Chronic glomerulonephritis is a group of immune kidney diseases with primary damage to kidney structures such as the glomeruli, with subsequent involvement of other parts, a tendency to progress, resulting in renal sclerosis and the development of renal failure. The root cause of this group of diseases is not completely clear.
The pathological process in the kidneys, leading to damage to the glomeruli and occurring with the participation of the immune system, can occur through two mechanisms of an inflammatory and non-inflammatory nature.
The classification of glomerulonephritis is based on morphological characteristics (changes in kidney tissue during biopsy). Features of the course of glomerulonephritis largely depend on the morphological form.
Symptoms of glomerulonephritis
Symptoms characteristic of glomerulonephritis may vary depending on the course of the disease:
- pain in the lumbar region
- decreased urine output (oliguria)
- swelling
- high blood pressure
- shortness of breath combined with impaired urine output
- change in urine color (blood in urine - the color of meat slop)
- “foam cap” when urinating (an indirect sign of protein in the urine)
- anemia, the occurrence of which is associated with inhibition of the production of erythropoietic factor in the kidneys.
If such symptoms appear, it is urgently recommended to undergo examination to exclude glomerulonephritis.
For any severity of the disease, you must immediately consult a nephrologist for help, since any form of glomerulonephritis, especially in the presence of frequent complications and the absence of anti-relapse treatment, can lead to numerous complications, among which the main ones are the following:
- arterial hypertension of renal origin
- chronic renal and heart failure.
Gestational glomerulonephritis after childbirth
Gestational glomerulonephritis after childbirth
Glomerulonephritis during pregnancy is an acute or chronic immunoinflammatory disease with damage to the glomerular apparatus of the kidneys (glomeruli), as well as involving the tubules and interstitial tissue, which occurs before or during pregnancy.
More than half of the cases are asymptomatic. It may be manifested by a change in the color of urine to pink, reddish or brown, swelling of the face, limbs and body, increased blood pressure with dizziness, headaches, and weakness. Chronic glomerulonephritis is a group of morphologically heterogeneous renal pathologies, and can be both independent diseases and secondary to many systemic diseases, such as systemic lupus erythematosus, systemic vasculitis, hemorrhagic vasculitis, etc. The severity of the prognosis for this pathology is determined by the progression of the disease with the development of nephrosclerosis and terminal chronic renal failure. During pregnancy, both activation and manifestation of chronic glomerulonephritis can be observed. The most severe category is patients with chronic glomerulonephritis (primary or secondary) with a clinical and laboratory picture of nephrotic syndrome. The main symptom of damage to the glomeruli of the kidneys is proteinuria. Nephrotic syndrome is characterized by severe proteinuria (>3.5 g/day), hypoalbuminemia (serum albumin <25 g/l), hyperlipidemia and edema. Massive loss of protein in the urine leads to a decrease in the oncotic pressure of the blood plasma and the movement of the liquid part of the blood into the interstitial space. Edema develops, which varies in severity from pastiness of the face and feet to anasarca with the presence of fluid in the abdominal and pleural cavities. Edema is usually combined with oliguria and even anuria with weight gain. Nephrotic syndrome is always a reflection of severe kidney damage.
Patient K., 34 years old, was admitted to the nephrology department No. 1 of city clinical hospital No. 52 on July 4, 2019, with complaints of a sharp decrease in the amount of urine, severe swelling of the torso, legs, and arms.
From the anamnesis it is known: until 2021, she did not notice any health problems. In 2021, episodes of palpitations began to bother me; upon examination, an atrial septal defect, pulmonary hypertension (MPAP 32 mm Hg), and extrasystole were diagnosed. Metoprolol 12.5 mg was prescribed.
In December 2021, pregnancy occurred. In the 1st trimester, the course of pregnancy was complicated by the threat of miscarriage; she underwent inpatient treatment in a hospital in the Moscow region. The pregnancy was saved.
At the end of May 2021, the patient noted darkening of urine and decreased urine output. June 13, 2021 hospitalized in a Moscow city hospital.
Diagnosis on admission: Pregnancy 28 weeks, threat of premature birth. Gestational pyelonephritis.
Urine tests revealed for the first time severe proteinuria of the nephrotic level: an increase in protein content in the urine to 3.0 g/l (with the norm being up to 0.03). Antibacterial (with a diagnosis of gestational pyelonephritis), magnesium and antispasmodic therapy was carried out.
After discharge from the hospital, swelling of the torso, legs and arms began to increase, and she gained 14 kg in weight. Due to severe edematous syndrome, June 28, 2021. hospitalized by ambulance to the perinatal department of the Moscow city hospital.
Diagnosis on admission: Pregnancy 30 weeks. Head presentation. Moderate preeclampsia. Gestational pyelonephritis. Regional State Administration. Uterine fibroids. NMPC 1A art.
Upon admission, attention was drawn to pronounced nephrotic syndrome (total protein 48.7 g/l, albumin 23.2 g/l, proteinuria 3.4 g/l) with unchanged urinary sediment (leukocyturia 0-1 in the subcutaneous area, erythrocyturia 2-3 in p/z). Mild anemia was noted (hemoglobin 114 g/l). At the same time, blood pressure was normal, renal function was satisfactory (creatinine 62 µmol/l, urea 6.6 mmol/l), there was no liver damage (bilirubin 3.6 µmol/l, AST 20.4 units, ALT 18 units), platelet level within normal limits (platelets 277×109/l.).
The question of early (i.e., up to 36 weeks inclusive) delivery in patients with CGN most often arises in the case of unresolved gestational exacerbation or rapid progression of glomerulonephritis with a decrease in renal function - in each subsequent analysis, an increasingly higher level of protein in the urine is revealed.
A pregnancy of 29-30 weeks, moderately severe preeclampsia, and polyhydramnios was diagnosed. Due to the lack of effect from the therapy, taking into account severe proteinuria, oliguria, June 29, 2021. Emergency delivery was performed by cesarean section and myomectomy. A live premature boy was born, 1400 g, Apgar scores 5-6-7). Antibacterial and anticoagulant therapy and albumin transfusions were carried out. Severe nephrotic syndrome persisted, with proteinuria increasing to 18.6 g/l. Due to severe nephrotic syndrome, hyperhydration before anasarca, lack of positive dynamics after delivery, for further treatment July 4, 2021. the patient was hospitalized in the nephrology department No. 1 of City Clinical Hospital No. 52 and, due to the severity of her condition, was transferred to ICU No. 2 (resuscitation and intensive care unit for nephrological patients).
Diagnosis upon admission to the nephrology department No. 1 of City Clinical Hospital No. 52: Nephropathy in pregnant women. Nephrotic syndrome. Condition after delivery on June 12, 2019.
Upon admission to the ICU, proteinuria reached 44.31 g/day. Against the background of worsening nephrotic syndrome, there was a progressive critical decrease in total protein in the blood serum to 33.5 g/l, albumin to 17.5 g/l, and an increase in cholesterol to 11.8 mmol/l. This condition was complicated by the development of renal failure with oligoanuria and an increase in blood creatinine to 140 µmol/l.
When analyzing the clinical and laboratory picture, a differential diagnosis of the genesis of nephrotic syndrome was made. Obviously, this pathology could not be explained by preeclampsia. Firstly, the severity of nephrotic syndrome did not correlate with clinical and laboratory manifestations of preeclampsia (absence of arterial hypertension, normal platelet levels, LDH, absence of extrarenal manifestations). Secondly, after delivery, the pathological process did not regress (which would be expected with preeclampsia), but, on the contrary, continued to worsen.
The manifestation of chronic glomerulonephritis, nephrotic type, was diagnosed. Secondary chronic glomerulonephritis was excluded. Markers of systemic diseases were studied; antiphospholipid syndrome was not identified. To exclude primary membranous nephropathy, a blood test was taken for antibodies to phospholipase A2 receptors - the result was negative.
Thus, the most likely morphological variant of chronic glomerulonephritis in the patient was minimal change disease or focal segmental glomerulosclerosis. However, performing a kidney biopsy, necessary to clarify the morphological picture of nephritis, was not possible (taking into account coagulopathy in conditions of recent delivery, pronounced nephrotic syndrome, severity of the condition) due to the extreme risk of hemorrhagic complications.
The differential diagnosis of GN during pregnancy is very difficult due to the fact that preeclampsia can occur with a similar clinical and laboratory picture.
One of the most important differential diagnostic criteria for CGN is the timing of the onset of clinical symptoms—the threshold is considered to be 20 weeks of gestation. Thus, proteinuria, detected up to 20 weeks. pregnancy, indicates the presence of background or de novo kidney disease;
Also, the difficulties in diagnosing CGN during pregnancy are determined by the impossibility in most cases of carrying out morphological verification of the diagnosis. Kidney biopsy is rarely performed and, due to the high risks of complications, is limited to very strict indications.
Our patient was hospitalized in extremely serious condition with massive edema leading to anasarca, virtually no diuresis and progression of renal failure, which could require transfer to hemodialysis. In ICU No. 2, intensive therapy was carried out aimed at maintaining vital functions. Pathogenetic therapy was initiated, which included ultra-high doses of corticosteroids (pulse therapy with metipred followed by oral prednisolone, cyclosporine). This therapy is aggressive and carries risks of complications, but is absolutely necessary to save the patient’s life and restore normal function of the kidneys and other organs and systems. Taking into account the severity of the disease and the seriousness of the prognosis, every day, during 40 days of inpatient treatment, there was a struggle for the life of the young mother.
Thanks to timely, active treatment tactics, almost complete remission of severe nephrotic syndrome and restoration of kidney function were achieved. During treatment, renal function indicators completely normalized (creatinine 78 µmol/l), proteinuria decreased from 44 g/day to 1.1 g/day. The level of total protein gradually recovered - 50 g/l and albumin - 28 g/l. The young mother was able to return home to her baby. In the future, doctors from the consultative and diagnostic nephrology department of City Clinical Hospital No. 52 will monitor her health.
Diagnosis at discharge: Main: Chronic glomerulonephritis. Background: I premature surgical birth at 29-30 weeks, myomectomy dated June 29, 2019. Severe preeclampsia. Complications: Nephrotic syndrome. Status on pathogenetic therapy (corticosteroids, cyclosporine). Acute kidney injury is in the process of resolution. CKD stage 2 (GFR 86 ml/min by CKD-EPI). Anemia. Bilateral lower lobe pneumonia is in the process of resolution. Steroid acne. Chronic gestational pyelonephritis. Associated: Congenital heart defect: patent foramen ovale. Pulmonary hypertension. Superficial gastritis. Duodeno-gastric reflux. OU Retinal angiopathy.
Management of pregnancy in patients with kidney diseases requires careful monitoring of clinical and laboratory parameters and, if necessary, active and timely etiotropic or pathogenetic therapy. Kidney diseases are an aggravating background that predisposes to the development of severe pathologies directly associated with pregnancy, such as preeclampsia, eclampsia, and HELLP syndrome. The polymorphism of nephrological diseases dictates the need for careful monitoring of the course of pregnancy, differential diagnosis of various types of kidney damage and timely correction of therapy.
Participated in the management of the patient
Artyukhina Lyudmila Yurievna, head of the nephrology department No. 1 Ekaterina Sergeevna Ivanova, nephrologist of the nephrology department No. 1 Karina Eduardovna Loss, nephrologist of the ICU No. 2 Olga Lvovna Podkorytova, head of the ICU No. 2 Nadiya Fyaatovna Frolova, deputy chief physician for nephrological care Vasily Mikhailo Grabovsky hiv , Deputy Chief Physician for Obstetrics and Gynecology Care.
Diagnostics
The EXPERT Clinic has developed a clear algorithm for the primary diagnosis of glomerulonephritis. The necessary initial examination includes:
Laboratory methods
- general urine analysis
- clinical and biochemical blood tests are performed
- glomerular filtration rate is determined as a factor in assessing renal function
- immunological blood test.
Doctors at the EXPERT Clinic have compiled a list of necessary tests for a kidney screening examination.
Instrumental studies
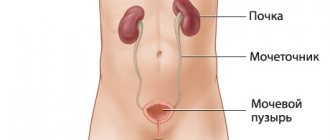
Ultrasound of the kidneys with Doppler examination of the vessels of the kidneys, which evaluates ultrasound signs of changes in the blood flow of the kidneys.
The final diagnosis is made ONLY with a kidney biopsy in a hospital setting.
Important! The scope of the necessary examination can only be determined by a nephrologist.
Treatment of glomerulonephritis
In the clinic, maintenance therapy and monitoring of the condition and function of the kidneys are carried out. The main treatment of glomerulonephritis and the selection of basic therapy is carried out in a specialized hospital. Complex treatment of glomerulonephritis includes drugs that affect the immune mechanisms of disease development: glucocorticoids, immunosuppressants, antiplatelet agents, which are prescribed in the hospital. In recent years, similar schemes have been prescribed for 6-24 months or more.
The general management of such therapy on an outpatient basis, determining its duration, drug doses, prevention and treatment of complications should be carried out by nephrologists. An important stage of treatment is the correction of blood pressure and the treatment of edema.
The EXPERT Clinic adheres to the principle of staged treatment.
At the first stage after inpatient treatment, an outpatient treatment plan is drawn up, which includes:
- mode
- diet
- supportive treatment.
At the second stage, the effectiveness of the therapy is assessed:
- If, while using maintenance treatment, destabilization of the condition develops, the nephrologist promptly refers the patient to inpatient treatment.
Even after achieving the long-awaited remission, the patient is advised to be attentive to himself and regularly see a nephrologist, as a relapse of the disease is possible.
Almost all patients need to take anti-relapse therapy recommended by their doctor. Some medications help reduce the risk of exacerbations and chronic renal failure.
Glomerulonephritis during pregnancy
A key feature of the treatment of glomerular nephritis detected in a pregnant woman is the restriction on the use of basic immunosuppressive drugs, including corticosteroids, due to the likely negative effect on the child and the course of pregnancy. Gestation management tactics include compliance with the requirements of the medical and protective regime, diet correction, and, if necessary, pharmacotherapy. A pregnant woman with glomerulonephritis is scheduled to be hospitalized in a specialized hospital twice: at 8-10 weeks - to assess the prospects of bearing a child and develop a gestational management plan, at 37-38 weeks - for planned prenatal preparation. Immediate hospitalization is indicated for progressive proteinuria and hematuria, hypertension, renal failure, and symptoms of fetal growth retardation.
In acute glomerulonephritis, strict bed rest is recommended; in clinically pronounced chronic glomerulonephritis, limited activity within the ward is recommended. Taking into account the severity of symptoms, it is necessary to reduce the amount of liquid and table salt consumed. For patients with acute forms of the disease, the amount of protein foods is limited; for patients with chronic forms, the amount is increased. For mild latent forms of glomerular inflammation, drug treatment is usually not used. Herbal medicine with compositions based on strawberries, bearberry, tricolor violet, yarrow, string, and black currant is possible. If clinical symptoms are present, the following groups of drugs are used:
- Diuretics
. For edema and decreased urination, fast-acting loop diuretics are preferred, blocking the reabsorption of sodium and chlorine ions, as well as xanthines, which improve renal hemodynamics. In parallel, potassium-containing drugs are prescribed to prevent hypokalemia. - Antihypertensive drugs
. The development of arterial hypertension is an indication for the use of medications that lower blood pressure. During pregnancy, cardioselective β1-blockers, calcium antagonists, and α2-adrenergic agonists are most often used. Vasodilators that also affect renal blood flow are effective. - Antiplatelet agents
. To improve blood supply to the organs of the mother and fetus, peripheral vasodilators, purine derivatives, and heparin are prescribed, which act at the microcirculatory level and prevent platelet adhesion. The use of indirect anticoagulants is limited due to the risk of developing hemorrhagic syndrome.
Antibiotics are used only when infectious agents are detected. Symptomatic therapy for glomerulonephritis is aimed at increasing hemoglobin levels (iron supplements, folic acid, red blood cell transfusion) and replenishing protein deficiency (infusion of plasma, albumin and protein solutions). Physiotherapeutic procedures are indicated, especially pulsed ultrasound on the kidney area, which stimulates vasodilation and has a desensitizing and anti-inflammatory effect.
Typically, women with glomerulonephritis are recommended to have a natural birth; a cesarean section is performed according to general indications when there is a threat to the mother or child. Early delivery is carried out in cases of unresolved gestational complications (severe gestosis, placental abruption, increasing chronic fetoplacental insufficiency, fetal malnutrition), therapeutically resistant arterial hypertension, and rapidly progressive decline in renal function.
Recommendations
Bacterial, viral infection, and the presence of foci of chronic infection can be considered as risk factors for the development of glomerulonephritis in patients with a genetic predisposition.
It is necessary to regularly monitor patients with systemic connective tissue diseases (systemic lupus erythematosus, scleroderma, rheumatoid arthritis, vasculitis, etc.), and women with kidney damage during pregnancy.
Basic preventive measures should be aimed at slowing the progression of glomerulonephritis. The diet should be monitored at every doctor's visit. The amount of salt, protein, and liquid varies depending on the clinical manifestations of the disease. Strong marinades, broths, and canned fish are prohibited.
Patients with glomerulonephritis are contraindicated in heavy physical activity, work at low temperatures, with increased dampness, and in the open air.
Patients who have suffered acute glomerulonephritis are observed for 2 years. For chronic glomerulonephritis, regular monitoring is recommended once a quarter.
FAQ
Can chronic glomerulonephritis be cured?
Chronic glomerulonephritis is a chronic kidney disease of an immune nature. A number of forms have a favorable course with long-term remission, some forms have an extremely aggressive course with the development of renal failure.
What causes the disease?
Glomerulonephritis is based on immune damage to the glomeruli of the kidneys with the involvement of other renal structures and the development of renal failure.
Is the disease a contraindication to pregnancy?
Carrying to term Frequent exacerbations, hypertension, and impaired renal function are indications for termination of pregnancy at any time.
Preservation of pregnancy is possible in some forms of glomerulonephritis with a favorable course in the phase of stable remission.
An absolute contraindication to pregnancy is an active process, frequent relapses, stable arterial hypertension, and decreased renal function.
Is there a cure for kidney failure?
Acute renal failure may resolve favorably. Chronic renal failure can only be corrected by replacement therapy (hemodialysis, peritoneal dialysis). Only a kidney transplant can solve this problem.
The problem, which can be conditionally designated as “chronic glomerulonephritis and pregnancy”, is only one aspect of the multidisciplinary problem “pregnancy in women with underlying kidney diseases” and includes many aspects - anatomical-physiological, pathophysiological, morphological and clinical, both nephrological, and obstetrics. The presence of underlying diseases of the kidneys and urinary system as a whole, in particular chronic glomerulonephritis (CGN), has for a long time been considered an unfavorable factor, if not a contraindication to pregnancy. The medical, psychological, social and ethical consequences of this approach are varied and mostly negative, especially since, according to modern epidemiological data, 3-10% of women of childbearing age have stage III-V chronic kidney disease (CKD)*. The main predictors of pregnancy outcomes in women with CKD are the level of proteinuria, the degree of renal dysfunction and the “controllability” of blood pressure (BP) before pregnancy. It is believed that these factors are more significant for prognosis than the underlying kidney disease itself. Moreover, it has now become known that pregnancy in women with CGN in half of the cases does not have a significant effect on the course of the disease, the complications that arise in 2/3 of the cases are reversible and 85% of pregnancies end in the birth of live children. In this case, specific significant factors, in addition to the above for CKD in general, are the need for immunosuppressive therapy, its volume and nature [1-4]. Thus, preconception counseling to resolve the issue of the possibility of carrying a pregnancy and the tactics of its management in women with CGN is of paramount importance and requires, in turn, a more in-depth acquaintance with the peculiarities of the mutual influence of kidney diseases (and CGN in particular) and pregnancy. It should also be emphasized that a multidisciplinary approach is required when managing pregnancy in women with CGN.
When examining pregnant women, symptoms such as edema, arterial hypotension or hypertension, proteinuria, changes in urinary sediment, etc. are often revealed. The presence of these symptoms requires a careful comprehensive analysis of anamnestic and clinical laboratory data, since none of them can be considered as a manifestation of any or one, and certainly a pathological process. Interpretation of the data obtained is complicated by the fact that often the examination performed in connection with pregnancy is actually the first or only one over a long period of time, and many symptoms can be characterized as physiological changes associated with pregnancy itself, or be a manifestation of underlying kidney disease (including and CGN), or indicate the development of specific gestational complications. Therefore, before talking about the features of pregnancy in women with CGN, it is necessary to consider some special aspects relating to physiological pregnancy, hypertensive gestational complications, and pregnancy with CKD.
Functional changes during physiological pregnancy
During physiological pregnancy, a number of changes occur in a woman’s body that relate to the regulation of general and intrarenal hemodynamics, the function of the renal tubules and water-salt metabolism [5, 6]. The scope of this publication does not allow us to discuss in detail the mechanisms underlying these changes, the main parameters of which are presented in Table. 1.
Table 1. Dynamics of some indicators during physiological pregnancy Note. SBP—systolic blood pressure; DBP—diastolic blood pressure; HR—heart rate; GFR is glomerular filtration rate.
It should be noted that during physiological pregnancy, blood pressure levels decrease already in the first trimester of pregnancy, by an average of 5-15 mm Hg; due to such physiological hypotension, initial arterial hypertension (AH) can be masked. Therefore, blood pressure indicators, which are normal for the general population, when recorded in pregnant women in the first and second trimesters, indicate the presence of A.G. Only from the third trimester is there a gradual increase in peripheral vascular resistance, and the blood pressure level returns to the background level or exceeds it by 10-15 mm Hg.
At the same time, the total plasma volume and cardiac output increase by 30-40%, and already at the 6th week of pregnancy, renal plasma flow and glomerular filtration rate increase. Normal values of GFR in pregnant women already in the very early stages are 120-150 ml/min, therefore the normal level of serum creatinine (CR) is lower than before pregnancy (65 µmol/l in the first trimester, 51 µmol/l in the second trimester, 47 µmol/l in the third trimester). Indicators considered normal for non-pregnant women (80 µmol/l) may indicate renal dysfunction during pregnancy, which requires a more thorough examination.
Against the background of an increase in GFR, multidirectional changes in the function of the renal tubules occur; as a result, slight glucosuria, proteinuria (not exceeding 0.3 g/day), aminoaciduria and bicarbonaturia may develop with the appearance of a persistent alkaline urine reaction.
Already from the first days of pregnancy, sodium and water retention occurs - the total water content in the body during pregnancy increases by an average of 8 liters, of which 1/3 is distributed in the mother's body. Excess sodium and water accumulates mainly in the extracellular space, which leads to the formation of so-called physiological edema, but some of the water remains in the vascular bed. Accordingly, hypervolemia develops, and parameters such as circulating plasma volume, minute volume of blood circulation, uterine blood flow, renal blood flow and glomerular filtration, which were already mentioned above, increase. At the same time, the sodium content in the blood serum decreases (to 132-140 mmol/l) and plasma osmolality (by an average of 10 mOsm/kg). It must be borne in mind that limiting the use of table salt and prescribing diuretics lead to a decrease in physiological hypervolemia, therefore, during physiological pregnancy, a free salt regime is recommended; diuretics are not indicated.
Gestational complications
In addition to physiological changes, pregnancy can also provoke pathological conditions, including damage not only to the kidneys, but also to other organs. Due to the similarity of symptoms of the so-called hypertensive gestational complications (which include hypertension in pregnant women, preeclampsia and eclampsia) and CGN, there is often a need to make a differential diagnosis between these conditions [7-14]. Clinical characteristics of hypertensive complications of pregnancy are given in Table. 2.
Table 2. Hypertensive complications of pregnancy
Discussion of the etiology and pathogenesis of hypertensive complications of pregnancy is not included in the scope of this publication, however, it should be noted that one of the most important differential diagnostic criteria is the timing of the onset of clinical symptoms - the threshold is considered to be 20 weeks of gestation. Thus, proteinuria detected before 20 weeks of pregnancy indicates the presence of background or de novo
kidney diseases; Hypertension registered before 20 weeks of pregnancy is also not a pregnancy complication and is considered “chronic hypertension.” It is important to keep in mind that CKD itself is a risk factor for the development of hypertensive gestational complications, and when conducting differential diagnosis, it is necessary to take into account the possibility of gestational complications layering on the underlying disease.
Pregnancy in women with kidney disease
Chronic kidney disease (CKD) is a supra-nosological concept introduced into clinical practice to improve the quality of diagnosis, treatment and outcomes of kidney diseases. There are 5 stages of CKD, and it should be especially emphasized that establishing the presence of CKD of one stage or another in no case replaces the main diagnosis. Identification of CKD in a patient creates alertness regarding the development of chronic renal failure, and establishing the stage of CKD allows the application of a general examination algorithm and therapeutic strategy developed for this stage, while the main diagnosis determines the possibilities of specific therapy and, in part, the rate of progression of the disease [15].
Pregnancy may have an adverse effect on the course and outcome of CKD and vice versa. It is known that as GFR decreases, the ability to conceive decreases, and the risk of complications for both the mother and the fetus increases [4, 10, 16-18].
Risk of complications for the mother:
1) decreased GFR, possible need for dialysis during pregnancy or in the short term after childbirth;
2) severe hypertension;
3) layering of preeclampsia - complications associated with damage to the kidneys, liver, central nervous system, thrombocytopenia, bleeding;
4) nephrotic syndrome - risk of thrombosis and sepsis.
Risk of complications for the fetus:
1) fetal growth retardation or intrauterine fetal death due to placental insufficiency;
2) premature birth;
3) side effects of drug therapy;
4) hereditary kidney diseases.
In general, when determining the management of pregnancy in women with CKD, a general approach should be followed: the ability to conceive and successfully carry a pregnancy, as noted above, depends mainly on the level of blood pressure and the state of renal function, and not on the nature of the underlying disease. Only in certain nosological forms, such as systemic scleroderma, periarteritis nodosa, other systemic vasculitis and systemic lupus erythematosus with a high degree of activity, and some variants of idiopathic CGN in the acute stage, does the nature of the kidney disease itself play a determining role. In such situations, the pregnancy prognosis is considered a priori unfavorable; in other cases, three categories of patients are distinguished: with preserved or slightly impaired renal function (Cr blood ≤130 µmol/l), with moderate renal failure (Cr - 130-220 µmol/l), and with severe renal failure (Cr ≥220 µmol/l) (Table 3).
Table 3. Maternal and fetal renal outcomes by baseline renal function
As can be seen from the table below. 3, an important prognostic factor in women with CKD is also the level of blood pressure. In the absence of hypertension, the natural course of most known diseases of the renal parenchyma does not change significantly under the influence of pregnancy. In women with well-controlled blood pressure and mild renal dysfunction, pregnancy is not contraindicated, but such patients require careful monitoring and should be advised that termination of pregnancy may be necessary if renal function deteriorates or uncontrolled hypertension develops. Women with hypertension and/or moderate to severe renal impairment should be advised to avoid pregnancy, as in 40% of cases pregnancy either develops/worsens hypertension or causes a sudden and often irreversible deterioration in renal function.
The principles of antenatal management of patients with chronic kidney disease [4, 16, 19] are as follows:
- correction of hypertension with target values 110-140/80-90 mm Hg;
- prescribing aspirin (75-150 mg/day) for creatinine >130 µmol/l;
— assessment of the dynamics of serum creatinine;
- monitoring and assessment of proteinuria, including nephrotic syndrome - prescribing heparin for nephrotic syndrome;
— assessment and maintenance of water balance;
— review of nephroprotective and antihypertensive therapy taking into account pregnancy;
— identification of “layering” of preeclampsia;
— assessment of the fetus’s condition — indications for delivery;
— taking into account the nature of the underlying disease and the specific problems associated with it.
Pregnancy in women with chronic glomerulonephritis
Chronic glomerulonephritis is a large group of pathogenetically heterogeneous diseases, the classification of which is based on morphological characteristics. Currently, the following morphological variants of CGN are distinguished: minimal change disease (MCD), focal segmental glomerulosclerosis (FSGS), membranous nephropathy (MN), IgA nephropathy (IgA-N), membranoproliferative glomerulonephritis (MPGN), extracapillary glomerulonephritis (ECGN) and diffuse nephrosclerosis (DS). Features of pathogenesis make it possible to distinguish between “idiopathic” glomerulonephritis and various glomerular lesions in a number of extrarenal diseases. It is now generally accepted that MCD, FSGS, MN and IgA-H can be observed both in the form of “idiopathic” and “secondary” forms, MPGN and ECGN in most cases are considered as kidney lesions in systemic, infectious, oncological and genetically determined diseases, and DS, as well as a number of cases of FSGS, is the outcome of many different diseases of the renal parenchyma [20, 21]. There are also familial glomerular diseases (Alport syndrome, thin basement membrane disease, Fabry disease, nail-patella syndrome, etc.). A detailed discussion of all of these conditions within the scope of this publication is impossible, so we will limit ourselves to the characteristics of the course of pregnancy in women with idiopathic CGN.
Clinically, CGN can manifest itself in the form of nephrotic syndrome (NS), isolated urinary syndrome (IUS), acute nephrotic syndrome (ONS) and rapidly progressive glomerulonephritis (RPGN). Characteristics of the syndromes and clinical and morphological correlations are presented in Table. 4. Chronic renal failure, i.e. CKD stages IV-V, can develop as a result of any variant of CGN.
Table 4. Clinical manifestations of CGN and main morphological correlations
It is believed that if CGN is manifested before pregnancy only by proteinuria and/or changes in urinary sediment, pregnancy proceeds normally, and special treatment for patients with UTI is not required. When assessing the dynamics of clinical and laboratory parameters in women with CGN occurring with IMS, it should be remembered that since, as already noted, protein excretion in the urine during pregnancy is physiologically increased, proteinuria can significantly increase, reaching the nephrotic level in 1/3 of cases. This in itself does not necessarily indicate a worsening of the underlying disease.
The presence of ONS and RPGN always indicates rapid progression of the disease and, accordingly, as stated above, serves as a contraindication to pregnancy. If these syndromes occur during pregnancy (exacerbation of the underlying disease or de novo
), then, taking into account that with a high degree of probability we are talking about systemic, infectious or other diseases that pose a serious threat to the health and life of a woman, termination of pregnancy, screening for systemic diseases, a kidney biopsy, and in some cases massive immunosuppressive therapy. In cases where a sudden and unexplained deterioration in renal function is detected long before the end of pregnancy, immediate renal biopsy is advisable, since if RPGN is diagnosed early, therapy with corticosteroids (CS) and plasma exchanges may be effective (options for immunosuppressive therapy in pregnant women will be discussed below).
Thus, the main clinical manifestation in idiopathic CGN, which requires further assessment and discussion, is NS, the presence of which, regardless of the characteristics of the underlying disease, significantly worsens the prognosis for both the mother and the fetus: the risk of perinatal fetal death increases significantly (up to 23 %), delayed fetal development, premature birth (up to 35%), addition or development of hypertension and deterioration of renal function in the mother [1, 2, 4].
In cases where pregnancy is planned or occurs in women with a previously established diagnosis, the morphological variant of CGN is of certain importance. Thus, with FSGS and IgA-H, pregnancy can more often provoke the development of exacerbations and be accompanied by a large number of complications, and with FSGS the probability of irreversible deterioration in renal function and the development of hypertension is especially high [4].
Significant difficulties in the development of NS during pregnancy are presented by the differential diagnosis of preeclampsia, the occurrence of de novo
and exacerbation of CGN, especially in women who have not previously sought medical help. As has already been shown in the section “Gestational complications,” if NS develops before 20 weeks of pregnancy, the diagnosis of preeclampsia can be excluded. In cases where NS occurs after 20 weeks of gestation, it is necessary to carefully clarify the anamnesis data relating to both the period before pregnancy and during pregnancy. The dynamics of clinical and laboratory manifestations are of some importance: the development of preeclampsia in pregnant women with CGN is characterized by a rapid increase in proteinuria to a high level with the addition of high A.G. On the contrary, with an exacerbation of CGN, proteinuria often increases more gradually and then stabilizes. But in some cases, adequate diagnosis and determination of management tactics are impossible without performing a kidney biopsy.
It has long been accepted that pregnancy is a relative contraindication to this procedure, as there have been reports of bleeding and other biopsy complications in pregnant women. However, these reports date from a time when biopsies were performed in hypertensive patients and there was little understanding of the mechanisms of coagulation abnormalities in women with preeclampsia. It has now been shown that if biopsy is performed in women with well-controlled blood pressure and normal coagulation parameters, the risk of complications does not exceed that in the general population of nephrology patients. However, percutaneous puncture biopsy of the kidney during pregnancy is rarely performed, since in general the morphological variant of glomerular damage is less important for the outcome of pregnancy than clinical manifestations [22].
With the development of NS before 20 weeks of gestation, a kidney biopsy makes it possible to make an accurate diagnosis and determine management tactics. Some authors recommend in such cases to carry out a course of treatment with CS without conducting a morphological study, however, it is more justified to establish the morphological substrate of the NS and, accordingly, the likelihood of an effect from the use of CS. This approach is safer - pregnancy itself is associated with hypercoagulation, which can increase with the use of CS, so their prescription should be supported by data from a morphological study of renal tissue.
At a gestational age of more than 32 weeks, a kidney biopsy is contraindicated, since in such periods, with the development of UA and/or a progressive decline in renal function, the decision on delivery should be made as quickly as possible and based on clinical data.
In general, tactics for the occurrence of NS, depending on the timing of gestation, are determined as follows:
— I trimester — termination of pregnancy, kidney biopsy;
— III trimester (term >32 weeks) — early delivery, kidney biopsy;
- II-III trimester (<32 weeks) - kidney biopsy, decision based on clinical and morphological data.
Management of pregnant women with NS involves, first of all, replenishing protein losses due to increased protein content in food. Protein restriction in the diet is not indicated even in the presence of stage IV CKD. Salt restriction is not required; the use of diuretics should be excluded, since these patients have initial hypovolemia due to NA, and a further decrease in intravascular volume will lead to a deterioration in uteroplacental perfusion. In addition, diuretics can provoke the development of hypotension, collapsed states and thromboembolic complications. Only in patients with a combination of NA and hypertension can moderate restriction of dietary salt intake and careful use of diuretics be recommended for the prevention of uncontrolled hypertension, requiring premature termination of pregnancy [1, 2, 4].
The question of the use of immunosuppressive therapy for idiopathic CGN during pregnancy remains the subject of study. Cases of the use of CS in pregnant patients with FSGS that occurred with N.S. are described. The effectiveness of therapy did not differ from that in the treatment of exacerbations not associated with pregnancy; side effects were not recorded in either women or newborns. Since endothelial-platelet hyperactivity plays an important role in the development of pregnancy complications in patients with CGN, the use of aspirin and heparin is recommended for the prevention of thrombotic and hypertensive gestational complications [16, 19]. The possibility of using some drugs is presented in table. 5.
Table 5. Possibility of using certain medications in patients with CGN during pregnancy
Early delivery is indicated in cases of uncorrectable gestational exacerbation of CGN or rapid progression of nephritis with a decrease in renal function (which is quite rare) and an increase in the severity of hypertension (develops in 10-20% of cases). Moreover, any manifestation of CGN, proteinuria, hematuria, renal failure or hypertension, is not yet a reason for termination of pregnancy. The dynamics of these indicators are important; only an increase in changes that cannot be corrected can serve as a reason for early delivery of pregnant women with CGN. Moreover, if in the first trimester in such cases termination of pregnancy is justified, followed by active pathogenetic therapy, then in the second and third trimesters it is quite difficult to make the right decision; an attempt to maintain pregnancy and conduct symptomatic, and in some cases, immunosuppressive treatment is justified. After the 34th week of pregnancy, early delivery is recommended.
Pregnancy in women with CGN receiving renal replacement therapy
The first successfully completed pregnancy in a patient using dialysis dates back to 1970. Until now, pregnancy in women receiving dialysis treatment is considered a rare and generally undesirable event. The outcome of pregnancy with the birth of live children, according to the largest registers, is 61.4-86.4% of cases, births are often premature, and polyhydramnios is noted. For a favorable pregnancy outcome, the “dose of dialysis” is crucial, maintaining a urea level of <15 mmol/l. Live births, depending on the “dialysis dose,” range from 48% at a dose <20 hours/week to 85% at a dose >36 hours/week (daily nocturnal hemodialysis) [17, 23–25].
A differentiated approach is recommended for female kidney transplant recipients [4, 26]. The world literature describes several thousand pregnancies in women with a kidney transplant, more than 90% of them ended successfully. The described complications, both in the mother and the fetus, were associated primarily with immunosuppression. Pregnancy is not contraindicated in kidney transplant patients who meet the following criteria:
- stable graft function for one to 2 years,
- absence of proteinuria or minimal proteinuria,
- absence of hypertension or controlled hypertension,
— no disturbances in the urodynamics of the graft,
— Kr <130 µmol/l,
- low doses of immunosuppressants: prednisolone ≤15 mg/day, azathioprine ≤2 mg/kg/day, cyclosporine <5 mg/kg/day.
Thus, the presented material allows us to draw the following conclusion.
— The mere presence of CGN is not a contraindication to pregnancy.
— Pregnancy is possible in the absence of signs of GN activity, in the absence or with satisfactory correction of arterial hypertension and preserved renal function.
— Patients planning pregnancy require preconception counseling and timely correction of ongoing antihypertensive, immunosuppressive and pathogenetic therapy.
— Both maintenance therapy and treatment of exacerbations and blood pressure control should be carried out with safe drugs.
— A multidisciplinary approach is necessary: throughout pregnancy and the postpartum period, patients should be observed not only by an obstetrician-gynecologist, but also by a nephrologist with regular monitoring of proteinuria, blood pressure, and blood creatinine.
— The main predictors of adverse outcomes for both mother and fetus are the activity of the underlying disease, arterial hypertension and impaired renal function.
— When an exacerbation with nephrotic syndrome develops, a differentiated approach is necessary (kidney biopsy, immunosuppressive therapy).
— Prevention of preeclampsia and thrombosis should be carried out by prescribing aspirin from the moment of pregnancy, and in the presence of aggravating factors - in combination with heparin.
— Indications for termination of pregnancy in chronic glomerulonephritis are uncorrectable exacerbation or rapid progression of the disease, as well as worsening arterial hypertension.
For characteristics of CKD and staging principles, see the section “Pregnancy in women with kidney disease” (Author’s note).