due to systemic diseases
- exacerbation of chronic glomerulonephritis
For differential diagnosis, it is very important to correctly perform a kidney biopsy to determine the morphological substrate of the disease.
Treatment
For acute post-streptococcal glomerulonephritis, therapy includes several provisions. Not only drug therapy is important, but also a proper diet and rational regimen. The goals of therapy are:
- relief of acute nephritic syndrome
- elimination of streptococcal infection
- normalization of blood pressure
- maintaining water and electrolyte balance
- reduction of edema
- reduction in the activity of immune inflammation during prolonged course
- treatment of complications, if any (eg, acute renal failure or hyperkalemia)
Since this form of glomerulonephritis has a fairly high risk of complications, it is better to hospitalize the patient. On average, the period is from 6 to 8 weeks. The total duration of temporary disability in an uncomplicated course is 6-10 weeks.
General events
At the onset of the disease (especially if hypertension and edema are severe), the person needs to remain in bed for 14 days. Next, the doctor prescribes a gentle regimen for 12 months. You should not overcool during this period; it is better to limit physical activity. Vaccination cannot be carried out for 1 year after suffering from glomerulonephritis.
The diet involves, first of all, limiting fluid intake. In case of anuria and severe edema, it is better not to drink at all in the first 24 hours, then the volume of liquid drunk should correspond to the amount of urine excreted over the previous day + 200-400 ml. The amount of table salt in the diet is sharply limited: to 1-2 g/day. Also consume up to 0.5 g/kg of protein per day, no more.
Treatment of streptococcal infection
Etiotropic therapy is used if the development of acute glomerulonephritis occurred after tonsillitis, pharyngitis, streptopyoderma, especially if there are positive results of cultures from the throat, skin, or when high titers of antibodies to streptococcus are detected. Doctors often prescribe an antibiotic from the penicillin group:
- phenoxymethylpenicillin
- ampicillin
- amoxicillin + clavulanic acid
The antibiotic dose is calculated taking into account the GFR. Tonsillectomy is indicated no earlier than 6 months after the clinical signs of the disease disappear. With the development of acute glomerulonephritis as part of sepsis, long-term antibacterial therapy is indicated. The vast majority of patients with acute glomerulonephritis are not prescribed antibacterial therapy.
Treatment of acute nephritic syndrome
In acute glomerulonephritis, edema occurs due to primary fluid retention. Therefore, a special diet involves consuming a minimum of water and salt. An effective diuretic is furosemide, which is prescribed in a dose of 80-120 mg. If GFR decreases, hydrochlorothiazide may not provide the desired effect. Drugs such as spironolactone and triamterene are not prescribed due to the risk of developing hyperkalemia in the patient. Diuretics as a component of antihypertensive therapy reduce the need for other medications.
To eliminate moderate hypertension, often only the diet described above, bed rest and diuretics are enough. If hypertension is persistent and severe, the doctor may prescribe other drugs. These are mainly vasodilators, including slow calcium channel blockers (nifedipine 10 mg is effective). ACE inhibitors should be used with caution due to the risk of hyperkalemia.
Treatment of complications
With the development of hypertensive encephalopathy, furosemide in large doses is relevant for treatment. Convulsive syndrome is relieved by diazepam administered parenterally (unlike other anticonvulsants, it is metabolized in the liver and is not excreted by the kidneys).
, pulmonary edema may develop as a consequence of hypervolemia. In this case, cardiac glycosides cannot be prescribed. Treatment should be aimed at reducing venous flow to the heart and reducing pressure in the pulmonary vessels. The person should lie on the bed with the head elevated. Antifoam agents, oxygen inhalations are used, and in some cases artificial ventilation is used. Loop diuretics are effective: furosemide at a dose of 40-80 mg intravenously, then, if necessary, drip up to 200 mg. Narcotic analgesics and antipsychotics are also used for treatment: morphine is administered intravenously at a dose of 5 mg, fentanyl at a dose of 1-2 ml of a 0.005% solution is administered intramuscularly or intravenously, droperidol at a dose of 2-4 ml of a 0.25% solution is administered intramuscularly or intravenously. V. Vasodilators are effective. This may be a dosed administration of sodium nitroprusside [0.1 mcg/(kghmin)]. Hemodialysis sessions in ultrafiltration mode are prescribed if hypervolemia is significantly pronounced.
Acute renal failure requires limiting the intake of potassium, salt, water and protein. Hemodialysis is carried out if hyperkalemia and azotemia increase. Peritoneal dialysis is prescribed for sick children and elderly people. For severe hyperkalemia, therapy consists of using large doses of furosemide, insulin is administered intravenously, as well as calcium gluconate, glucose solutions, and sodium bicarbonate. If life-threatening hyperkalemia develops, hemodialysis is performed urgently.
Immunosuppressive therapy
Immunosuppressants are used for treatment if nephrotic syndrome persists or only develops, as well as in cases where kidney function has not been fully restored. Glucocorticoids are often effective: prednisolone at a dose of 1 mg/kg per day. If renal failure progresses rapidly (as indicated by a doubling of serum creatinine concentrations within 3 months or less), a kidney biopsy is performed.
If crescents are detected, a course of pulse therapy with methylprednisolone is recommended (500-1000 mg intravenously daily for 3-5 days). Cytostatics are prescribed only if there is no active infection. If possible, the use of GCs and cytostatics in acute glomerulonephritis should be avoided.
Spa treatment
This treatment should begin six months later or later after the elimination of clinical manifestations of glomerulonephritis. People are sent to local general sanatoriums, without sudden changes in climatic conditions. Treatment is not prescribed at resorts with a dry desert climate. Insolation is prohibited.
Complications and prognosis for cure
In severe cases, nephritis progresses rapidly, causing kidney failure, accompanied by severe swelling. Impaired kidney function leads to poisoning of the body with unresolved toxins. Problems arise with the functioning of other organs - the heart, liver, brain.
Undiagnosed and untreated glomerulonephritis becomes chronic and leads to renal failure. The kidneys shrink, decrease in size, and cannot fully perform their function.
If the disease is not treated, you can get:
- acute renal failure (in 1% of cases);
- acute heart failure (2-3%);
- intracerebral hemorrhage and visual impairment;
- preeclampsia, eclampsia (acute renal encephalopathy);
- chronic glomerulonephritis.
With timely contact with an experienced urologist, the symptoms of acute glomerulonephritis - edema and arterial hypertension - disappear within 2-3 weeks. For a complete recovery, you will have to undergo treatment for at least 2 months.
Clinical examination
After a person has suffered from acute glomerulonephritis, clinical observation is necessary for 2 years. The doctor is visited every 30 days for the first 6 months. We need to monitor the indicators of a general urinalysis, Nechiporenko urine analysis, general and biochemical blood tests. A person at home should systematically measure blood pressure and monitor its changes. In the next 1.5 years, examinations are carried out every 3 months. For two years, you need to limit salt and foods rich in purine bases in your diet. The amount of animal protein in the diet should be adequate to the age of the person who has recovered from the disease.
Not recommended:
- drink any alcoholic beverages
- smoking (cigarettes, hookah, etc.)
- use herbal medicines with nephrotoxic effects
- use medications and dietary supplements with nephrotoxic effects
- engage in heavy physical labor
- be exposed to sudden changes in temperature
- come into contact with toxic substances
Treatment
Typically, treatment of glomerulonephritis requires a hospital stay of 1-2 months. Treatment includes:
- Bed rest, diet and drinking regime,
- Antibiotics,
- Diuretic herbal preparations.
In difficult cases, plasmapheresis is prescribed; in extreme cases, if renal failure develops, a kidney transplant is prescribed.
After treatment for glomerulonephritis, children should be under the supervision of a pediatrician or nephrologist for several years, undergo regular urine tests, and not engage in active sports.
Other forms of acute glomerulonephritis
This disease can be caused not only by streptococci, but also by viral and bacterial diseases. In diseases caused by parasites, membranous glomerulonephritis is observed. With alcohol abuse, a mesangioproliferative form of the disease is observed. As for symptoms, this may be isolated urinary syndrome or severe forms of nephritis. Drug-induced or post-vaccination glomerulonephritis can be caused by minimal change disease and manifest as nephrotic syndrome.
Acute glomerulonephritis, caused by poisonous insect bites, allergens , is manifested by nephrotic syndrome and impaired renal function. Nephrotic syndrome, as a rule, develops after the manifestation of other allergic reactions (bronchial asthma, skin manifestations, etc.). But in rare cases, there may be no manifestations of allergies other than this. Treatment is the same as for acute post-streptococcal glomerulonephritis.
If nephrotic syndrome is severely expressed, glucocorticoids are relevant for treatment. In some cases, transition to chronic glomerulonephritis is possible, especially with repeated exposure to the causative factor.
↑ Etiology of primary glomerulonephritis
In some cases, the development of glomerulonephritis is associated with an infection, often bacterial (bacterial glomerulonephritis), in others there is no such connection (abacterial glomerulonephritis). Among the possible causative agents of glomerulonephritis, the main role is played by ß-hemolytic streptococcus (its nephritogenic types). Of lesser importance are staphylococcus, pneumococcus, viruses, and plasmopium malaria. In most cases, bacterial glomerulonephritis develops after an infectious disease, being an expression of the body's allergic reaction to the infectious agent. More often it is a sore throat, scarlet fever, acute respiratory disease, less often - pneumonia, erysipelas, diphtheria, meningococcal infection, prolonged septic endocarditis, malaria, syphilis. Glomerulonephritis can also be caused by non-infectious agents, in particular ethanol (alcoholic glomerulonephritis). Glomerulonephritis may be hereditary. Hereditary glomerulonephritis, or Alport syndrome, is characterized by:
- dominant type of inheritance;
- the most common occurrence and severe course of the disease is in boys;
- chronic latent course of nephritis of the hematuric type;
- predominantly productive nature of changes in the glomeruli (productive intra-extracapillary glomerulonephritis) resulting in glomerulosclerosis and chronic renal failure;
- combination of nephritis with deafness.
Symptoms
After the completion of the main phase of the infectious disease that caused the development of glomerulonephritis, namely on the 10-21st day, the following symptoms of glomerulonephritis in children may appear:
- Increased thirst
- Weakness,
- Darkening of urine
- Edema,
- Persistent hypertension and accompanying phenomena - headache, drowsiness, etc.
You should respond to the child’s symptoms of illness as soon as possible, consult a doctor and begin treatment to avoid possible complications of the disease - kidney failure and even cerebral edema.
If there is any suspicion of kidney pathology in children, a general urine test is prescribed, on the basis of which the pediatrician prescribes a consultation with a nephrologist and additional studies. These include blood tests, ultrasound of the kidneys, ultrasound examination of the renal vessels, fundus examinations, etc.
Typically, treatment of glomerulonephritis requires a hospital stay of 1-2 months. Treatment includes:
- Bed rest, diet and drinking regime,
- Antibiotics,
- Diuretic herbal preparations.
In difficult cases, plasmapheresis is prescribed; in extreme cases, if renal failure develops, a kidney transplant is prescribed.
After treatment for glomerulonephritis, children should be under the supervision of a pediatrician or nephrologist for several years, undergo regular urine tests, and not engage in active sports.