Hemorrhagic stroke is a cerebral hemorrhage that has consequences of varying severity and duration. This pathology poses a serious threat to human life. After a long crisis, irreversible brain damage occurs. Regardless of the course of the disease and the severity of the consequences, long-term recovery is required. It is better to carry out rehabilitation after a hemorrhagic stroke in a department or special rehabilitation centers. They employ doctors of the highest category who control the speed and quality of the patient’s return to a normal lifestyle and adaptation to new conditions.
Mechanism of occurrence and types of hemorrhagic stroke
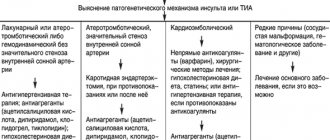
A stroke is an acute cessation of blood supply to tissues. This condition leads to necrosis of nerve cells, which are slowly restored and cannot perform their usual functions. The most common type is ischemic stroke - neurons are deprived of oxygen due to blockage of arteries and other vascular pathologies. Hemorrhagic stroke is more life-threatening and is associated with vascular rupture and subsequent hemorrhage. Its severity depends on the location of the damaged area, the caliber of the vessel and other factors, including the age of the patient.
Hemorrhagic strokes are usually classified according to the place of their occurrence. So, there are several main varieties:
- parenchymal - occurs directly in nerve tissues;
- intraventricular - hemorrhage into the cavity of the ventricles of the brain;
- subdural - blood enters under the dura mater of the brain;
- epidural - the focus is localized above the hard shell;
- subarachnoid - hemorrhage between the arachnoid and pia mater of the brain.
When blood enters nerve tissue or the cavity of the brain, hematomas of various sizes are formed. Their appearance causes tissue swelling, which puts pressure on neurons. If there is no blood supply, they die. As a result of necrosis of nerve cells, there is a loss of vital skills, a sharp deterioration in health, and the risk of developing coma remains. In addition, the acute period is dangerous and fatal, and during the rehabilitation process a recurrence of stroke is possible.
Recovery after a stroke at home
When a person is strong enough after a stroke, recovery measures can be taken even at home with the support of loved ones. However, all this must be in accordance with the prescriptions of doctors and under their supervision. Only in this case can you expect an effective result. It is important to start a rehabilitation program immediately after discharge from the hospital, and not to miss the first year after a stroke attack, when proper therapy helps you recover the fastest.
Recovery at home is a huge responsibility for the relatives of a person who has suffered a stroke. It is important to prepare comfortable conditions for him, restore order, ensure the prevention of bedsores and proper nutrition, and monitor the intake of medications. An organized daily routine and comfort in the home improve your mood and well-being, making it possible to recover faster.
Possible causes of the attack
Hemorrhagic stroke has an acute onset. It is difficult to determine its cause, especially in the absence of a history of heart and vascular diseases. Up to 15% of cases remain unrecognized, and in a quarter of patients, hemorrhage begins without a clear cause. During the diagnosis, a rupture of the vessel is noted, and the provoking factor remains the goal of further examinations. This is necessary to prevent further relapses. In general, there are several conditions that can provoke a hemorrhagic stroke:
- chronic increase in blood pressure;
- diabetes;
- lipid metabolism disorders;
- heart and vascular diseases, including atrial fibrillation, stenosis (narrowing) of the carotid arteries, anemia;
- unhealthy lifestyle, bad habits, excess weight.
Arterial hypertension is the most common cause of hemorrhagic stroke. With a chronic increase in pressure, the strength and elasticity of the vascular walls decrease and the properties of the blood change. Patients of the Clinical Brain Institute often complain of pressure surges, but have no idea what consequences this condition can lead to. Rapid blood filling of the vessels causes their rupture with subsequent hemorrhage into the brain tissue.
Metabolic disorders also affect the condition of the vascular walls. One of the most common forms of dyslipidemia (pathologies of fat metabolism) is the accumulation of excess cholesterol. It forms deposits on the walls of the arteries, causing them to become brittle and unable to withstand stress. This condition provokes the development of atherosclerosis, a disease that is accompanied by a decrease in the elasticity of the arteries. This disease is often diagnosed as a precursor to hemorrhagic stroke.
Another pathology that can lead to spontaneous hemorrhages is diabetes mellitus. Frequent fluctuations in blood glucose levels irritate the inner lining of the walls of blood vessels, which causes their fragility. Additional factors, including surges in blood pressure, cause rupture of arteries in any area. If the process is localized in the brain area, it is dangerous with serious complications.
The lifestyle and age of the patient also affect the condition of blood vessels and the chemical composition of the blood. Only with regular physical activity is normal blood circulation possible. Sedentary work, poor diet, alcohol abuse and smoking are the main causes of increased blood viscosity, blood clots, atherosclerosis and other vascular diseases. In such conditions, strokes can occur for no apparent reason, with a slight increase in pressure.
Rules for caring for victims after a stroke
The rehabilitation program should begin as soon as the person’s condition becomes stable, the sooner the more effective. In this matter, an individual approach is very important. Rehabilitation specialists carefully study the history and clinical picture of the pathology, analyze existing disorders, the location and extent of brain damage, and the patient’s general well-being.
In addition, a proper rehabilitation program is based on the following principles:
- systematic;
- duration;
- subsequence;
- involvement of the sick person and his relatives;
- complexity;
- adequacy
You need to work with a person after a stroke every day. With a methodical and competent approach, the desired effect of therapy is possible.
Preparing the room and bed
The environment in the room where a person is recovering from a stroke should be comfortable. You need a spacious room with good lighting and sound insulation. Furniture must be stable enough so that a person can safely lean on it if necessary.
At first, when a stroke victim cannot move on his own, it is advisable to provide a bed with an anti-bedsore mattress. Functional beds are especially convenient, in which you can adjust the height of the headboard. Small sides that protect against falls are also useful.
A person after a stroke cannot be in one position all the time, as the back and limbs begin to tense, this causes pain. To relieve stress, you can use pillows. For example, if your leg hurts, you can put it on a pillow and bend your knee slightly. This will reduce the load at certain points and the body will relax.
Bed linen must be changed regularly. Pillowcases, duvet covers, sheets - everything should be fresh and pleasant. And next to the bed you need to provide a table or bedside table where you can put water and the things a person needs (books, glasses, phone). All objects should be close enough so that you do not have to bend or climb for them.
A toilet chair must be placed near the bed. The device should be positioned so that a person can sit on it himself if necessary.
Prevention of bedsores
In the first time after a stroke, a person lies down almost all the time, so it is necessary to prevent bedsores. These skin and tissue damage usually appear as redness, abrasions, and blisters. Bedsores most often appear in the area of the back of the head, sacrum, and shoulder blades. To prevent their occurrence, you need to use an anti-bedsore mattress, as well as regularly change the body position of the sick person. It is also important to keep your skin clean and make sure it is not overly wet or dry. The sheet should also be clean: without folds, crumbs, lumps, etc. When changing bedding, do not pull it out from under the person lying down; try to carefully remove it piece by piece.
If bedsores cannot be avoided, you should consult with a healthcare professional on how to properly get rid of them. The damaged areas should be treated with medicinal ointments.
Nutrition
The key to a quick recovery is tasty and healthy food. But being overweight is also dangerous, so it is important not to overeat. For recovery after a stroke, split meals in four to five meals in small portions are better suited.
Try to keep your food to a minimum of salt (up to 5 g) and vegetable oil. Boiled or baked dishes are recommended. The menu can include:
- black bread, bran;
- cereals;
- fruits, vegetables and herbs;
- soups;
- low-fat dairy products;
- eggs;
- red and river fish;
- chicken meat without skin;
- juices, mineral water, green tea,.
Fatty and sweet foods should be limited as much as possible. It is better to cook as few dishes as possible with potatoes, especially fried ones. Caviar, fatty sausages, jam, baked goods, chocolate, and sweets are contraindicated. Honey or dried fruits are suitable as dessert.
In some cases, people have trouble swallowing after a stroke. Until this function is restored, a person needs to prepare the softest food possible, but not liquids. At the same time, it is important to be with the patient while eating and help if necessary.
An example of a healthy menu for a person recovering from a cerebrovascular accident:
| Eating | Example menu |
| Breakfast | Two boiled eggs or rice porridge, green tea |
| Lunch | Low-fat cottage cheese, baked apple or dried fruit compote |
| Dinner | Vegetable or bean soup, beef stroganoff with buckwheat porridge, tea with milk |
| Dinner | Salmon fillet with fresh vegetable salad, apple compote |
| Second dinner | A glass of low-fat kefir or some dried fruits |
Motor rehabilitation
This is one of the most important areas of rehabilitation therapy, since a person’s ability to return to self-care and normal lifestyle largely depends on it. Patients after a stroke:
- do ergotherapy and kinesiotherapy;
- learn to move independently;
- restore self-care skills;
- are being treated for arthropathy;
- overcome muscle spasticity (taking muscle relaxants, physiotherapy, auto-training, prevention of bedsores, acupuncture);
- attend massage sessions.
Gradually, a person restores everyday habits, skills in handling household appliances, the ability to move around and take care of himself independently. But all this happens gradually. First, a person learns to roll over on his own, then sit down, stand, and gradually tries to walk and climb stairs. It is important not to push it and to systematically go through all these stages. You need to relearn how to move at your own pace, consolidate these skills and enjoy your achievements.
All methods are selected taking into account the patient’s well-being, since some of them are very tiring for a weakened person, for example, kinesiotherapy or physiotherapy. Prescriptions are made taking into account contraindications to motor rehabilitation, including second and third degree heart failure, chronic pulmonary diseases, malignant tumors, frequent attacks of bronchial asthma, and psychosis. The possibility of carrying out certain activities is limited by the presence of severe arthritis, arthrosis, and pelvic disorders in the patient.
Restoration of cognitive functions
Neurologists, neuropsychologists, and occupational therapists help the patient recover. It is important that after a stroke the person himself does not lose faith in his own strength and desire to exercise. The patient must perform exercises to develop thinking, attention, and memory. If doctors deem it necessary, they prescribe medications to stimulate nervous activity.
Return of speech
This direction of the rehabilitation program determines whether the patient can return to normal communication with others. To do this, individual and group sessions with a speech therapist are prescribed, and special techniques are used that help develop the muscles of the larynx.
Speech disorders are also often accompanied by impairments in the ability to write, count and read. In this case, psychological correctional classes are prescribed.
With a proper rehabilitation program, speech functions are restored mainly in the first three to six months. However, recovery in general can last up to two to three years.
Psychological support
This part of the rehabilitation program includes classes with a psychologist or psychotherapist, pleasant physical activity (walking, light exercises, etc.), communication with loved ones. If necessary, doctors may prescribe antidepressants.
Clinical picture
At the first symptoms of a hemorrhagic stroke, it is important to begin treatment immediately. This is an acute condition that does not go away without symptoms. In most cases, the patient experiences a sharp deterioration in health, and loss of consciousness may occur.
The first symptoms of hemorrhagic stroke
The first manifestations of a stroke may differ, depending on the volume of the hematoma and its location. The task of loved ones is to identify them at an early stage and call a medical team for urgent hospitalization of the patient. Experts from the Clinical Brain Institute advise you to familiarize yourself with the main symptoms that may indicate acute cerebrovascular accident:
- tingling sensation of the skin, numbness of part of the face;
- nausea and vomiting;
- headaches, as well as soreness in the eye area and behind the eyes;
- impaired motor coordination;
- rapid pulse;
- paresis and paralysis of muscles in any part of the body, most often the process is one-sided.
These symptoms are typical if the patient remains conscious. Fainting is a common sign of a hemorrhagic stroke, and it is strictly forbidden to try to revive the person. There are several phases of consciousness regression - the prognosis for each of them will also be different:
- stunning - minor changes in which the victim is poorly aware of what is happening and practically does not react to others;
- somnolence - lack of response to external factors, while the eyes remain open, breathing and heartbeat are normal;
- stupor - a condition that resembles sleep, with preservation of the swallowing reflex and the reaction of the pupils to light;
- coma is a complete lack of reaction to what is happening; the patient’s vital activity is supported by special equipment.
Various disturbances of consciousness are present in almost all patients, say experts from the Clinical Brain Institute. Based on their condition, it is already possible to preliminarily predict their chances of recovery. Thus, if consciousness is maintained, the probability of death remains within 20%, with stunning - up to 30%, with somnolence - up to 55%, with stupor - up to 85%. With the development of coma, the prognosis is questionable - survival rate is no more than 10%.
Signs of the acute phase of stroke
The clinical picture of stroke includes several main syndromes. They are a consequence of acute cerebrovascular accident and occur when neurons die. These syndromes suggest a hemorrhagic stroke, even if the patient is conscious:
- anisocoria - the patient’s pupils are dilated unevenly and have different sizes;
- decreased severity of reflexes, including a slower reaction of the pupils to bright light;
- the appearance of an oculocephalic reflex - if a patient in a coma turns his head to the side, his pupils shift in the opposite direction;
- bulbar syndrome - decreased tone of the chewing, swallowing muscles and tongue, which is manifested by corresponding symptoms;
- pseudobulbar syndrome - a violation of swallowing, chewing and speech while maintaining the tone of the corresponding muscles.
Immediately after a hemorrhagic stroke, it is difficult to predict the likelihood of full recovery. The patient’s condition can only be determined dynamically, so the patient spends the first time under 24-hour medical supervision. The fact is that during the course of the disease there are often several critical periods during which the likelihood of relapse is increased. The first of them occurs on the second to fourth day after the attack, the next one appears 10-12 days later.
Terms of rehabilitation
There is no specific time frame for recovery after a cerebrovascular accident. The duration of the rehabilitation program depends on various factors:
- what size and location is the affected area;
- how quickly the patient received medical care;
- what type of stroke;
- what is the patient’s health status;
- what rehabilitation course is prescribed.
But in any case, a person and his loved ones should prepare for the fact that it will take at least three months to recover. Already in the first stages, it is possible to identify some prognostic factors that determine the timing and possibility of recovery:
- favorable – spontaneous return of lost functions, high-quality and early rehabilitation program, preservation of the patient’s intelligence and activity;
- unfavorable - a large lesion or its location in functionally significant areas of the brain, old age, cognitive or emotional disorders, severe severity of defects, poor health.
The following table will help you navigate the rehabilitation time frame.
| Type of stroke | Consequences | Possible outcome of a rehabilitation program |
| Pathology with minimal neurological deficit | Mild paralysis of the face or limbs, problems with vision and coordination | Partial return of lost functions in one to two months, full recovery in three months (the exact timing is determined by the state of health) |
| Severe neurological deficit | Extensive paralysis of the face or limbs, significant loss of coordination | The ability to self-care returns on average within six months; it can take years to restore lost functions |
| Severe hemorrhagic or ischemic stroke with persistent neurological deficit | Paralysis and other consequences of circulatory disorders lead to disability | Patients can partially recover in one to two years. A complete return to previous life is impossible due to the death of important neurons, whose functions cannot be performed by other cells. |
Diagnostic methods
In the acute phase of a hemorrhagic stroke, the patient must be urgently examined to preliminarily determine the prognosis and select treatment tactics. The condition is complicated by the following factors:
- extensive hematoma in the brain tissue, which occupies an area of 7 square cm or more;
- large intraventricular hematomas - more than 2 square cm;
- high blood pressure;
- elderly age of the patient;
- any chronic diseases;
- presence of dislocation syndromes.
Dislocation syndromes are signs of an increase in the volume of the brain with a subsequent change in its localization in the skull. Using these symptoms, you can determine in which area the main pathological focus is located, as well as predict the chances of recovery. The primary diagnosis of strokes is based on the clinical picture, so dislocation syndromes play an important diagnostic role. In total, there are 9 options for how the brain matter can shift. However, when diagnosing strokes, 2 of them are most important.
Treatment tactics
The treatment regimen is selected individually, depending on the examination results, the general condition of the patient and other factors, including age and concomitant diseases. The Clinical Brain Institute is a staff of professionals who will help you choose the right treatment regimen and will accompany the patient at all stages of treatment and rehabilitation. In case of stroke, conservative methods or surgical intervention may be recommended.
Conservative methods
In the acute period of hemorrhagic stroke, it is important to regulate blood pressure, as well as restore the level of blood circulation in the nerve tissues. This process is controlled by the systemic use of drugs from different groups:
- hypothetical agents for lowering blood pressure levels;
- potassium antagonists;
- antispasmodics and painkillers;
- sedatives;
- hemostatic drugs;
- antiprotease and antifibrinolytic groups;
- vitamin complexes;
- diuretics to prevent brain swelling;
- blood plasma substitutes.
Drug therapy is possible only if the size of the hematoma does not interfere with the normal functioning of the brain. As soon as the patient's condition becomes stable, measures can begin to restore lost skills. If with ischemic strokes this possibility appears within a few days after the attack, then after a hemorrhage in the brain the process takes longer.
Surgical treatment of hemorrhagic stroke
Surgery is performed to remove large hematomas that are preventing normal recovery. The operation is complex, so it is prescribed only in cases where conservative methods do not bring results. Thus, the size of a hematoma of 30 ml or more is considered critical - such a volume does not resolve on its own. Surgery is also recommended for hemorrhages in the cerebellar area, which are manifested by severe neurological symptoms. There are two methods of performing the operation: with access using classical and endoscopic methods.
Experts from the Clinical Brain Institute advise you to accept the decision voiced by your attending physician. If full treatment and rehabilitation are impossible without surgery, it is better to carry it out using endoscopy. However, there are also contraindications to surgery. These include medial hematomas and the patient being in a state of deep coma - in both cases, the risk of death during surgery is up to 100%.
Direct surgical removal of hematoma
| Direct surgical removal of hematoma |
Direct surgical intervention is used for subcortical hematomas of medium and large sizes, for large hematomas of lateral or mixed localization, accompanied by increasing edema and dislocation of the brain, deteriorating condition of the patient, for cerebellar hematomas. The operation consists of removing the hematoma by encephalotomy, aspiration of blood, removing dense clots with fenestrated tweezers and washing the wound with saline solution. After removing the hematoma, it is necessary to examine its walls and perform thorough hemostasis using coagulation and hemostatic agents. Better results can be achieved by using microsurgical techniques, which can significantly reduce the size of the encephalotomy and thereby minimize surgical brain trauma. For large VMH, accompanied by edema and dislocation of the brain, a wide osteoplastic craniectomy is performed with plastic surgery of the dura mater with periosteum or artificial materials. In case of cerebellar hematomas, it is advisable to supplement direct removal of the hematoma with the installation of external ventricular drainage.
Rehabilitation and prognosis
It is impossible to recover quickly after a stroke. This process begins once the patient is stabilized and can continue for many years. Doctors at the Clinical Brain Institute are confident that no two cases of hemorrhagic stroke are absolutely identical, so an individual program must be developed for each patient. It will include medication support, as well as sessions with specialists and at home. It is important to gradually restore motor, speech and social function, self-care skills, as well as the patient’s intellectual abilities. Rehabilitation includes simple exercises that must be performed daily, constantly becoming more complex. The process can be lengthy—many patients are unable to get up and move independently for the first few years after a stroke. However, fine motor skills and the ability to care for oneself improve within the first months. It is also worth contacting specialists in therapeutic massage and rehabilitation physical education - such activities significantly speed up the recovery process.
Hemorrhagic stroke is a dangerous condition, the prognosis of which largely depends on the speed of medical care. It is worth understanding that full rehabilitation of the patient is possible only if the doctors’ orders are followed, independent work and the support of loved ones. Specialists at the Clinical Brain Institute are ready to develop an individual program for each person who has suffered a stroke, as well as examine them throughout the entire rehabilitation period.
Clinical Brain Institute Rating: 5/5 — 4 votes
Share article on social networks
Puncture-aspiration method
| Puncture removal of hematoma with administration of fibrinolytic |
It is advisable to use the puncture-aspiration method for small lateral and medial hematomas accompanied by severe neurological disorders. The method consists of puncturing the hematoma with a catheter and simultaneously evacuating the liquid part of the hematoma. For precise positioning of the catheter, it is recommended to use neuronavigation. In some cases, drainage is carried out within 24 hours. The puncture-aspiration method with the introduction of fibrinolytics is indicated for lateral and medial supratentorial hemorrhages of medium size (from 30 to 60 ml) and for cerebellar hematomas (15–30 ml) provided the patient’s condition is stable. In this case, the technique is supplemented by fractional administration of fibrinolytic drugs at certain intervals. In the case of isolated ventricular hemorrhages, external ventricular drainage is performed with fractional intraventricular administration using fibrinolytics. According to the Research Institute of Neurosurgery, this method can reduce mortality in massive IVH by up to 40%, while in the natural course of this disease it approaches 100%.
Programs:
Assessment of rehabilitation potential
Movement restoration
Rehabilitation after stroke
Restoration of cognitive functions
Early (resuscitation) rehabilitation