- Characteristics of psychosis
- Who's at risk
- Causes
- Symptoms
- Diagnostics
- Treatment
- Forecast
- Prevention
Attention! Drug use causes irreparable harm to health and poses a danger to life!
Alcohol abuse is one of the main causes of diseases of the central nervous system. Korsakov's alcoholic psychosis is a psychotic condition that develops during prolonged alcohol abuse in the second and third stages of alcoholism. It is one of the types of chronic encephalopathy (organic brain damage).
Characteristics of psychosis
Korsakov's alcohol psychosis was previously known as polyneuritic psychosis, and is a mental disorder in patients suffering from chronic alcoholism, combined with polyneuritis. Characterized by severe memory impairment.
The pathology was first described by psychiatrist Sergei Korsakov in 1887. The doctor described a common disease in patients with alcoholism - damage to the peripheral nervous system, combined with memory impairment and spatio-temporal orientation. In 1897, the disease was recognized internationally and named Korsakoff syndrome.
Who's at risk
The average age of patients admitted with alcoholic psychosis is 50-60 years. It was noted that women predominate among the cases. Also at risk are people who have reached the third stage of addiction, who often take various substitutes for alcohol and low-quality alcoholic drinks.
Diagnosis and treatment of patients with cardiac syndrome X
About the article
17266
0
Regular issues of "RMZh" No. 14 dated June 26, 2009 p. 903
Category: Cardiology
Authors: Lupanov V.P. , Dotsenko Yu.V.
For quotation:
Lupanov V.P., Dotsenko Yu.V. Diagnosis and treatment of patients with cardiac syndrome X. Breast cancer. 2009;14:903.
Epidemiology Approximately 10–20% of patients undergoing diagnostic coronary angiography for acute or chronic cardiac ischemic syndrome have intact coronary arteries. Even if we assume that in some of them the symptoms of ischemia may be due to other cardiac and non-cardiac causes, then at least one out of ten patients with typical angina pectoris does not have hemodynamically significant stenoses of the coronary arteries.
Epidemiology Approximately 10–20% of patients undergoing diagnostic coronary angiography for acute or chronic cardiac ischemic syndrome have intact coronary arteries. Even if we assume that in some of them the symptoms of ischemia may be due to other cardiac and non-cardiac causes, then at least one out of ten patients with typical angina pectoris does not have hemodynamically significant stenoses of the coronary arteries. Definition The presence of typical angina with unchanged coronary arteries was first described by N. Kemp in 1973 [1]. This syndrome is called "syndrome X". Syndrome X is diagnosed in patients with typical chest pain, positive stress tests, angiographically normal epicardial coronary arteries, and no clinical or angiographic evidence of coronary artery spasm. In addition, patients should not have systemic arterial hypertension with or without left ventricular hypertrophy, as well as disturbances in left ventricular systolic function at rest. During exercise, systolic function may be normal or slightly altered. Quite rarely, patients with syndrome X develop blockade of the left bundle branch with the subsequent development of dilated cardiomyopathy. Although most patients with typical chest pain on exercise and a positive stress test usually have overt (obstructive) coronary artery disease, especially when underlying risk factors are identified, approximately 10–20% of them have normal coronary angiograms [2]. These patients are classified as cardiac (cardiac) syndrome X, for which there is no universal definition. In the absence of changes in the coronary arteries during angiography, there is often occlusive pathology of the distal vessels (microvascular angina) [3]. Some authors use the term “microvascular angina,” meaning that patients with typical angina have a normal coronary angiogram and reduced coronary reserve. Syndrome X is usually classified as one of the clinical forms of coronary artery disease, since the concept of “myocardial ischemia” includes all cases of imbalance in oxygen supply and myocardial demand for it, regardless of the reasons causing it. It should be noted that the capabilities of the angiography method in assessing the state of the coronary bed, in particular microvascular, are limited. Therefore, the concept of “angiographically unchanged coronary arteries” is very arbitrary and indicates only the absence of atherosclerotic plaques narrowing the lumen of the vessels in the epicardial coronary arteries. The anatomical features of the small coronary arteries remain “angiographically invisible.” Syndrome X includes various groups of patients, among them, apparently, women in menopause predominate. A significant proportion of patients, especially women who undergo coronary angiography to clarify the cause of chest pain, do not have significant changes in the coronary arteries. In such cases, the characteristics of the pain allow us to consider 3 possibilities: 1) non-anginal pain; 2) atypical angina, including vasospastic; 3) cardiac (cardiac) syndrome X. Positive results of stress tests are observed in 10–20% of individuals with normal coronary arteries and complaints of chest pain [4]. These are usually patients aged 30–45 years, more often women, usually without risk factors for atherosclerosis and with normal left ventricular function. Etiology and pathogenesis The etiology of syndrome X remains unclear. Until now, only some pathophysiological mechanisms have been established that lead to the development of typical clinical and instrumental manifestations of the disease: increased sympathetic activation, endothelial dysfunction, structural changes at the level of microcirculation, metabolic changes (hyperkalemia, hyperinsulinemia, “oxidative stress”, etc.), increased sensitivity to intracardiac pain, chronic inflammation, increased arterial stiffness, etc. There are a number of hypotheses that determine the pathogenesis of syndrome X. According to the first of them, the disease is caused by myocardial ischemia due to functional or anatomical disorders of microcirculation in the intramuscular (intramural) prearterioles and arterioles, i.e. in vessels that cannot be visualized by coronary angiography. The second hypothesis assumes the presence of metabolic disorders leading to disruption of the synthesis of energy substrates in the heart muscle. The third hypothesis suggests that syndrome X occurs with increased sensitivity to painful stimuli (decreased pain threshold at the level of the thalamus) from various organs, including the heart. Despite intensive research over the past 35 years regarding the pathogenesis of coronary syndrome X, many important questions remain unanswered. Among them are the following: 1) whether the chest pain is of cardiac origin; 2) whether pain causes myocardial ischemia; 3) whether other mechanisms (besides ischemia) are involved in the origin of pain; 4) what is the role of myocardial dysfunction and a decrease in the pain threshold in the long-term prognosis of the disease. In recent years, various mechanisms of the formation of IHD have been intensively studied. At the cellular and molecular level, the state of endothelial cells, their metabolism, the role of the receptor apparatus, etc. is assessed. Various interactions between pain threshold and microvascular dysfunction may explain the heterogeneity of the pathogenesis of cardiac syndrome X. Both pain threshold and microvascular dysfunction have gradations in severity and are modulated by various factors such as endothelial dysfunction, inflammation, autonomic neural influences and psychological mechanisms. Among the listed causes, endothelial dysfunction in cardiac syndrome X appears to be the most important and multifactorial, i.e. associated with major risk factors such as smoking, obesity, hypercholesterolemia, as well as inflammation. For example, high plasma levels of C-reactive protein, a marker of inflammation and damage, correlate with the “activity” of the disease and the severity of endothelial dysfunction. Endothelial dysfunction is the earliest link in the development of atherosclerosis, it is determined already in the period preceding the formation of an atherosclerotic plaque, before the clinical manifestations of the disease, and damage to the endothelium, causing an imbalance in the synthesis of vasoconstrictor and vasorelaxant substances, leads to thrombus formation, adhesion of leukocytes and proliferation of smooth muscle cells in arterial wall. Endothelial dysfunction with decreased bioavailability of the endothelium-dependent relaxant factor nitric oxide (NO) and increased levels of endothelin-1 (ET-1) may explain the impaired microcirculation in cardiac syndrome X. In addition, low NO/ET-1 ratios are directly correlated with the severity of pain in these patients. Changes in the structure of blood vessels with impaired endothelial function lead to complications such as myocardial ischemia, heart attack, and stroke. Patients with multiple risk factors often have early coronary atheroma (undetected on coronary angiogram), which can impair endothelial function. Again, it is noteworthy that there is a predominance (approximately 70%) of postmenopausal women in the population of patients with cardiac syndrome X. They often present with atypical chest pain that lasts longer than with typical angina and may be resistant to nitroglycerin. Sometimes these women have mental illness. Estrogen deficiency is a pathognomonic factor that affects blood vessels through endothelium-dependent and endothelium-independent mechanisms. Symptoms Less than 50% of patients with cardiac syndrome X have typical exertional angina, and the majority have atypical chest pain. Despite its atypicality, pain in this syndrome can be very intense and can significantly impair not only the quality of life, but also ability to work. Many patients with cardiac syndrome X experience: a decrease in the internal pain threshold, the occurrence of chest pain during intravenous administration of adenosine, and a tendency to spastic reactions of the smooth muscles of internal organs. Symptoms accompanying cardiac syndrome X resemble vegetative-vascular dystonia. Cardiac syndrome X is often found in people who are suspicious, with a high level of anxiety, against the background of depressive and phobic disorders. Suspicion of these conditions requires consultation with a psychiatrist. Diagnosis Although there is no generally accepted definition of syndrome X, its clinical picture suggests the presence of three signs: 1) typical angina that occurs during exercise (less commonly, angina or shortness of breath at rest), 2) a positive result on an exercise ECG or other stress tests (ST segment depression on ECG, myocardial perfusion defects on scintigrams), 3) normal or non-narrowed (initial changes) coronary arteries on an angiogram. Therefore, syndrome X resembles stable angina. However, clinical manifestations in patients with syndrome X are very variable, and in addition to exertional angina, attacks of resting angina can also be observed. In patients with chest pain and “normal” coronary arteries, arterial hypertension is often identified, with or without ventricular hypertrophy. Hypertensive heart is characterized by endothelial dysfunction, changes in the ultrastructure of the myocardium and coronary bed, and a decrease in coronary reserve. Together or separately, these changes impair coronary blood flow and can cause angina. In such cases, control of arterial hypertension is of primary importance, allowing to restore the functional and structural integrity of the cardiovascular system. Using adequate provocative tests (with acetylcholine, etc.), the clinic tries to exclude spasm of the coronary arteries. In certain situations, for example, in the presence of a widespread perfusion defect or a focus of asynergy of the left ventricular wall and angiographically unchanged artery, intracoronary echocardiography (intravascular ultrasound) may be performed to exclude obstructive changes in the vessel. Table 1 shows the recommendations of the ESC (2006) for the examination of patients with the classic triad of syndrome X. Thus, cardiac syndrome X is diagnosed by exclusion. First of all, coronary atherosclerosis and other diseases of the coronary arteries are excluded. You should carefully collect an anamnesis with an analysis of concomitant symptoms and risk factors for cardiovascular diseases, the results of non-invasive stress tests, and also carry out a differential diagnosis with diseases and dysfunction of other organs (esophagus, spine, lungs and pleura, abdominal organs), certain diseases and valvular cardiac anomalies - vasospastic angina, mitral valve prolapse. It is necessary to differentiate cardiac syndrome X from cardialgia associated with impaired motility of the esophagus, fibromyalgia and osteochondrosis. Some cardiologists believe that in addition to chest pain typical of angina and ischemic ECG changes (horizontal or downsloping ST segment depression of 1 mm or more) or other evidence of heart damage (for example, detection of a transient defect in myocardial perfusion on thallium scintigraphy - 201), the subepicardial coronary arteries should be angiographically completely unchanged. However, even these strict angiographic criteria have their limitations, since it is known that coronary angiography may be uninformative (since it does not detect early atherosclerotic changes within the arterial wall, is not sensitive enough in diagnosing intracoronary thrombosis, does not help determine the internal structure of plaques and identify plaques prone to rupture and ulceration). At the same time, the stress ECG test in some patients with syndrome X may be uninformative due to its premature termination at low load due to fatigue, shortness of breath or chest discomfort. In these cases, a transesophageal electrical stimulation test or an intravenous dobutamine test can be used to detect myocardial ischemia. In cardiac syndrome X, transient perfusion defects have been shown to occur in areas supplied by poorly affected arteries. Single-photon emission computed tomoscintigraphy of the myocardium, along with the assessment of myocardial perfusion, allows one to determine the parameters of left ventricular contraction [5,6]. In some patients, local disturbances in the mobility of the heart wall are detected during stress echocardiography, magnetic resonance imaging, or disturbances in myocardial metabolism are determined during positron emission tomography. Intravascular ultrasound examination of the coronary arteries is of greatest importance precisely in cases where coronary angiography reveals normal or slightly altered coronary arteries. It allows you to study the surface and internal structure of atherosclerotic plaques, verify plaques of complex configuration, give them a quantitative assessment, examine the condition of the vascular wall around the plaque, and identify coronary artery thrombosis. However, the complexity of the technique, its high cost, and the need for highly qualified personnel prevent the widespread use of this valuable method. Table 2 shows the characteristic signs and examination plan of a patient with cardiac syndrome X. Differential diagnosis The group of patients with cardiac syndrome X is heterogeneous. Some experts include patients with systemic arterial hypertension, hypertrophic cardiomyopathy, or idiopathic dilated cardiomyopathy. However, most of them believe that patients with muscle bridges, arterial hypertension, pulmonary hypertension, valvular heart disease, mitral valve prolapse, left ventricular hypertrophy and diabetes mellitus should be excluded from coronary syndrome X, since in these cases it is assumed that the causes for the appearance angina pectoris are known. When diagnosing the disease in question, the following should also be excluded: patients with spasm of the coronary arteries (vasospastic angina), patients in whom non-cardiac causes of chest pain have been documented by objective methods (for example, musculoskeletal - osteochondrosis of the cervical spine, etc.; neuropsychic – anxiety-depressive syndrome, etc.; gastrointestinal – esophageal spasm, gastroesophageal reflux, gastric or duodenal ulcer, etc.). In addition to cardiac syndrome X (microvascular angina), there is also metabolic syndrome X. This “multi-metabolic syndrome” describes a combination of certain clinical signs and risk factors for CAD: abdominal obesity (waist/hip index >0.85), hypertension, impaired carbohydrate tolerance or type 2 diabetes mellitus, dyslipidemia (hypertriglyceridemia and decreased high-density lipoprotein levels). The unifying factors for all these clinical conditions in metabolic syndrome X are hypertriglyceridemia and tissue resistance to insulin [7]. Other characteristics of these patients include hyperuricemia, physical inactivity, and premature aging. However, both described syndromes X can be combined in one patient. Drug treatment Insufficient attention of cardiologists to the pathology in question does not lead to the disappearance of the problem. Treatment for the group of patients with syndrome X remains not fully developed, so the right drug strategy can improve the quality of life of patients and reduce the financial costs of healthcare. Various approaches to drug treatment are used (antianginal drugs, ACE inhibitors, angiotensin II receptor antagonists, statins, psychotropic drugs, etc.). The choice of treatment is often difficult for both treating physicians and the patients themselves. The success of treatment usually depends on the identification of the pathological mechanism of the disease and is ultimately determined by the participation of the patient himself. An integrated approach to the treatment of patients with cardiac syndrome X is often necessary. General advice on changing the quality of life and treating risk factors, especially aggressive lipid-lowering therapy with statins (reducing total cholesterol to 4.5 mmol/l, LDL cholesterol to less than 2.5 mmol/l ), should be considered as vital components of any chosen treatment strategy. Antianginal drugs such as calcium channel blockers (nifedipine, diltiazem, verapamil, amlodipine) and
Causes
The development of Korsakoff's psychosis is possible against the background of severe delirium and Gaye-Wernicke syndrome. The disease develops after a series of encephalopathies in patients with alcoholism. But in practice, there have been cases of gradual manifestation of symptoms with systematic intake of alcoholic beverages and progressive alcohol degradation. Rarely does the disease develop in conditions of a relatively favorable emotional state without previous signs of mental disorders.
The main factors causing the development of Korsakov’s alcoholic psychosis:
- acute lack of thiamine (vitamin B1);
- destruction of liver cells, toxic hepatitis, cirrhosis;
- damage to the intestinal mucosa.
Regular intake of alcohol stimulates the work of the small intestine, where the absorption of elements required for the normal functioning of the body occurs. The absorption of vitamins is impaired, which leads to the slow destruction of the limbic structures of the brain.
Vitamin B1 deficiency increases the risk of encephalopathy and delirium. If a patient in this condition does not receive medical care, in 80% of cases Korsakov alcoholic psychosis begins.
Neurological diseases contributing to the development of the syndrome:
- heart attacks and brain cancer;
- encephalitis of any pathogenesis;
- serious head injuries;
- degenerative dementias;
- surgical operations in the treatment of epilepsy.
Get help now
Do any of your relatives or friends have an addiction? Have you tried in every possible way to help, but as a result the person still returned to his past life?
You are not the first to encounter this problem, and we can help you.
We guarantee anonymity, we will persuade you to undergo treatment, and we will help you choose a center.
Call us
+7
or
Call me
Wernicke-Korsakoff syndrome
Wernicke-Korsakoff syndrome (WKS) is a disease that includes acute and chronic stages of a neurodegenerative process that occurs as a result of thiamine deficiency and usually develops in individuals with severe forms of alcoholism. “As a rule,” because it is extremely rare that this condition develops outside of alcohol consumption. The acute stage of the process is called Gaye-Wernicke encephalopathy, the chronic, residual stage is called Korsakoff psychosis, or Korsakoff syndrome [2].
The classic manifestation of acute Wernicke encephalopathy is a tetrad of symptoms: ophthalmoplegia, ataxia, nystagmus, confusion [2]. It should be noted that a complete tetrad is found in only 20% of cases, which is associated with difficulties in diagnosing this condition. With incomplete recovery, the acute stage of encephalopathy gives way to the chronic stage, and irreversible changes in the brain structures responsible for the process of memory consolidation are observed [1, 2]. Thus, the patient has difficulty remembering information that has just entered the brain (fixation amnesia), while relative preservation of other mental functions is observed [1, 2].
When analyzing this syndrome, it is worth considering Wernicke encephalopathy and Korsakoff psychosis separately.
Wernicke encephalopathy (WE) is an acute brain disorder that manifests itself with severe neurological and mental disorders, ending in death in half of the cases. This pathology was first described by Karl Wernicke in 1881 as “acute superior hemorrhagic polioencephalitis” (“polyoencephalitis haemorrhagica superior acuta”) [2,3].
The pathogenesis is based on the development of neurodegenerative changes as a result of vitamin B1 deficiency [2]. The underlying causes may be both malnutrition and insufficient absorption, but ultimately there is a violation of the conversion of thiamine to thiamine pyrophosphate (TPP), which is the active part of TPP-dependent enzymes, such as: alpha-ketoglutarate dehydrogenase, transketolase, pyruvate dehydrogenase [4,2 ]. These enzymes catalyze biochemical reactions that ensure normal metabolism of nervous tissue. Thiamine's ability to overcome the blood-brain barrier is impaired, cellular transport is disrupted, which leads to a lack of vitamin B1 in the brain, which in turn leads to a decrease in the activity of TPP-dependent enzymes, which lead to lactic acidosis, followed by a violation of mitochondrial functions, as a consequence of inhibition tissue respiration, which in turn reduces the energy supply of neurons and neuroglia. Most often, the mediodorsal nuclei of the thalamus, hypothalamus, mamillary bodies and tegmentum of the midbrain are involved in the process, with characteristic intravital symptoms. Death most often occurs as a result of cerebral hemorrhage [2, 3].
Wernicke's encephalopathy is characterized by the following tetrad: ophthalmoplegia, nystagmus, ataxia, confusion. Although sometimes swelling of the optic discs and hemorrhages in the retina are also observed. With EV, body temperature decreases, tachycardia occurs, and weakness increases. One of the indicators of the patient's condition is the degree of impairment of consciousness. In some cases, EV follows a short period of severe alcoholic delirium, in this case there is a gradual decrease in the intensity of psychomotor agitation and an increase in detachment, the transition of delirium into a murmuring (mumbling) form or amentia-like agitation limited to the bed. As the condition further deteriorates, the level of consciousness begins to decline with the formation of stupor and coma. Patients usually have reduced body weight and sometimes suffer from dehydration [4, 5]. .
Figure 1 | The role of thiamine in glucose metabolism
Korsakov psychosis
The difference in pathogenesis between Korsakoff's psychosis and Wernicke's encephalopathy lies in the degree of reversibility of the changes. Thus, in the first case, the changes are irreversible, while in the second case, the changes are characterized by biochemical changes, which theoretically implies the possibility of adjustment with timely treatment with loading doses of thiamine. In Korsakoff's syndrome, the conduction of the mamillary-thalamic tracts is disrupted, resulting in impaired memory consolidation. The mamillary bodies and nuclei of the thalamus are damaged [2].
The leading symptom is amnesia, primarily fixation, which determines a special type of disorientation in such patients. Deprived of the ability to record new information, a patient with Korsakov's psychosis is unable to remember the current date, the place in which he is, and the location of the rooms, the name of his roommate or the attending physician, but he can often recognize by indirect signs that he is in the hospital, and window - spring. Fixation amnesia is also accompanied by (antero)retrograde amnesia, which, however, does not determine the severity of the patient’s condition. Occasionally, amnesia is accompanied by confabulations - false memories with which the patient fills in gaps in his memory. It should also be noted that patients develop lower flaccid paraparesis and paraplegia as a result of polyneuropathy.
It is important to mention the description of Korsakov’s psychosis, compiled by S. S. Korsakov himself: “From one patient I had to hear almost constantly the following: “I lay down today, I’ll get up now - only this very minute my legs somehow cramped - as soon as they disperse, I I’ll get up.” He had a long-term contracture in his knees, but, not remembering its existence, he believed that this was only a matter of the moment. This same patient categorically claimed that he had no pain in his legs, but meanwhile he had very strong shooting pains: when he shot, he would scream, and then immediately answer the question that he had absolutely no pain. ... The same patient, reading a newspaper, could read the same line ten times in a row as something completely new; it happened that by chance his eyes would stop on something interesting, and he would read this line out loud to his mother and laugh; but at this time, of course, he will take his eyes off the place he was reading for a few seconds, and then, when his eyes again fall on this place, at least right away, he again with the same words: “listen, mom” - reads this passage, and thus can be repeated many times...” [2].
Diagnosis of the disease is based on MRI results, clinical picture, medical history and laboratory diagnostic data. .
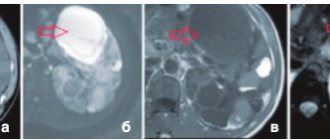
Figure 2 | MRI of the brain
1 - hyperintense signal not only from the periaqueductal gray matter and mammillary bodies, but also from the white matter of the midbrain. 2, 3 - hyperintense signal from individual areas of the gray matter of the cerebral cortex. 4 - area of central demyelination in the region of the midbrain and the upper part of the pons. 5 - accumulation of contrast in the meninges and individual areas of the cortex [4].
Thus, an MRI of the brain can reveal damage to certain areas of the gray matter; in this case, the gray matter of the midbrain tegmentum is affected. Almost always, with Wernicke-Korsakoff syndrome, damage to the mamillary bodies is detected, this image is no exception. The image also shows lesions in the hippocampus and hypothalamus with subtle enhancement in these areas, also characteristic of CRS.
Treatment of acute Wernicke encephalopathy consists of immediate administration of large doses of thiamine (vitamin B1) within 48–72 hours from the onset of neurological symptoms [1,2].
Intravenous administration of thiamine is recommended, since taking tablet forms does not allow creating a high concentration of the active substance in the blood in a short time, ensuring penetration through the blood-brain barrier and entering the brain in sufficient quantities [3,2].
The treatment regimen includes intravenous administration of thiamine from 200 to 500 mg 3 times a day for 7 days. From day 8, intravenous administration of thiamine is replaced by oral administration, reducing the dose to 200 mg per day for 2 weeks, then 100 mg per day for another 2 weeks [2].
The recommended duration of thiamine administration for Wernicke encephalopathy is 2–3 months, and for Korsakoff psychosis it reaches 2 years [2].
Often this disease is accompanied by polyneuropathy. Treatment includes alpha lipoic acid (ALA; syn. thioctic acid). ALA is close in biochemical activity to vitamin B. One of the biological effects is the interaction with TPP-dependent enzymes, including pyruvate dehydrogenase, which catalyzes biochemical reactions in the central and peripheral nerve formations. ALA also has an antioxidant effect, suppressing oxidative reactions in mitochondria, thereby preventing their damage and, as a result, inhibition of energy processes. It is worth mentioning that the substance interacts with vitamins C and E, thereby stimulating their ability to neutralize free radicals (FR) [3,2].
When treating patients with Wernicke's encephalopathy, it is necessary to avoid dehydration and electrolyte deficiency, in particular potassium and magnesium. Correction of water and electrolyte balance is carried out using infusion of plasma-substituting solutions. Also, during the treatment of CRS, it is necessary to avoid administering large doses of glucose to patients with chronic alcoholism and delirium delirium, as this increases vitamin B1 deficiency, as a result, increasing the risk of developing encephalopathy or worsening its course [2].
Sources:
- Latt N, Dore G. Thiamine in the treatment of Wernicke encephalopathy in patients with alcohol use disorders. J Intern Med. 2014;44(9):911-5.
- I.V. Damulin Wernicke-Korsakoff syndrome / I.V. Damulin, S.Yu Petrovich // Clinical medicine. Review of literature on neurology, neuropsychology. — 2014 — P.76-80
- Meier S, Daeppen JB. Prevalence, prophylaxis and treatment of Wernicke encephalopathy. Thiamine, how much and how do we give it? Rev Med Suisse. 2005;1(26):1740-4.
- S. V. Kotov Wernicke-Korsakoff syndrome / A. I. Lobakov, S. V. Kotov, E. V. Isakova G. A. Stashuk T. V. Volchenkova // Journal of Neurology and Psychiatry named after. S.S. Korsakov. — 2021 116(7), — P.4-11
- Schabelman E, Kuo D. Glucose before thiamine for Wernicke encephalopathy: a literature review. J Emerg Med. 2012;42(4):488-494.
Symptoms
The first signs of Korsakov's psychosis may appear in advance, before the onset of the underlying disease (about 2 years), among them:
- body aches;
- pain in the limbs;
- unsteady gait the next day after drinking alcohol;
- sleep problems - insomnia, nightmares;
- increased anxiety;
- fears for no apparent reason.
The disease is characterized by the following clinical manifestations:
- Fixation amnesia. The patient is unable to remember and store new information, events from the recent past and present. At the same time, memories from youth and even childhood are preserved. A mental disorder sometimes manifests itself with such intensity that a person loses the ability to learn, reacts inadequately to household changes, new people in the environment, or moving.
- Retrograde amnesia. The memory of events that preceded the disease or the onset of attacks is lost.
- Amnestic disorientation. The patient is not oriented in space and time, and loses the ability to perform life skills. Loses criticality towards one's own condition. Doesn't understand where he is, seems helpless.
- Confabulation is one of the early signs of the syndrome. The patient creates confused or imaginary versions of events that he cannot remember. Often such stories “pop up” when questioning patients, and not spontaneously. In terms of content, they may include facts from everyday life that sound plausible. Less often, the patient talks about imaginary adventures and incidents, fantastic events.
- Neurological signs - neuritis, accompanied by paresis, more or less pronounced atrophy of the muscles of the limbs, decreased sensitivity, weakness, paralysis. Sometimes tendon reflexes disappear.
General behavioral changes:
- passivity;
- lethargy;
- excessive fatigue;
- dysphoria;
- there is practically no facial expression;
- slow motor skills;
- apathy followed by fussiness;
- irritability;
- defects in visual fields, impaired pupil movement;
- anxiety;
- hypochondriacal disorder;
- decrease in intellectual abilities.
Severe psychosis leads to dementia. If the disease is malignant, there is a risk of death due to brain pathologies.
Clinical picture
From the manifestations of K. s. Memory disorders for current events are especially pronounced: patients almost instantly forget the content of what they just said, after a few minutes they do not remember who approached them, which is why they can say hello to the same people many times, ask the same questions questions; they cannot say what they just did or what they ate; They read the same page in a book for weeks, immediately forgetting what they read. Verbal memory is most severely impaired, figurative memory is to a lesser extent, and the so-called memory suffers even less. emotional memory, in connection with which, completely not remembering the content of an unpleasant event, the patient may get into a bad mood in the environment where it happened, or at the sight of a person related to him.
Despite a pronounced memory disorder for current events, memory for past life events, often distant, remains with K. s. relatively intact, and some memories of ancient events are particularly vivid. However, the events immediately preceding the disease, often spanning weeks, months and even years, can completely disappear from the patient’s memory, which allows us to talk about the presence of c. retrograde amnesia (see) of varying duration.
Characteristic for K. s. Disorders of orientation in time, place and environment are expressed to varying degrees. Time orientation is most severely impaired, and patients often cannot name not only the date, day of the week, month and year, but also the time of year. Orientation in a place is also inaccurate in most cases. Patients with more severe disorders cannot even navigate their surroundings: they cannot find their bed, cannot find their way to the dining room, toilet, etc.
False memories in K. s. There are two types. More typical are the replacement of memory gaps for current events with memories of real events that occurred in the past. Thus, patients who have been in hospital for a long time say that they recently “came from work”, “were visiting relatives”, etc. This type of false memories is called pseudo-reminiscence. Less often, when asked about their current life, patients report fictitious stories, often of fantastic content (“traveled to the countries of Africa and Asia, met the Abyssinian Negus,” “flew on a spaceship,” etc.). Such memory deceptions are called confabulations (see Confabulosis). Patients with K. s. suggestible. Asking questions can trigger one type of false memory or another.
An influx of abundant confabulations with deep disorientation and incoherent thinking in the absence of clouding of consciousness is called confabulatory confusion. The latter is mainly observed with K. s. in patients with a variant of senile dementia, designated as hron, Wernicke's presbyophrenia (see Senile dementia).
In some patients with K. s. Sometimes phenomena of false recognition are observed when they mistake others for people they have met before.
Patients with K. s. in most cases, one or another degree of intellectual deficiency is characteristic, which is expressed in a weakening of the productivity of thinking, stereotypicality and monotony of judgments, their pronounced dependence on external impressions, the inability to notice contradictions in one’s own statements, and to detect the incompatibility of false memories with reality. At the same time, some patients are distinguished by a certain intelligence and, within a specific situation, sometimes skillfully mask memory defects.
In most patients with K. s. there is a more or less pronounced decrease in the level of impulses and volitional activity, and therefore, left to their own devices, they can remain inactive for hours. More often these are elderly people. They have a predominant apathetic or apathetic-euphoric mood background. Young people are usually more active.
As a rule, patients' consciousness is not clouded. At the same time, a combination of K. with. with states of clouded consciousness, more often with symptoms of delirium (see Delirious syndrome), accompanied by motor restlessness and occurring mainly at night.
K. s. may have a number of age-related characteristics. Thus, in children, false memories are usually absent or weakly expressed. In old age, orientation disorders are especially intense (amnestic disorientation), and orientation in the immediate environment is often disturbed, false memories manifest themselves in the form of replacement of memory gaps with events of the distant past (ecmnestic confabulations), and false recognitions are frequent.
As a rule, K. s. is a relatively persistent, chronic condition. However, cases of transient C. are possible, for example, with traumatic brain injuries, delirium tremens, carbon monoxide poisoning, and postoperative psychoses. Transient K. s. is one of the transitional Vick syndromes.
Current of K. s. depends mainly on the nature of the underlying disease. So, alcoholic K. s. occurs acutely, immediately after the patient emerges from a state of darkened consciousness, and then a long-term (from 2 to 15 years) stationary course is possible, followed by a slow reverse development, which ends in an outcome in a personality defect in the form of intellectual failure, memory weakness, decreased activity and apathetic or apathetic-euphoric mood.
K. s. with severe brain hypoxia (carbon monoxide poisoning, self-hanging) develops acutely, following a period of darkened consciousness; the stationary period is relatively shorter (from several weeks to 2-3 years), followed by a regressive course. Sometimes the illness ends in complete recovery. However, a more typical outcome is a personality defect with intellectual-mnestic deficiency.
K. s. with traumatic brain injuries, it also begins acutely, after a period of darkened consciousness. Its further course is regressive, although the outcome of complete recovery is rarely observed. The development of a persistent mental defect is more often noted.
For vascular diseases of the brain (cerebral atherosclerosis, hypertension) K. s. develops gradually, has a more or less long stationary period, which is replaced by a progressive course, characterized by progressive amnesia and deepening intellectual disability. K. s. for senile dementia, Ch. arr. hron, presbyophrenia, develops gradually, and then there is a progressive increase in memory disorders and a gradual general disintegration of personality.
T. o., K. s. can have a stationary, regressive and progressive course.
Diagnostics
In making a diagnosis, it is important to talk with relatives who will give truthful information about the patient’s behavior, the duration of alcohol dependence, and the presence of previous signs.
Diagnosis of Korsakov polyneuritic alcoholic psychosis involves the following measures:
- Consultation with a psychiatrist and psychologist. Specialists determine the nature of memory loss, disorientation due to amnesia, the presence of accompanying delusional ideas, and confabulation. During the examination, to identify memory problems, the doctor conducts word recall tests and other types of psychological testing for rote and conscious memorization.
- Consultation with a neurologist. The symptoms of polyneuritis are determined. The doctor examines the condition of the limbs to identify muscle atrophy, paresis, and disorders of the musculoskeletal system. Also pays attention to the function of the eye muscles.
- Laboratory research. The patient donates venous blood for biochemical analysis. First of all, it is important to identify vitamin B1 deficiency and the general condition of systems and organs.
- Hardware diagnostics. MRI of the brain, computed tomography of the liver and other organs are performed.
When diagnosing, it is important to differentiate Korsakov's psychosis from other diseases, such as atherosclerosis, dementia, delirium, progressive paralysis, dissociative amnesia, memory impairment due to depression.
The main difference between Korsakov's psychosis and dementia is that the patient is conscious, able to think and answer questions clearly, only memory is impaired.
Treatment
After the diagnosis is made, the rehabilitation center prescribes complex therapy aimed at detoxification and restoration of the vital functions of the body. Acute psychosis can only be treated in an inpatient setting.
Therapy is carried out as follows:
- Detoxification: infusion therapy - droppers with saline and glucose.
- Vitamin therapy - a high dose of thiamine is administered (followed by a gradual reduction in dosage). This is an effective way to treat neuritis and any neurotic disorders.
- Drug therapy aimed at restoring cognitive functions, improving memory and concentration of the patient. For this purpose, nootropics (Phesam, Noopept) are introduced. For increased anxiety, antipsychotics (clozapine, pipothiazine) are administered in small doses.
- General condition monitoring. Prescribed for severe disorientation, passivity, and severe amnesia. Medical personnel monitor the daily routine, compliance with hygiene rules, and physical recovery.
- If the patient is bedridden, separate care is required to prevent bedsores and hypoventilation.
- Physiotherapeutic methods. This includes gymnastic exercises, hardware techniques that prevent complications and complete muscle atrophy.
One of the promising means of treating acute alcohol disorders and alcoholism itself is memantine - akatinol. According to research results, the drug improves the cognitive functions of patients suffering from Korsakoff's psychosis, and at the same time demonstrates a chance to reduce the severity of alcohol dependence.
Forecast
Treatment of alcoholic psychosis is characterized by relative effectiveness - the success of the procedures depends on the age category, general physical and mental condition, experience of alcoholism, and ability to adapt.
Memory defects with correct long-term treatment may disappear, but they may remain incurable and even worsen over time.
In general, if prescribed therapy is followed, the prognosis will be favorable. But some problems with thinking and psyche may persist. There is a risk of an unfavorable prognosis if medical assistance is not provided on time. In this case, the disease becomes malignant with a fatal outcome.