Characteristics of Pseudomonas aeruginosa
This motile gram-negative bacterium is rod-shaped with rounded ends, measuring 2 x 0.5 µm on average. It is equipped with flagella for movement in space.
It is an obligate aerobe, i.e. can only exist in the presence of oxygen.
Pseudomonas aeruginosa lives in water, soil, air, on plants, objects, and is found in small quantities in the gastrointestinal tract and upper respiratory tract of humans.
It is capable of producing toxins and substances that affect body tissues, liver cells, leukocytes, pulmonary surfactant, and also secretes a number of pigments, one of which has a blue-green color, which determines the name of the microorganism.
Successfully competes with other microbes. It is highly resistant to antibiotics, antiseptics, and environmental factors.
These bacteria have an interesting feature - they form colonies that are covered with a special protective film. They are credited with “social behavior.” The collective intelligence of such communities is aimed at combating unfavorable conditions.
Routes of infection:
- airborne;
- food;
- contact.
The entry points for infection can be damaged mucous membranes and skin, the gastrointestinal tract, the conjunctiva of the eye, the umbilical wound in newborns, etc.
Determination method using Bond and Blesk media.
When using the second method, 1 liter of water is taken as a sample and poured into two 500 ml containers. Next, 50 ml of Bonde medium is added to them, after which the resulting mixture is mixed and incubated for 24-48 hours at a temperature of 37 C. The first inspection of the crops is carried out a day later. If microbial growth occurs, Bonde's medium becomes cloudy. To confirm that these bacteria actually belong to the desired category, they are inoculated on Blesk medium.
If Pseudomonas aeruginosa is detected, then dark red colonies grow on the medium, which have a golden sheen or specks on the plaques. If there is no growth of bacteria, or detection of colonies of another type, sowing is repeated after 48 hours.
Why is Pseudomonas aeruginosa dangerous?
A special property of this bacterium, like any conditionally pathogenic organism, is the ability to become more active and manifest its negative qualities when the immune system is weakened.
The infection will appear in the following cases:
- with reduced body defenses (old age, children in the first months of life, HIV, leukemia and other cancers, diabetes mellitus, chronic bronchitis, cystic fibrosis, the need for constant hemodialysis, extensive burns, taking hormones);
- entry of the pathogen into internal environments (long-term mechanical ventilation, catheterization of cavities, etc.);
- high microbial load.
The latter often occurs in intensive care, burn and surgical departments with a purulent profile. Favorite places for the stick: catheters, endotracheal tubes, ventilators, washbasins, air conditioners, taps. Therefore, a long stay of an already weakened body in these places is a huge risk of developing complications caused by the bacterium.
When the rod is activated, diseases of the urinary system occur (in 35% of patients), pneumonia (5-10%), purulent wound processes, enteritis, encephalitis, osteomyelitis. In severe cases, sepsis develops, even leading to death.
Routes of infection
If Pseudomonas aeruginosa is found in a child’s urine, you need to understand how it got there. Often it appears in the body, especially in children, in stationary conditions. When the patient is weakened, many bacteria stick to him. It is during treatment for other diseases that the immune system is not able to fight Pseudomonas. It’s easier for adults to cope with it, but it’s especially difficult for children.
She lives in hospitals everywhere. In respirators, food, toilets, sinks and even disinfectants. People become infected from each other and from medical staff, as well as from contact with hospital tanks. In 20% of infections, this bacterium is to blame.
How to deal with Pseudomonas aeruginosa
Fighting this microorganism is not an easy task. This is facilitated by:
- its great resistance to various antiseptics;
- insensitivity to many antibacterial drugs;
- protective properties and “social behavior” of colonies of the infectious agent;
- weak immune response of patients at risk.
Successful resistance to bacteria is helped by:
- reducing the length of stay of patients in high-risk departments (intensive care, burns, etc.);
- increasing patient immunity;
- compliance with strict sanitary requirements in hospitals and the fight against nosocomial infections;
- the use of physical methods of disinfection of instruments and medical devices (boiling, autoclaving);
- use of 3% hydrogen peroxide, 5-10% chloramine solution and modern disinfectants (Septolite line) for surface treatment.
Clinical picture
If Pseudomonas aeruginosa is found in the urine, then it is often a urological infection. This could be cystitis, urethritis, pyelonephritis. During various manipulations associated with the installation of a catheter, during operations, this bacterium can enter the body and begin to multiply there. The disease can occur in acute and chronic form. The latter type is characterized by an asymptomatic picture. In this case, the bacteria can only be detected by taking a culture test.
Below we suggest familiarizing yourself with some signs indicating the presence of Pseudomonas aeruginosa in the body:
- foamy urine;
- frequent urination with strong urge;
- unpleasant-smelling urine discharge;
- pain during urine output;
- the presence of blood, which causes urine to become an unusual color;
- temperature increase;
- pain in the lower back.
Diagnostics
Until Pseudomonas aeruginosa is detected in the genitourinary system, the doctor does not prescribe treatment, even if the above symptoms are present. To begin with, a general urine test is recommended. If the results indicate inflammation (white blood cells are higher than normal), then the doctor will definitely suggest additional testing aimed at detecting the bacteria
The patient needs to collect morning urine. The laboratory assistant will sow it into a nutrient medium that already contains antibacterial drugs that prevent other microorganisms from developing. Thanks to this, it will be possible to discover the properties that are inherent in Pseudomonas.
When the results indicate the number 10 to the fifth power of CFU/ml, then there are all indications for therapy. To determine the sensitivity of bacteria to drugs, the disc method is used. For this purpose, special discs are placed on top of the sowing surface, which are impregnated with an antibiotic.
Treatment
Test-confirmed Pseudomonas aeruginosa in the genitourinary system requires mandatory treatment. The duration of therapy depends on the individual case. It is installed by a doctor. Treatment usually takes place in a hospital. The most important drugs are antibiotics. When the resistance of the stick to certain agents is established, then treatment only begins.
Often, local therapy using a catheter is also prescribed in parallel to kill bacteria in the urinary tract. Immunotherapy will also not be superfluous, since it is very important to help the body cope with the enemy, using all available methods.
Medication
Pseudomonas aeruginosa in the urine is treated with the following drugs:
- Antibacterial agents (Dioxidin);
- Antibiotics of the polypeptide group (Gentamicin, Ziomycin, Colistin and others);
- Antibiotics of the penicillin group, as well as cephalosporins (Ticarcillin, Cefoperazone, Carbenicillin and others).
Traditional methods
Traditional medicine always acts as a complement. And always after the doctor’s permission, especially if Pseudomonas aeruginosa is found in the child’s urine.
Aspen leaves. A decoction is prepared from this raw material. You need to take two tablespoons of dry leaves and add water to them. Cook for about twenty minutes over low heat. Leave for an hour, wrapped in a warm wool cloth. The strained broth is taken two tablespoons on an empty stomach.
Viburnum berries. You need to take one tablespoon of berries, pour boiling water over them and cook in a water bath for about twenty minutes. Squeeze the berries and strain the broth. Then add two glasses of water (boiled). Drink half a glass four times a day.
Prevention
Medical staff are required to undergo regular examinations so that the wand is identified on time. Equipment must be thoroughly treated with antiseptics and special solutions that kill all pathogenic flora.
Patients who are seriously ill should be kept in separate rooms.
Primary prevention includes strengthening the immune system. If the patient eats healthy food, washes his hands thoroughly and observes basic rules of personal hygiene, then Pseudomonas aeruginosa is unlikely to be detected in his urine. Share:
On the use of immunotherapy in the treatment of malignant otitis externa (clinical case)
Malignant otitis externa (MOE) is an inflammation of the external auditory canal involving adjacent tissues, damage to the bones in the ear canal and at the base of the skull. However, the name is not related to the fact that this disease is a tumor, but only emphasizes its severity, so another name can be found in the literature - necrotizing external otitis [1]. Malignant neoplasm with concomitant osteitis of the temporal bone and mandible was first described in 1959 [2]. Among the predisposing factors of the disease, many authors note two trigger points: the presence of a violation of the integrity of the skin of the external auditory canal in patients at risk. Skin damage can occur when cleaning the ear with metal objects, irritation of the external auditory canal with earmolds of hearing aids, headphones, or constant water getting into the ear (“swimmer’s ear”). Risk groups include elderly patients, those with immunodeficiency, a history of diabetes mellitus, cancer, after long-term radiation or chemotherapy, and hypovitaminosis [1, 3–7].
Many authors are of the opinion that the etiological factor of this disease is an opportunistic gram-negative bacterium - Pseudomonas aeruginosa (Pseudomonas aeruginosa) [8, 9]. This is a rod-shaped bacterium with rounded ends, 0.5 to 1 micron in size, mobile, does not have a dense capsule, does not form spores, is an obligate aerobe - it reproduces with access to oxygen and high humidity. During bacteriological examination, it grows on special nutrient media (meat-peptone agar - MPA, meat-peptone broth - MPB and others), where, as it grows, bluish-greenish colonies with a glow (fluorescent) appear, smelling of jasmine. The presence of surface villi in most of its strains ensures adhesion to cells; the pathogenic effect is due to the formation of exotoxins (exotoxin A, cytotoxin, etc.) and the release of endotoxins during cell cytolysis [8]. Infections caused by Pseudomonas aeruginosa are difficult to respond to antibacterial therapy due to its multiple resistance transmitted by R-plasmids, as well as due to the ability to form a mucus-like capsule - a glycocalyx - around its colonies. Pseudomonas aeruginosa is resistant to the action of many aminoglycosides, cephalosporins and fluoroquinolones, which complicates the effectiveness of therapeutic measures in patients [9–13].
Infection and the occurrence of infection occurs in three stages: 1) attachment of Pseudomonas aeruginosa to the damaged tissue and its reproduction at the site of attachment (primary focus of infection); 2) spread of infection into deep tissues - the so-called local infection; 3) penetration of the pathogen into the blood with the development of bacteremia and spread of infection to other organs and tissues (septicemia).
Malignant external otitis is a serious disease that begins with damage to the skin of the external auditory canal and the formation of granulations, most often at the border of the cartilaginous and bone sections. The cause of necrotic phenomena is necrotizing vasculitis involving the entire vessel wall. Then the process spreads to the cartilage, temporal bone and base of the skull, nearby soft tissues, and the parotid gland. Patients are concerned about constant pain in the ear, suppuration from it, the presence of soft tissue infiltrates in the parotid areas, enlargement of regional lymph nodes, and when the temporomandibular joint is involved in the process, trismus of the masticatory muscles. Complications such as mastoiditis, petrositis, osteomyelitis of the temporal bone, paralysis of the facial nerve, and lesions of the IX–XI cranial nerves are common. Mortality in the absence of damage to the cranial nerves does not exceed 10%, in case of facial nerve palsy it reaches 50%, and in case of multiple cranial nerve palsies it exceeds 80% [1]. Sometimes death occurs from sepsis.
In 1987, Peter Friedman and David Cohen described the diagnostic criteria for cancer, which were divided into two categories: mandatory and additional [14]. Mandatory symptoms include pain, swelling, exudation, granulation, the presence of changes in bone structures, isolation of Pseudomonas aeruginosa in bacterial cultures and lack of effect from local treatment within a week. Additional criteria are the presence of diabetes mellitus, old age, involvement of cranial nerves in the process. To make a diagnosis, the patient must have all the mandatory signs; the presence of only one or two mandatory criteria along with additional ones is not a basis for confirming cancer.
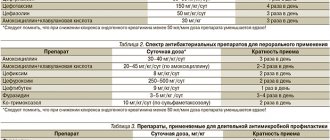
Issues of treatment of cancer remain relevant due to the long relapsing course of this disease and unfavorable prognosis [1–5]. The recommendations require the prescription of antibiotics with an antipseudomonal spectrum - aminoglycosides, fluoroquinolones, ceftazidime, cefepime, imipinem/cilastatin in large dosages [1–5]. The duration of antibiotic therapy is individual, it is necessary to take into account clinical data (regression of symptoms, decrease in ESR in a clinical blood test). If conservative treatment is ineffective, they resort to extensive surgical intervention - all necrotic tissue is removed, including cartilage, bone, and the parotid gland.
Ongoing clinical studies are aimed at identifying the most effective treatments for Pseudomonas aeruginosa infection. One of the main directions of new developments is research into the therapeutic properties of the vaccine and plasma of hyperimmunized donors for infections caused by Pseudomonas aeruginosa [15]. The theoretical basis for attempts to introduce vaccines or immune sera to treat infections caused by Pseudomonas aeruginosa was research conducted in the mid-50s. Studies have shown that antibodies in human γ-globulin preparations are protective against Pseudomonas aeruginosa infections in mice. Further studies were aimed at obtaining a safe immunogenic vaccine against Pseudomonas aeruginosa, effective against all types of infection, the immunogenicity of various virulence factors was considered, and various routes of vaccine administration were studied (oral, nasal). At the moment, antipseudomonal plasma is widely used in the treatment of patients with severe burns, chronic infections of the respiratory tract, and genitourinary system, which leads to a significant reduction in the mortality of these patients and a decrease in the incidence of sepsis [15].
Taking into account the experience of using immunotherapy in the treatment of this infection, we successfully used antipseudomonas human plasma in a patient with malignant otitis externa. A description of this clinical case is given below.
Patient P., 74 years old, was admitted to the ENT department of the Lugansk Republican Clinical Hospital with complaints of intense pain in both ears, radiating to the mastoid region, the angle of the lower jaw, and the temporal region.
According to the patient, the above complaints appeared about a month ago after washing the wax plugs with a cool solution. He sought medical help at his place of residence, was hospitalized in the ENT department, where he underwent a course of treatment for two weeks: antibiotic therapy (lincomycin 30% - 2.0 IM 2 times a day No. 5, ceftriaxone 1.0 IM 2 times a day No. 10), hyposensitizing therapy (30% sodium thiosulfate - 5.0 IV once a day No. 5), Trimistin ointment and ear drops with ciprofloxacin were used topically. A positive effect was noted, but 2 weeks after discharge the patient experienced a sharp deterioration in his condition, and therefore was referred for consultation to an ENT doctor at the Lugansk Republican Clinical Hospital.
On admission, blood pressure was 130/90 mm Hg. Art., pulse - 78 per minute. Body temperature 37.3 °C. When examining the ENT organs, the patient had a pronounced inflammatory process, swelling, infiltration of the skin of the external auditory canals, with an abundance of granulations on both sides, serous-purulent discharge, the presence of infiltrates that occupied the postauricular area, the parotid area and the angles of the lower jaws on both sides, pronounced pain syndrome. On the left, in the area of the superoposterior wall of the external auditory canal, there are foci with purulent fusion in the center (antral fistulas?). The eardrums are not visible. Hearing is sharply reduced on both sides (whispered speech - 0 m, spoken speech - 1.0 m, according to audiometry - conductive type hearing impairment). Other ENT organs are unremarkable.
Clinical blood test: erythrocytes - 4.81 × 1012/l, Hb - 149 g/l, leukocytes - 13.8 × 109/l, p - 9%, s - 68%, e - 1%, l - 18 %, m - 4%, ESR - 32 mm/h. Blood sugar - 4.6 mmol/l. Blood on RW is negative. Biochemical tests are normal.
When the patient underwent radiography of the mastoid processes according to Schüller with contrasting of the fistulous tracts, bilateral mastoiditis was diagnosed, and the presence of antral fistulas on the left was confirmed.
To exclude otogenic intracranial complications, the patient underwent magnetic resonance imaging of the brain with intravenous enhancement. Conclusion: predominantly internal, more on the left, mild hydrocephalus.
The results of a bacteriological examination of ear discharge upon admission revealed abundant growth of Pseudomonas aeruginosa, sensitive to ceftriaxone, ofloxacin, and norfloxacin.
Considering that the process began with inflammation of the external auditory canals, cultures from the ears revealed Pseudomonas aeruginosa, the presence of granulations, foci of bone destruction, the patient, according to the mandatory Friedman-Cohen criteria [14], was diagnosed with malignant bilateral otitis externa, complicated by mastoiditis with both sides.
Due to the ineffectiveness of the conservative treatment, the patient underwent bilateral antromastoidotomy. During the operation, the external auditory canal on the left in its bony part was detached with purulent exudate from the bone; it also contained a large number of granulations, which were taken for histological examination. On the left in the antrum there is liquid pus, the apical cells of the mastoid process are carious, the bone was softened, bleeding, samples were taken for histological examination. On the right in the antrum there is scanty serous discharge, granulations. The samples for histological examination contained granulation and bone tissue with focal inflammatory infiltrate.
There were no complications in the postoperative period. Antibacterial therapy was prescribed taking into account the antibiogram. Hyposensitizing therapy was carried out, Oflokain ointment, betadine were used topically, compresses on the behind-the-ear and parotid area with solutions of ectericide and dimexide in a dilution of 1:4, and a course of endoaural laser therapy. Repeated cultures of discharge from the ears revealed scant growth of Pseudomonas aeruginosa; it was not possible to achieve complete elimination of the pathogen during culture. At the same time, clinically, the discharge from the ears completely stopped, hearing improved: whispered speech in both ears - 1.0 m, spoken speech more than 6.0 m, upon discharge, the inflammatory process of the skin of the external auditory canals on both sides regressed.
The patient was hospitalized again 2 weeks later with complaints of renewed suppuration from the ears, itching in the ears, and decreased hearing. On examination, hyperemia and swelling of the skin, the presence of granulation tissue, purulent discharge in both external auditory canals.
The results of a bacteriological study of discharge from the ears indicate an abundant growth of Pseudomonas aeruginosa, but already insensitive to ceftriaxone, weakly sensitive to ofloxacin, norfloxacin. Considering the relapse and severity of the disease, the patient was prescribed a course of treatment with antipseudomonas human plasma. Plasma was administered intravenously, by drip, in strict adherence to the rules of asepsis and antisepsis at a daily dose of 3–6 ml per 1 kg of patient weight three times every other day [16]. There were no allergic reactions or complications to the administration of the blood product. Granulation tissue was removed from the external auditory canals, and betadine solution was used topically.
The patient was discharged from the department on the 10th day in satisfactory condition. Recommendations are given: avoid getting water in the ears, refuse to clean the ears, including with cotton swabs, contact an otolaryngologist when the first signs of the disease appear. During dynamic observation of the patient for two years, there were no relapses of the disease.
The presented results of the use of antipseudomonas human plasma in the treatment of malignant otitis externa showed the effectiveness of immunotherapy, which was expressed in a rapid and persistent clinical effect.
Considering the relevance of the treatment of diseases caused by Pseudomonas aeruginosa infection, we believe that our experience in the use of immunotherapy for this infection will arouse interest among clinicians of various specialties and will continue clinical research aimed at determining the most effective methods for treating Pseudomonas aeruginosa infection.
Literature
- Bobrov V. M. Necrotic (malignant) external otitis // Bulletin of otorhinolaryngology. 2011. No. 3. pp. 71–72.
- Meltzer PE, Kelemen G. Pyocyaneous osteomyelitis of the temporal bone, mandible and zygoma // Laryngoscope. 1959. 169. R. 1300–1316.
- Gardyga V.V., Bartsikhovsky A.I. Two observations of malignant external otitis // Journal of ear, nose and throat diseases. 1994. No. 2. P. 64–65.
- Ophir Handzel, Doron Halperin. Necrotizing (Malignant) External Otitis // Am Fam Physician. 2003. 15. Vol. 68(2). R. 309–312.
- Drew SJ, Himmelfarb R., Sciubba JJ Invasive (malignant) external otitis progressing to osteomyelitis of the temporomandibular joint: a case report // J Oral Maxillofac Surg. 1993. 51. R. 429–431.
- Dunaivitser B.I. Necrotizing external otitis // Bulletin of otorhinolaryngology. 1985. No. 1. P. 71–72.
- Rybalchenko K. D., Chekrygina N. I. Necrotizing external otitis in patients with diabetes mellitus // Bulletin of Otorhinolaryngology. 1981. No. 2. P. 69–70.
- Chastre J. Trouillet JL Problem pathogens (Pseudomonas aeruginosa and Acinetobacter) // Seminars in Respiratory Infectious. 2000. 15. R. 287–298.
- Kovacs K. Patterson DL, Yu VL Antimicrobial Therapy for Pseudomonas aeruginosa: Skin and Soft Tissue, Ear, and Eye Infections; Meningitis; and Clinical Syndromes of Febrile Neutropenic and HIV Patients // Infect Med. 1998. 15. R. 464–478.
- Kostyshin A. T. Our experience in treating patients with granulating external otitis // Journal of ear, nose and throat diseases. 1984. No. 1. pp. 64–65.
- Tacconelli E., Tumbarello M., Bertagnolio S. et al. Multidrug-resistant Pseudomonas aeruginosa bloodstream infections: analysis of trends in prevalence and epidemiology // Emerging Infectious Diseases. 2002. 8. R. 220–221.
- Cooper MA, Andrews JM, Wise R. Ciprofloxacin resistance developing during treatment of malignant otitis externa // J Antimicrob Chemother. 1993. 32. R. 163–164.
- Kozlov R. S. Nosocomial infections. Antibacterial therapy. Practical guide / Ed. L. S. Strachunsky, Yu. B. Belousov, S. N. Kozlov. M.: Publishing house RC "Pharmedinfo", 2002. pp. 143–146.
- Cohen D., Friedman P. The diagnostic criteria of malignant external otitis // Journal of Laryngology and Otology. 1987. Vol. 101(3). R. 216–221.
- Döring G., Pier GB Vaccines and immunotherapy against Pseudomonas aeruginosa // Vaccine, 2008. Vol. 26 (8). R. 1011–1024.
- Khvatov V. B., Zdanovskaya L. K., Bodrova G. N. Instructions for the use of antipseudomonas antitoxic human plasma (Plasma antipseudomonas antitoxicum human), approved by the Ministry of Health of the Russian Federation M. 1992.
V. G. Senchenko* T. M. Pristavko**, Candidate of Medical Sciences I. E. Berest**, 1, Candidate of Medical Sciences
* Lugansk Regional Clinical Hospital, Lugansk, Ukraine ** State Institution Lugansk State Medical University, Lugansk, Ukraine
1 Contact information