Thiazide diuretics are first-line drugs in the treatment of arterial hypertension and abnormalities in the cardiovascular system, which makes them one of the main pharmaceutical agents.
The main effect, as the name suggests, is the removal of excess fluid. This type of medicine is otherwise called diuretics.
Thiazide diuretics are considered the safest and at the same time effective among this category of drugs. They are used in the treatment of arterial hypertension, heart failure and a number of other diseases.
However, like other diuretics, they are not suitable for independent use; they require precise dosing and constant dynamic monitoring of the patient’s condition. Prescription is the prerogative of the doctor.
Classification of diuretic drugs by mechanism of action
Doctors and researchers distinguish the following groups of diuretics:
- drugs that effectively act at the level of the tubules in the kidneys, for example, mercury diuretics - Diacarb, Bumetonide, Eplerenone and Indapamide;
- medications that significantly increase blood circulation in the kidneys - Zufillin and Aminophylline;
- herbal diuretics from strawberry fruits, birch buds and torment leaves.
Based on their composition, diuretics can be divided into the following large groups:
- loop preparations consisting of sulfonamide derivatives. Furosemide, Ethacrynic acid, Torsemide;
- thiazide drugs from derivatives of thiazide substances and sulfonamide. Clopamide, Hydrochlorothiade, Cyclomethisiade;
- potassium-sparing medications made from non-sulfonamide-type compounds. Triamterene, Amiloride, Aldactone;
- osmotic agents as sulfonamide derivatives. These are, first of all, solutions of sodium chloride and glucose, used as hypertensive drugs, as well as Mannitol.
Mechanism of action of diuretics[edit | edit code]
The main thing in the mechanism of action of diuretics is their effect on the kidneys, the structural and functional unit - the nephron, on the processes that occur in it (glomerular filtration, tubular reabsorption, secretion).
To understand the mechanism of action of diuretics, let us briefly consider the process of urine formation. Each kidney contains about 1 million non-communicating nephron formations, consisting of a vascular glomerulus (glomerulus), glomerular capsule and tubules. In the renal glomerulus, plasma is filtered from the capillaries into the capsule cavity. The endothelium of the capillaries does not allow blood cells and proteins to pass through. The filtrate is called primary urine, which enters the kidney tubules from the glomerulus through the capsule. Filtration in the kidneys requires that the blood pressure in the glomerular capillaries exceed the oncotic pressure of the blood plasma. With a decrease in blood pressure, filtration in the glomeruli decreases; with an increase, on the contrary, it increases. The glomerular filtration rate depends not only on the blood supply to the kidneys, but also on the number of functioning nephrons.
Glomerular filtration in an adult averages 100 ml/min. During the day, 150-200 liters of fluid are filtered in the kidneys, and only 1.5-2 liters of urine are excreted, i.e. 99% of the primary urine is again absorbed (reabsorbed) in the tubules. The tubules are divided into proximal, which passes into the loop of the nephron (Henle) (V-shaped convoluted tube), and distal, through which urine passes from each nephron into the collecting ducts, and from them into the renal pelvis and through the ureters into the bladder.
The reabsorption process occurs throughout the nephron. In order to increase diuresis by 2 times, it is necessary to increase glomerular filtration by 2 times, which is practically impossible to do, or to reduce reabsorption by only 1%. Thus, urine formation can be significantly increased by reducing tubular reabsorption (Fig. 3.11). In addition to water, sodium, chlorine and potassium ions are reabsorbed in the tubules. It should be taken into account that in the tubules it is necessary to reduce the reabsorption of sodium ions, and water passively follows this osmotically active ion.
The effect of increasing filtration and decreasing reabsorption by 10% on the amount of diuresis
Sodium reabsorption in the kidney tubules occurs as follows. From the lumen of the tubule, Na+ enters the cell through the apical membrane. It is believed that sodium transport within the cell is carried out using a special carrier protein, the synthesis of which is regulated by aldosterone. Aldosterone binds to receptors in cells, is transferred to the nucleus and, influencing DNA, stimulates the synthesis of messenger RNA, which promotes the activation of the synthesis of the carrier protein in the ribosomes. Sodium, which entered the tubule cell, creates a fund (pool) of sodium, which is subsequently actively reabsorbed. Reabsorption is carried out using special pumps that are located on the basement membrane of the tubule wall cells. Several types of such pumps are known, one of them transports Na+ in exchange for K+. Others reabsorb Na+ together with SG or HCO~. This active transport of sodium is carried out due to the energy produced by mitochondria located near the basement membranes.
Reabsorption of sodium by epithelial cells of the renal tubular wall
About 70-80% of the total filtered Na+ is reabsorbed in the proximal tubules, followed by passive reabsorbment of water and SG. Carbonic anhydrase reabsorbs hydrogen carbonate (HCO3). The point of application of diuretics may be the proximal nephron, but their effect is insignificant, since a decrease in reabsorption in the proximal tubule entails a compensatory increase in it in the nephron loop and the distal tubule.
Active transport of Na+ and SG occurs in the nephron loop; its wall is impermeable to water. The action of diuretics primarily occurs in this part of the nephron; they are called loop diuretics. Blockade of sodium reabsorption in this department causes the greatest natriuresis.
Diagram of the nephron and localization of the action of diuretics (Farmakolopya, 2001): 1 - xanthines; 2 - diacarb; 3— mannitol; 4— furosemide, ethacrynic acid; 5 - dichlothiazide; 6— spirolactone, triamtren
Urine formation is completed in the distal nephron and collecting ducts. Transport processes here are controlled by hormonal influences. The sodium-retaining effect of the mineralocorticoid aldosterone and the water-retaining effect of the antidiuretic hormone (vasopressin) are manifested. Passive secretion of K+ from nephron cells occurs through the apical membrane along an electrochemical gradient. The distal tubule and collecting ducts can also be the point of application of diuretics (aldosterone antagonists, triamterene and others), but they are ineffective. Blocking Na+ reabsorption in this compartment, when about 90% of the filtered Na+ has already been reabsorbed, can increase its excretion by only 2-3% - the filtration charge. Sodium transport in the kidneys is also regulated by other factors. This is an atrial natriuretic hormone that is released from the atria when they are stretched, which causes an increase in glomerular filtration rate and inhibition of sodium reabsorption in the collecting ducts. In addition, there is natriuretic hormone - a low-molecular compound that enters the blood when volumoreceptors are stimulated and, like ouabain, blocks Na*, K+-ATPase in the kidneys, which reduces Na+ reabsorption. Substances that act as potential regulators of sodium excretion include estrogens, somatotropin, insulin (increase Na+ reabsorption), progesterone, parathyroidin, glucagon (reduce Na+ reabsorption). Factors that are formed in the kidneys (kinins, prostaglandins, dopamine, etc.) also act locally.
Considering the principles of functioning of the urinary system, it becomes clear that drugs that stimulate urination can directly affect the urinary function of the kidneys or change their hormonal regulation.
The use of diuretics, primarily as a means of symptomatic therapy aimed at reducing edema, also has an important pathogenetic effect on the complex chain of reactions in diseases that are accompanied by the retention of salts and water in the body.
There are more than 20 drugs in the arsenal of diuretics. Which of them should be preferred in a given situation should be helped by knowledge of pharmacokinetics, mechanism of action, possible side effects, and more.
Thiazide diuretics – what are they?
It is well known that any diuretic drugs negatively affect the salt balance in the body, since they remove a lot of useful substances during deurination. This complicates the functioning of the heart. Thiazide diuretics increase the excretion of urine from the body without limiting the patient's salt intake, even in cases of diagnosed heart failure.
The fundamental difference between diuretics of this group and the rest is a decrease in calcium production and an increase in sodium secretion in special parts of the nephron that are responsible for these processes. Thus, the exchange of sodium for potassium enzymes increases significantly, and it is excreted intensively through the genitourinary system.
All thiazide diuretics are taken in tablet form with plenty of water. The onset of action is noted within a couple of hours. The final withdrawal from the body will occur after 12 weeks of regular use.
The thiazide group is not as hard on the patient’s body as the loop group, due to which their effectiveness in time is reduced. But such diuretics are prescribed to absolutely everyone, except in cases of renal failure, in which the drug cannot overcome the resistance of the pathology.
More on the topic: How to take Trifas diuretic tablets?
Application in medicine
In medicine, diuretics are used to treat heart failure, arterial hypertension, influenza, liver cirrhosis, kidney disease, and hyperhydration. Some diuretics, such as acetazolamide, can slightly alkalinize the urine and are useful for increasing the excretion of various types of chemicals from the body, such as acetylsalicylic acid (aspirin) in cases of overdose or poisoning.
Common combinations
Diuretics are rarely prescribed as monotherapy. To achieve a lasting effect with a minimum number of adverse reactions, they are combined with other antihypertensive drugs. These can be two separate tablets or a complex medicine containing 2 active ingredients. Combined use with ACE inhibitors, calcium antagonists, sartans are the most preferred combinations (1). It is also advisable to prescribe thiazide diuretics and beta blockers.
Common combination drugs
| Active ingredients | Tradename |
| valsartan + hydrochlorothiazide |
|
| irbesartan + hydrochlorothiazide |
|
| losartan + hydrochlorothiazide |
|
| captopril + hydrochlorothiazide | |
| lisinopril + hydrochlorothiazide |
|
| ramipril + hydrochlorothiazide |
|
| enalapril + hydrochlorothiazide |
|
| lisinopril + indapamide | |
| amplodipine + valsartan + hydrochlorothiazide |
|
| amplodipine + indapamide |
Thiazide diuretics in the treatment of arterial hypertension
In June 2007, at the European Congress on Hypertension in Milan (Italy), new European guidelines for the treatment of arterial hypertension (HTN) were announced. Particular attention of cardiologists was directed to the place of certain classes of drugs in treatment regimens for hypertension.
6 rational combinations of antihypertensive drugs have been proposed [1]:
- thiazide diuretic + angiotensin-converting enzyme (ACE) inhibitor;
- thiazide diuretic + angiotensin receptor blocker;
- calcium antagonist + ACE inhibitor;
- calcium antagonist + angiotensin receptor blocker;
- calcium antagonist + thiazide diuretic;
- beta blocker + dihydropyridine calcium antagonist.
Based on the above, we can conclude that calcium antagonists (4 times) and thiazide diuretics (3 times) appear most often in combinations.
Thiazide diuretics have long been used as agents for the treatment of hypertension. In the 2007 European guidelines, the target groups for whom diuretics are preferred include elderly patients with systolic hypertension as well as heart failure [1].
However, the use of medium and high doses of thiazide diuretics is currently considered undesirable: for example, hydrochlorothiazide at a dose of 100 mg/day increases the risk of sudden death, and at doses of 50–100 mg/day does not prevent the development of coronary heart disease (CHD). In this regard, the recommended doses of thiazide diuretics are currently 12.5–25 mg/day, which do not always achieve an adequate diuretic and antihypertensive effect [2]. In addition, limiting the doses of thiazide diuretics is also associated with their negative effect on carbohydrate, fat and purine metabolism [3]. Therefore, in the 2007 European recommendations, gout was included as absolute contraindications to the use of thiazide diuretics, and metabolic syndrome and impaired glucose tolerance were included as relative contraindications. In addition, special emphasis is placed on the fact that high doses of diuretics cannot be prescribed to pregnant women due to the possibility of reducing circulating blood volume (CBV) and deteriorating blood supply to the fetus. However, we should not forget that diuretics can delay the development of chronic heart failure in patients with hypertension (Davis BR, 2006).
Thus, it is obvious that the scope of application of thiazide diuretics in the treatment of hypertension is quite limited. In this regard, the thiazide-like diuretic indapamide is of particular interest.
Indapamide has a dual effect, due to which it has a short-term and long-term antihypertensive effect. The short-term effect is associated with the effect of the drug on the proximal part of the distal tubules of the nephron and represents a natriuretic effect characteristic of representatives of the diuretic class as a whole. As for the long-term antihypertensive effect, it is unique to indapamide and occurs due to a direct vasodilating effect on the smooth muscle cells of the vascular wall [4].
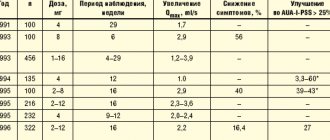
The antihypertensive effect of indapamide retard 1.5 mg was compared with amlodipine (5 mg/day) and hydrochlorothiazide (25 mg/day) in a study of 605 patients with hypertension treated with the above drugs for 3 months. The number of patients responding to monotherapy was slightly higher in the indapamide-retard group (75.3%) compared with the amlodipine (66.9%) and hydrochlorothiazide (67.3%) groups. In the subgroup of patients with isolated systolic hypertension, a similar trend was observed: the number of respondents in the indapamide-retard group was 84.2%, while in the amlodipine group - 80%, hydrochlorothiazide - 71.4% [5].
The multicenter LIVE (Left ventricle hypertrophy: Indapamide Versus Enalapril) study examined the effect of indapamide and enalapril therapy on regression of left ventricular myocardial mass (LVMM). 505 patients (255 - indapamide group; 250 - enalapril group) with mild and moderate hypertension were prescribed indapamide retard 1.5 mg/day or enalapril at a dose of 20 mg once a day for 1 year. Therapy with indapamide led to a significant decrease in LVMM (p < 0.001); similar results were not obtained in the enalapril group. Indapamide also reduced the severity of left ventricular hypertrophy (LVH) to a greater extent than enalapril (p < 0.049) [6, 7].
Thiazide diuretics have been prescribed in combination with ACE inhibitors for a very long time: many pharmaceutical companies have even developed fixed combinations of these components. In a large number of studies, the combination of indapamide with perindopril also showed good results. However, there are not many studies on the effectiveness of combinations of indapamide with other classes of the drug.
In this regard, we found the work of Hashimoto J. et al interesting. [8], who added indapamide at a dose of 1 mg to 76 patients receiving ACE inhibitors, angiotensin receptor blockers, and calcium antagonists as monotherapy, but failed to achieve target blood pressure (BP) values with this treatment. During 4 weeks of combination therapy in these three groups, the dynamics of the level of 24-hour blood pressure monitoring, home blood pressure measurements, and random blood pressure measurements were assessed. In all groups, a significant decrease in systolic blood pressure (SBP) and diastolic blood pressure (DBP) was noted. The decrease in SBP in the evening and pulse blood pressure was significantly more pronounced in the angiotensin receptor blocker + indapamide group compared to the calcium antagonist + indapamide group. Thus, the addition of indapamide to antihypertensive therapy led to an additional hypotensive effect that lasted 24 hours.
Until recently, only three classes of drugs were thought to have nephroprotective effects: ACE inhibitors, angiotensin receptor blockers, and calcium antagonists (mainly phenylalkylamines). The nephroprotective effect of thiazide-like diuretics was demonstrated in the NESTOR study [9]. In 570 patients with hypertension and type 2 diabetes mellitus, a comparative study of the effect of indapamide retard 1.5 mg and enalapril 10 mg on the severity of microalbuminuria (MAU) was carried out during one-year therapy. There was a decrease in MAU by 37% in the enalapril group and by 45% in the indapamide-retard group. Thus, the nephroprotective effect of indapamide retard 1.5 mg turned out to be comparable and even slightly higher than that of enalapril.
Another study examined the effect of indapamide retard at a dose of 1.5 mg prescribed for 3 months, compared with placebo, on 24-hour blood pressure monitoring, carbohydrate and lipid metabolism in patients with type 2 diabetes mellitus [10]. A significant decrease in average daily blood pressure was detected in the indapamide group compared to placebo. In addition, there was no effect of the therapy on electrolytes, creatinine, lipid spectrum, uric acid, liver transaminases, insulin levels, glycosylated hemoglobin and glucose tolerance test results.
Considering that diuretics have long established themselves as the drug of choice for the treatment of elderly patients, especially those with isolated systolic hypertension (ISAH). The multicenter X-CELLENT study included 1,758 patients with systolic-diastolic hypertension or ISAH, who were then randomized into 4 groups, which received monotherapy with indapamide retard 1.5 mg/day, amlodipine 5 mg/day, candesartan cilexetil 8 mg/day and placebo for 3 months. Compared to the placebo group, a significant decrease in blood pressure was noted in all groups. The advantage of indapamide in patients with ISAH was the virtually no effect of the drug on normal DBP values while reducing SBP; the remaining drugs reduced both SBP and DBP. In addition, in this group of patients, indapamide retard reduced average daily SBP to a greater extent than amlodipine. All three types of therapy were well tolerated [11].
As we indicated above, a dose of hydrochlorothiazide of 12.5–25 mg/day is considered metabolically neutral. In the work of A. A. Semenkin et al. A comparative study of the antihypertensive effectiveness and metabolic effects of indapamide retard (1.5 mg/day) and hydrochlorothiazide (25 mg/day) was conducted. Despite the comparable antihypertensive effect, in the group of patients receiving hydrochlorothiazide, after 3 months there was a significant increase in triglyceride levels by 15.3% (p < 0.05) and glucose by 12.2% (p < 0.05), and also a significant deterioration in endothelium-dependent vasodilation by 17% (p < 0.05) [12].
Of interest is the potential expansion of indications for the use of indapamide, in particular, its use in the treatment of chronic heart failure accompanied by edema syndrome. In one recent study in patients with persistent peripheral edema, indapamide 2 mg was added to furosemide (40–120 mg/day), which resulted in a significantly greater diuretic effect without a significant effect on plasma potassium and creatinine levels [13].
Thus, the original indapamide has more than convincingly proven its antihypertensive effectiveness and organoprotective properties during research. In an attempt to combine low cost with high quality of the drug to provide the majority of patients with hypertension with drugs of adequate action, modern generics of indapamide and, in particular, the drug “Ravel SR”, produced in a dose of 1.5 mg, are of particular interest. The drug has successfully proven itself after a trial in Slovenia in 2005–2006. study [4], which examined its antihypertensive efficacy and tolerability. The drug was prescribed to 1419 patients (58.1% women, mean age 61.9 ± 11.6 years), who showed a decrease in SBP by 14.1% and DBP by 11.1%. The development of adverse events while taking Ravel SR was noted in only 2.5% of patients (the most common were dry mouth and dizziness - 0.42% each, and 1 patient required correction of potassium levels due to the development of hypokalemia without discontinuation of the drug) .
The effectiveness and tolerability of Ravel SR was also studied in domestic studies. S. V. Nedogoda et al. [14] compared therapy with Ravel SR 1.5 mg/day and hydrochlorothiazide 25 mg in patients with hypertension and obesity. Patients of the 1st group received Ravel SR for 6 months, patients of the 2nd group were prescribed hydrochlorothiazide at a dose of 25 mg/day for the first 3 months, and then they were transferred to Ravel SR (3 months). The results of the study showed that while taking Ravel SR, achieving target blood pressure values occurred 15% more often than with hydrochlorothiazide. It was noted that only on therapy with Ravel SR there was an improvement in vascular elasticity (as assessed by pulse wave velocity) and a decrease in myocardial hypertrophy, as well as an improvement in carbohydrate and lipid metabolism.
Also of interest are the results of the BOLERO program (Basic treatment and antihypertensive effect: the drug “Ravel SR” in patients with arterial hypertension), aimed at studying the antihypertensive effectiveness of the slow-release form of the drug and its effect on quality of life. It was shown that the use of indapamide retard for 2 months led to a decrease in SBP and DBP in men by 18%, and in women by 15%. During treatment, cardiovascular risk decreased to the same extent in men and women, and the improvement in quality of life was more noticeable in the group of women [15].
The emergence of each new high-quality and safe generic drug is a step towards ensuring that Russian patients demonstrate higher adherence to hypertension treatment. Currently, patients with hypertension in the Russian Federation who have a target blood pressure level do not exceed 5–15% of the population, while in Western Europe there are more than 30% of such patients. The drug "Ravel SR" (indapamide retard) 1.5 mg as an antihypertensive drug with a mild diuretic effect has every opportunity to expand the boundaries of the use of diuretics outlined by modern recommendations for the treatment of hypertension.
For questions regarding literature, please contact the editor.
D. A. Napalkov , Candidate of Medical Sciences MMA named after. I. M. Sechenova , Moscow
Medicinal properties of the thiazide group
Thiazide diuretics are intended for the treatment of heart and vascular diseases. Based on the variety and their class, they can be prescribed for multiple complications of cardiovascular pathologies.
The main properties of thiazide-type diuretics are:
| № | Helpful information |
| 1 | In the treatment of hypertension, diuretics based on thiazide derivatives have been used for a very long time, and treatment with thiazide-like analogues has not yet been invented. In world medicine, thiazide diuretics are the first line in the treatment of hypertension. The main property of this group in the fight against the disease is to reduce the risk of heart attack or stroke, cardiac arrest, as well as in cases of heart failure of any severity |
| 2 | for the treatment of swelling, thiazides reduce hepatic and renal edema, cardiac type, as well as swelling with regular use of glucocorticoids. These medications must be taken very carefully in cases of acute heart and kidney failure, in which the optimal choice would be treatment with loop-type diuretics |
| 3 | in order to prevent the formation of stones and other concretions in the renal system, the main medicinal property of this group is used, which is aimed at reducing the level of calcium excretion from the kidneys, which generally leads to its decrease in the body. Thus, all calcium deposits in the form of stones and other formations in the kidneys will not occur |
| 4 | in the treatment of diabetes (not diabetes!) of the nephrogenic type, the amount of circulating blood decreases, which promotes intensive extraction of moisture in the renal tubules |
Classification of diuretics
Diuretics are divided into 5 main classes of substances: thiazide, loop, osmotic, potassium-sparing diuretics and carbonic anhydrase inhibitors. Next, let's look in a little more detail at all of them.
Thiazide diuretics
Thiazide diuretics are a special class of diuretics that are most often used to treat hypertension and edema (caused, for example, by heart, liver, or kidney failure). This group of diuretics is homogeneous in pharmacological action, and the substances differ from each other only in the duration and strength of action.
Main representatives: indapamide, hydrochlorothiazide.
Loop diuretics
Loop diuretics are the most potent of all diuretics available in clinical practice. Most often, loop diuretics are used in the treatment of edema of various origins.
Main representatives: furosemide, ethacrynic acid.
Potassium-sparing diuretics
Potassium-sparing diuretics are a special class of diuretics that do not promote the excretion of potassium in the urine from the body. Potassium-sparing diuretics are most often used as adjuvant therapy in the management of congestive heart failure and the treatment of hypertension.
Main representatives: spironolactone, triamterene
Osmotic diuretics
Osmotic diuretics are a special type of diuretic that inhibit the reabsorption of water and sodium (Na) in the body. Osmotic diuretics, from a pharmacological point of view, are inert substances that are administered intravenously. They increase blood osmolarity and enhance renal filtration.
Main representative: mannitol.
Carbonic anhydrase inhibitors
Carbonic anhydrase inhibitors are a type of diuretic that, paradoxically, are not used as diuretics (diuretics) on their own. Carbonic anhydrase inhibitors are mainly used for glaucoma.
Main representative: acetazolamide.
List of thiazide drugs
At the moment, there are a lot of diuretic drugs of various types and effects on pharmacy shelves and in manufacturers’ catalogs. It is important to get a doctor's recommendation or prescription before purchasing any of these, especially if thiazide diuretics are needed.
Dichlorothiazide
For hypertension, Dichlorothiazide is prescribed, but in the presence of renal or liver failure, it is not recommended for use by specialists. The drug is available in capsules or tablets. Standard doses, when taken regularly, improve the condition already on the fourth day, but if you reduce the recommended dosage, the effectiveness may disappear completely.
With long-term use of Dichlorothiazide, hypertension is reduced, as is the likelihood of a heart attack. There are some side effects that you should be aware of before you start taking it, in particular, with low potassium levels, an increase in sugar levels is possible, but by reducing the dosage this effect can be avoided.
Indapamide
Indapamide is much more effective than Dichlorothiazide, it does not affect metabolism at all and is completely safe. The drug is indifferent to the level of glucose, cholesterol or insulin in the patient’s blood. Analogs are Acripamide, Indap and Arifon Retard.
These drugs have proven themselves to be effective in cases of renal failure, but can cause headaches and disruptions in the functioning of the nervous system.
More on the topic: What gentle diuretics help with edema?
Chlorothiazide
Chlorothiazide is the very first thiazide-type diuretic. The weakest and most gentle of all diuretics in this group, it is gentle on the kidneys and heart. It is usually produced in tablets of 500g and 250g.
Bendroflumethiazide
Bendroflumethiazide is more effective than Chlorothiazide, but has a lot of contraindications. The most significant of them are systemic lupus erythematosus, as well as the period of lactation and breastfeeding.
Hydroflumethiazide
Hydroflumethiazide is actively excreted by the kidneys, which limits its use in pathologies of this system. In cases of extreme necessity, the smallest dosage should be taken. As a rule, the product is available in the form of 50 gram tablets. Reception is carried out once a day.
Chlorthalidone
Chlorthalidone actively lowers blood pressure, requiring absolute health of the patient's renal system. 15 mg tablets are very effective; a doctor’s recommendation is required before taking them.
Classification of diuretics
Diuretics are divided into classifications:
- According to the time of onset of the expected effect (from half an hour, for example, “Urea”, “Furosemide” to several days - “Spironolactone”, “Eplerenone”);
- According to the duration of action of the drug (up to 4 hours, for example, “Ethacrynic acid”, up to 4 days “Chlorthalidone”);
- According to the impact scale (weak - "Aldactone", "Triamterene", medium - "Hydrochlorothiazide", "Hygroton", strong drugs - "Lasix", "Uregit").
There are different types of diuretics, the main ones are divided into 4 separate groups:
1) Saluretics are a very large group of diuretics, it includes loop diuretics, carbonic anhydrase inhibitors, thiazide-like and thiazide drugs. Tablets and powders of this group are produced under the following names:
- Diacarb;
- Furosemide;
- Dehydratin;
- Priretanide;
- Indapamed;
- Fonurit and others.
2) Osmotic drugs - are distinguished by their ability to normalize plasma pressure in a short time. They are extremely effective for pulmonary and cerebral edema, peritonitis, glaucoma, burns, and drug poisoning. Osmotic diuretics:
- Sorbitol;
- beckons;
- Urea.
3) Potassium-sparing diuretics are indicated for hypertensive patients; for all their effectiveness in removing fluid, they still allow potassium salts to remain in the body. Names of drugs in this group:
- Amiloride;
- Triamteron;
- Spironolactone;
- Aldactone;
- Triamour.
4) Calcium-sparing diuretics – effective for osteoporosis and hypertension. From the name of the group it is clear that these drugs ensure that calcium is not excreted with excess fluid. These diuretics are indicated for anyone who suffers from excessive stress on the body’s skeleton and brittle bones. The drugs are called:
- Pamid;
- Arindap;
- Indap;
- Indiur;
- Retapres;
- Hygroton.
Contraindications for use
When treating with thiazide diuretics, it is important to know the existing contraindications:
- gout caused by a metabolic failure. Acceleration of processes will lead to exacerbation of the disease;
- hyperuricemia, a disease characterized by large amounts of uric acid in the body. Removing moisture from the body will increase the concentration of acid;
- hyponatremia and hypokalemia, in which the lack of corresponding substances in the body increases with the excreted fluid;
- hypercalcemia, when there is too much calcium in the body and possible formation of stones and other formations in the renal system, which leads to complications of urolithiasis;
- heart and kidney failure, acute form of the disease. Taking thiazides is strictly contraindicated, since the kidneys cannot cope with the increased volume of incoming water;
- Addison's disease is an inflammatory process in the adrenal cortex, leading to the cessation of the synthesis of corticosteroids.
Side effects
Taking TZ can cause:
- darkening of the eyes, dizziness;
- general weakness;
- abdominal pain, nausea and diarrhea;
- decreased visual acuity;
- increased concentration of uric acid;
- increased calcium levels;
At the beginning of a course of taking thiazides, it is not recommended to perform complex work or drive a car due to a decrease in concentration and reaction speed. Calcium losses should be replenished by taking drugs simultaneously with TZ: Asparkam, Panangin, Potassium normin. Include dried apricots, nuts, and honey in your diet.
The patient's diet should include dried apricots, honey and nuts
When using drugs of the TD class, it is necessary to control the balance of microelements in the body. Diuretics can cause potassium or sodium levels in the blood to fall below normal levels.
If it is impossible to discontinue the drug, a special serum or other means are prescribed to restore potassium balance.
If, as a result of taking thiazide diuretics, changes in the composition of the blood plasma occur (the risk of blood clots has increased), then they will have to be discontinued. If the concentration of uric acid increases, which threatens kidney damage and the development of arthritis, then thiazide diuretics should be abandoned.
Currently generally accepted recommendations for the treatment of arterial hypertension (AH) [1] imply the use of representatives of 5 classes of antihypertensive drugs as the main drugs, among which thiazide diuretics (TDs) still retain their position. Like other antihypertensive drugs, they are not completely free from certain undesirable effects, which, however, are not a reason to refuse them. The prescription of TDs in the treatment of hypertension is justified from a pathogenetic point of view, supported by long-term experience of their use in clinical practice and the results of controlled clinical studies, indicating a significant positive effect of this class of drugs on the long-term prognosis of patients.
Why did TD begin to be used for the treatment of hypertension?
Back in the first half of the twentieth century. sodium and water retention was recognized as one of the central components of the pathogenesis of most clinical variants of hypertension; moreover, it was often given a decisive role in the formation of a persistent increase in blood pressure (BP) [2]. Before the advent of truly effective antihypertensive drugs in patients with hypertension, including severe hypertension, it was possible to achieve a noticeable reduction in blood pressure by sharply limiting the consumption of table salt. A series of studies by Wallace Kempner in the 1940s is considered classic. demonstrated the possibility of significantly reducing blood pressure in patients with high hypertension, including kidney disease, by changing the diet, which meant eliminating foods containing salt. Patients received only rice and fruit; at the beginning of the observation period, they tolerated the complete cessation of access to table salt very poorly (even to the point of suicide attempts). Subsequently, many people began to feel disgusted by salty food, which often coincided with a decrease in systolic blood pressure (SBP) and diastolic blood pressure (DBP) [3].
TD is the product of a targeted search for approaches to controlling the function of tubular transport systems (interestingly, this search was initially aimed at developing agents that slow down the excretion of expensive penicillin and, therefore, prolong its action). The ability of TDs to reduce blood pressure and, in certain doses, to significantly increase diuresis is determined by their effect on the Na+/Cl- transporter of the distal nephron tubules [4]. By interacting with the Cl-binding center of the transporter, these drugs cause an increase in the excretion of sodium and chloride ions, and, consequently, an increase in the clearance of osmotically bound water, while the pre- and afterload on the left ventricular myocardium decreases, and blood pressure decreases.
The significance of the described mechanisms in the development of the antihypertensive effect of TD was established back in the late 1950s – early 1960s. Wilson IM et al. (1959) [5] demonstrated that in patients with hypertension, taking chlorothiazide is accompanied by a decrease in blood plasma volume, body weight, and an increase in urinary excretion of sodium, chloridione and potassium; in parallel, most patients experienced a decrease in blood pressure. In most patients, these effects of chlorothiazide persisted even with long-term (12 months) use of this drug, but disappeared relatively quickly after its discontinuation. Thus, it can be argued that the antihypertensive effect of TDs is determined primarily by their ability to stimulate natriuresis and the excretion of osmotically bound water.
Have the benefits of TD been confirmed in controlled clinical trials?
TD is a class of antihypertensive drugs, the use of which has been able to justify the need for continuous treatment of hypertension with the achievement and maintenance of target blood pressure values. It is well known that until the second half of the 1970s. The practice of treating hypertension primarily meant stopping hypertensive crises and lowering blood pressure in a situation where its increase was accompanied by a deterioration in well-being, for example, a headache. The benefit of chronic use of antihypertensive drugs was considered not obvious, and in some categories of patients (for example, the elderly) even dangerous. However, in the early 1970s. Freis ED, comparing outcomes in groups of patients who received constant antihypertensive therapy (its main component was hydralazine) or placebo, showed a significant difference in the incidence of cerebral strokes, which indicated the need for a constant reduction in blood pressure [6]. These data were obtained as part of a large study, the Veterans Administration Cooperative Study, the results of which also showed a significant reduction in the incidence of ECG abnormalities, achieved through the constant use of antihypertensive drugs, including hydrochlorothiazide (HCTZ) [7]. Thus, the incidence of left ventricular hypertrophy, registered on the basis of an increase in the Sokolov-Lyon index > 35 mm, was 28% in those taking placebo and 6% in the group of patients receiving antihypertensive drugs (p < 0.005). Moreover, the Veterans Administration Cooperative Study demonstrated that long-term use of antihypertensive treatment regimens including HCTZ can reduce the Sokolov-Lyon index, indicating regression of left ventricular hypertrophy: the incidence of this effect was 32% in those treated and 6% in those taking placebo (p < 0.005).
The Hypertension Detection and Follow-up Program study, conducted at 14 US clinical centers, included 10,940 patients with previously untreated hypertension aged 30 to 69 years. Patients were randomized to the then generally accepted antihypertensive therapy regimen (taking an antihypertensive drug if clinically indicated) or to continuous use of antihypertensive drugs that ensured maintenance of DBP < 90 mmHg. Art. A five-year follow-up of patients continuously receiving antihypertensive drugs was designed to confirm or refute the benefit of continuous drug normalization of blood pressure in terms of its effect on mortality. The majority of patients enrolled in the Hypertension Detection and Follow-up Program study were receiving HCTZ; If necessary, other antihypertensive drugs were added.
Contrary to the initial belief that continuous use of antihypertensive drugs, especially those with a diuretic effect, would be poorly tolerated by patients, more than 80% of patients randomized to continuous antihypertensive therapy were adherent to it and more than 75% of them achieved target DBP [8 ]. Moreover, chronic antihypertensive therapy using HCTZ was found to achieve a significant reduction in overall mortality compared with those receiving episodic antihypertensive therapy; this difference remained statistically significant regardless of the degree of blood pressure increase, age, sex, and race [9]. The prognostic advantages of continuous antihypertensive therapy were explained primarily by a significant decrease in blood pressure compared with the group where antihypertensive drugs were taken occasionally [10].
TD is a class of antihypertensive drugs, thanks to which it was possible to radically change the fate of patients with isolated systolic hypertension, demonstrating that they require constant antihypertensive therapy (until the early 1990s, they were practically not given due to the fact that it was considered dangerous, and An increase in blood pressure with age was considered as a variant of the norm). In the SHEP study, patients with isolated systolic hypertension over the age of 60 years were randomized to receive TD chlorthalidone (12.5–25 mg) or placebo. The follow-up period was 5 years. The primary endpoint was any new cardiovascular complication. Treatment with chlorthalidone was accompanied by a reduction in the incidence of non-fatal cerebral stroke by 37%, non-fatal acute myocardial infarction by 33%, and chronic heart failure (left ventricular) by 54%. In addition, a 25% reduction in the number of transient ischemic attacks, as well as overall (13%), cardiovascular (20%), cerebrovascular (29%) and coronary (15%) mortality was recorded [11]. The achieved improvement in cardiovascular prognosis persisted 14 years after the end of the study [12].
The well-known large controlled trial ALLHAT, the results of which remain one of the main events in cardiology of the 2000s, was planned with the aim of possibly demonstrating the benefits of newer classes of antihypertensive drugs compared with TD (ACE inhibitor, long-acting dihydropyridine calcium antagonist, α- adrenergic blocker) from the point of view of the effect on cardiovascular prognosis in patients with hypertension who had other risk factors. However, neither the ACE inhibitor nor the long-acting dihydropyridine calcium antagonist reduced the likelihood of the primary endpoint of nonfatal acute myocardial infarction and cardiovascular death more than TD, and the α-blocker did not. In comparison, it even worsened the cardiovascular prognosis: in particular, with its use, a significant increase in the number of new cases of chronic heart failure was noted [13]. The prognostic effectiveness of TD in the ALLHAT study did not depend on the race of the patient (the large number of included African Americans initially caused some criticism due to the fact that in this category of hypertensive patients TD is obviously superior in effectiveness to other classes of antihypertensive drugs) [14].
Thus, the rationale for the need for continuous treatment of hypertension is largely related to clinical studies in which TDs were used. Both when compared with true placebo and when compared with other classes of antihypertensive drugs, TDs have demonstrated the ability to significantly reduce the risk of disabling and potentially fatal cardiovascular events.
What are the possible limitations for prescribing TD for hypertension?
The use of TD, like other classes of antihypertensive drugs, may be associated with the development of certain adverse events. Thus, it is well known that taking TD can provoke the development of gouty arthritis [15]. A 52-year follow-up of women enrolled in the Framingham Heart Study [16] showed that TD use was associated with a 2.39-fold increase in the risk of gouty arthritis, but was not the most significant determinant of articular gout (its risk increased by 2.74). times with increasing age for every 5 years and 3.1 times with consumption of more than 200 ml of ethanol per week). However, this does not mean that TDs themselves cause uric acid metabolic disorders: it is obvious that they aggravate the already existing urate dysmetabolism, which is widespread in the general population and makes a certain contribution to the formation of essential hypertension [17, 18]. Obviously, in patients with hyperuricemia, TD can be prescribed only after the dose of allopurinol has been adjusted, and only in a situation where the patient is on a low-purine diet.
Most of the adverse events associated with the use of TD (erectile dysfunction, worsening metabolic disorders) are caused by a decrease in serum potassium concentration that occurs in some cases. According to large controlled studies, the incidence of TD-induced hypokalemia is generally low and does not exceed 8% [19]. It must be emphasized that increasing potassium intake with food and taking medications containing potassium can reduce the incidence of TD-induced (or more often aggravated in the presence of more significant predisposing factors: type 2 diabetes mellitus (T2DM) and smoking) erectile dysfunction [20]. In addition, the vast majority of patients receiving TDs today take them in combination with ACE inhibitors or angiotensin II receptor blockers, which are known to significantly reduce the likelihood of hypokalemia.
A decrease in serum potassium concentration and metabolic disorders are observed in the vast majority of cases when TD is used in doses significantly higher than currently recommended for mono and combination therapy. For example, in a systematic review by Zillich AJ et al. (2006) [21], which summarized 59 clinical studies, the maximum dose of chlorthalidone was 100 mg/day, and HCTZ was 400 mg/day (i.e., 16 times more than the maximum dose that is currently usually used for the treatment of hypertension ).
T2DM associated with the use of TD - a danger that can be controlled?
Noted in some controlled clinical trials, for example in ASCOT-BPLA [22], an increase in the number of new cases of T2DM in groups of patients taking TD has become the basis for attempts to reconsider the role of this class of antihypertensive drugs in the treatment of hypertension and is considered as an argument in favor of their exclusion number of first line funds. This point of view is obviously not justified, if only because the greatest risk of T2DM was found when TD was combined with α-blockers, which themselves significantly increase the likelihood of clinically obvious disorders of carbohydrate metabolism.
It is known that the formation of T2DM associated with the intake of TD is determined by a decrease in serum potassium concentration, causing an increase in insulin resistance and a disruption of the phasicity of insulin secretion by pancreatic α-cells [23]. An analysis of the SHEP study population published in 2008 [24] showed that a 0.5 mEq/L decrease in serum potassium concentration was associated with a 45% increase in the risk of T2DM (p < 0.001). Moreover, the likelihood of T2DM increased maximally during the first year of chlorthalidone use, thus being associated with initial changes in potassium concentrations. If hypokalemia is not observed at the beginning of TD treatment, the factors leading to it are eliminated (for example, concomitantly used loop diuretics in large doses), and the patient receives potassium-containing drugs, the likelihood of TD-induced diabetes is most likely low.
In addition, T2DM associated with the use of TD apparently does not lead to a significant deterioration in the prognosis of patients. In the previously mentioned SHEP study, the presence of T2DM at baseline or its development during follow-up was associated with a significant increase in mortality. However, in the group of patients in whom the development of T2DM was associated with taking the TD chlorthalidone, there was no increase in overall and cardiovascular mortality [25]. It should be noted that patients who had T2DM and received TD demonstrated the lowest cardiovascular and overall mortality rates.
Thus, TD should not be considered as drugs with a clear “diabetogenic” effect. They obviously should not be used primarily as monotherapy in patients with metabolic syndrome and/or with established insulin resistance, as well as in combination with β-blockers, especially those without cardioselectivity. The increased likelihood of T2DM observed in some categories of patients receiving TD generally reflects the scale of the epidemic of this disease and the conditions that predispose to its development.
What are the indications for the use of TD in hypertension?
Currently, the vast majority of patients with hypertension require combination antihypertensive therapy at the first stage of treatment[26]. TD, in particular HCTZ, is almost always included in combinations as the second or third drug. It must be borne in mind that their combination with ACE inhibitors and especially with angiotensin II receptor blockers makes it possible to achieve almost complete neutralization of negative metabolic effects [27]. In addition, the use of HCTZ, which makes it possible to control natriuresis, disorders of which still remain one of the central mechanisms of the development of hypertension, allows for a greater reduction in SBP, which is especially important for patients with high/very high risk hypertension. HCTZ also demonstrates significant advantages in hypertension associated with chronic heart failure. In this regard, despite the emergence of new classes of antihypertensive drugs, the history of the use of TD in hypertension will undoubtedly continue.
Reception features
All thiazides should be taken with caution and only on the recommendation of the treating physician. A thiazide-type diuretic is gentle on other systems in the body, but if the rules of administration are violated or the dosage is not controlled by a doctor, irreparable harm can be caused. Each administration action must be checked for compliance with the instructions for use included by the manufacturer in each package.
Before starting treatment with thiazides, it is worth undergoing an additional examination of the body in order to identify diseases from the list of contraindications. If the patient's general condition is severe, and also based on the form of hypertension, the effect of the medicine may be slightly different than with conventional treatment. In some cases, taking the medication is accompanied by a noticeable improvement and effect on the first day, and sometimes you have to wait a week before the first progress.
More on the topic: The principle of action of the diuretic Triampur
Drugs that can provoke hyperglycemia
Corticosteroids
Glucocorticosteroids can antagonize the action of insulin and stimulate gluconeogenesis, especially in the liver, leading to an overall increase in glucose production [1]. With normal carbohydrate metabolism, this property of steroids is not accompanied by changes in glycemia: the beta cells of the pancreas are able to produce sufficient amounts of insulin to compensate for excess glucose. However, in diabetes mellitus, when insulin levels are reduced and tissue sensitivity to it is impaired, the body is not able to neutralize the effect of steroids on glucose metabolism. Therefore, while taking corticosteroids with concomitant hyperglycemia in patients with diabetes or prediabetes (impaired glucose tolerance), blood glucose levels may increase and the need for insulin or oral antidiabetic drugs may increase [1, 2].
The severity of the hyperglycemic effect varies among corticosteroids, with prednisolone and dexamethasone having the most potent effects. However, there are limitations to systemic administration of most steroids [3].
Restrictions:
- Prednisolone, methylprednisolone, dexamethasone and betamethasone are contraindicated for use in diabetes mellitus
- Hydrocortisone is prohibited for decompensated severe diabetes
- Triamcinolone is approved for disorders of carbohydrate metabolism, however, the instructions for use emphasize the likelihood of developing diabetes mellitus while taking the drug [3].
Atypical antipsychotic drugs
Drugs in this group are quite widely used to treat schizophrenia and more common mental disorders, such as recurrent depression. They can exhibit a number of serious side effects, including impaired glucose metabolism. Its severity can be so great that while taking antipsychotics, there is a possibility of developing diabetes mellitus or even diabetic ketoacidosis [1].
It is believed that hyperglycemia while taking antipsychotics develops due to changes in the regulation of glucose and insulin levels, as well as disorders of lipid metabolism. The ability of drugs in this group to stimulate appetite and promote weight gain plays a certain role. With increasing weight, the volume of adipose tissue sharply increases, which leads to a decrease in insulin sensitivity and, as a consequence, to the development of diabetes mellitus [4]. It is known that with every kilogram of excess weight, the risk of type 2 diabetes increases by 4.5% [4].
It should be noted that the severity of the negative effect of atypical antipsychotics on carbohydrate metabolism varies. Olanzapine is associated with the highest risk of impaired glycemia. Risperidone and quetiapine are considered “intermediate” risk drugs, and aripiprazole and ziprasidone have the least effect on carbohydrate metabolism [2, 4].
Restrictions
Olanzapine is prescribed with caution in diabetes mellitus. Other atypical antipsychotics, including clozapine, are used without restrictions according to the instructions [3].
Thiazide diuretics
Thiazide (hydrochlorothiazide) and thiazide-like diuretics are widely used to treat arterial hypertension, including in patients with diabetes mellitus. They are prescribed despite the fact that these drugs contribute to the development of hyperglycemia, and in some cases even induce the development of new cases of diabetes mellitus [1].
Hyperglycemia while taking diuretics of this group develops due to the implementation of several mechanisms. First, the drugs cause hypokalemia, which increases transport across beta cell membranes, leading to impaired insulin secretion. Secondly, against the background of their intake, the renin-angiotensin-aldosterone system is activated and, as a result, blood flow in the striated muscles worsens and glucose utilization decreases. This contributes to hyperglycemia and increased insulin resistance [1].
However, there is some good news. Firstly, the effect of drugs of this series on the level of glycemia is dose-dependent, and for the treatment of arterial hypertension they are used in low dosages. And secondly, the thiazide-like diuretic indapamide has virtually no negative effect on glucose metabolism, and its use in diabetes mellitus reduces the likelihood of hyperglycemia to zero [1].
Restrictions
- Hydrochlorothiazide - contraindicated in diabetes mellitus
- Chlorthalidone - contraindicated in severe forms of diabetes mellitus
- Indapamide - used with restrictions for diabetes mellitus in the stage of decompensation. The importance of monitoring blood glucose concentrations in all patients with diabetes, especially in the presence of hypokalemia, is emphasized [3].
Statins
Statins are key drugs used to prevent cardiovascular diseases. Undoubtedly, they are prescribed for diabetes, despite their so-called diabetogenic effect. Research results indicate that statins can cause the development of diabetes. However, the hyperglycemic effect of statins is quite “modest”: for the development of one case of diabetes mellitus, it is necessary to treat 167 patients with rosuvastatin at a dose of 20 mg for 5 years [1].
The negative effect on glucose levels and the possibility of increased glycemia during use are already included in the instructions for the use of statins [1]. Unfortunately, this side effect is characteristic of the entire class of drugs, and there is no difference in the severity of the hyperglycemic effect among its different representatives.
The mechanism of development of the diabetogenic effect of statins is combined. The drugs suppress insulin secretion by reducing the sensitivity of beta cells to glucose and reduce insulin sensitivity in muscles. The diabetogenic effect of statins is dose dependent: the risk of developing diabetes increases with increasing dosages.
It is noteworthy that the likelihood of diabetes when taking lipid-lowering drugs of the statin group is not increased in all consumers. The risk of a hyperglycemic effect is much higher with increased blood glucose levels, increased triglycerides, obesity (BMI ≥30 kg/m2), hypertension and old age. The increased risk of statin-induced diabetes is also associated with a number of other factors, including the female gender of the patient [1].
Despite the proven diabetogenic effect, statins continue to be used in patients with diabetes, since it is obvious that the risk of developing diabetes while taking them is completely offset by the benefit - a significant reduction in the likelihood of developing cardiovascular diseases and complications.
Restrictions
There is no guidance on the use of statins for diabetes, but the instructions emphasize the possibility of developing type 2 diabetes mellitus while taking the drugs [3].
A nicotinic acid
Vitamin PP, or niacin, is involved in many redox reactions, the formation of enzymes, and the metabolism of lipids and carbohydrates in cells. The drug is converted in the body into nicotinamide, which is involved in the metabolism of fats, proteins, amino acids, purines, tissue respiration and biosynthesis processes.
The negative effect on glycemia is expressed in the ability to increase the level of plasma glucose and glycated hemoglobin due to the development of insulin resistance and a decrease in insulin secretion by pancreatic beta cells [1]. For a person suffering from diabetes, this effect can be critical.
Restrictions
If you have diabetes, it is prohibited to take nicotinic acid in high doses. It is also considered inappropriate to prescribe a drug for the correction of dyslipidemia in cases of impaired carbohydrate metabolism. The instructions also note that nicotinic acid can reduce the hypoglycemic effect of glucose-lowering drugs [3].
How to use?
- Thiazide diuretics should be used very carefully . Although this type of diuretic drugs is one of the most gentle in terms of their effects on other systems and organs, they should be taken only as prescribed by a doctor and in the amount indicated in the instructions.
- Before taking medications, you must undergo a full examination to identify diseases in which such medications are contraindicated.
- Depending on the form of hypertension and the general condition of the patient, medications may act differently. In some cases, the effect of the drug begins on the day of administration, while in others it is necessary to take the medicine for more than a week.
- If you feel unwell while taking medications, you should immediately consult a doctor for further advice.
Advantages and disadvantages of the thiazide group of diuretics
Any medication has its own advantages and disadvantages. The clear advantages include a gentle effect on the body. This group is prescribed to patients with problems in the heart, kidneys, liver and other systems. In this case, thiazide derivative drugs are the only possible choice for treatment.
The disadvantages include the not very strong pharmacology of the clinical type, so the patient is often prescribed a long-term regimen of antihypertensive concomitant medications. Loop diuretics could speed up the process in this case, but due to many contraindications, they may not be suitable for a particular person's treatment.
Thiazide overdose and its treatment
Due to increased removal of fluid and salts from the body, the following symptoms may develop:
- rapid pulse,
- drop in blood pressure,
- state of shock
- severe weakness
- fainting,
- dizziness,
- cramps in the calf muscles,
- decreased urination and even anuria,
- numbness of the limbs,
- increased thirst.
For treatment, gastric lavage, forced vomiting and enterosorbents are used if the drug was taken less than half an hour ago. In case of a shock reaction, the introduction of plasma-substituting solutions, sodium and potassium salts is required.