Leukocytes are white nucleated blood cells that are the main components of the immune system.
They are formed in the red bone marrow. Their main task is to protect the body from foreign particles that lead to infections, inflammation and allergies.
The reference (acceptable) values of leukocyte content for adults are 4.0 – 9.0 x 109 U/l. In children, the norm depends on age.
An increase in the number of leukocytes in the blood above acceptable values is called leukocytosis.
Leukocytosis can be of two types: physiological (normal) and pathological. They differ in the reason for their occurrence, the mechanism of development, the duration of preservation and their significance for the body. Let's look at each separately.
Read more about blood tests in our article
“Hematological tests: norms and interpretation of results.”
Physiological leukocytosis
Associated with the redistribution of leukocytes, they move from the parietal pool (reserve) into the general bloodstream.
Physiological types of leukocytosis include:
- Digestive. 2-3 hours after eating, leukocytes are released from the depot into the blood, and it flows to the gastrointestinal tract for better digestion. Immune cells are necessary for the submucosal layer of the stomach and intestines for protection, since microorganisms contained in the air, water and on products enter the body with food.
- Myogenic (muscular). Intense muscle work triggers a cascade of reactions, stimulating the work of all organs, tissues and cells. During and after physical activity, the number of white blood cells can be 3-5 times higher than normal.
- Elevated leukocytes during pregnancy are a necessary measure to protect the mother’s body from infection entering the blood. If in the first trimester leukocytosis is relative, but by the third trimester the leukocytes exceed the norm by 2 times and this is not considered a pathology. In addition, leukocytes are involved in stimulating uterine contractions during childbirth.
- In the first 2-3 days of life, elevated leukocytes in a child are the norm. During pregnancy, the mother's immune system protects the fetus. After birth, all formed elements are actively released into his blood from the depot. Leukocytes are necessary to protect the child’s body from an aggressive external environment.
- Painful. When pain receptors are irritated, blood vessels constrict, blood pressure and adrenaline levels increase. This is a stress reaction, in response to which leukocytes are redistributed and released from the parietal reserve into the blood, leading to short-term leukocytosis.
- Stress. Emotional outbursts cause changes in blood vessels, hormonal surges, increased blood pressure and heart rate. In response to this, the number of leukocytes in the blood increases, as during painful stimulation.
With physiological leukocytosis, there is a slight increase in the number of leukocytes without changes in the leukocyte formula (the ratios of all 5 fractions of leukocytes). This phenomenon is short-term and harmless.
Indications for the study
To diagnose and analyze possible female diseases, a smear test is taken:
- It must be taken if any abnormalities occur in the menstrual cycle.
- You should also be concerned about pain in the lower abdomen and discomfort during sex.
- An indication for testing for elevated white blood cells is painful urination, which is accompanied by a burning sensation in the urethra.
- In patients who have taken hormonal drugs and antibiotics, a smear is also taken to detect elevated leukocytes.
- As for pregnancy, the analysis is mandatory at the first time a woman contacts her. If no deviations are found, then the next smear from the urethra is taken at a later date.
- In the absence of any suspicious symptoms, women are still recommended to undergo such an examination at least once every 3 months, since most pathologies in the early stages are asymptomatic.
Return to contents
Pathological leukocytosis
Pathological leukocytosis is the body’s response to an infectious agent or allergen.
Causes of increased leukocytes in the blood:
- Acute infections.
- Acute and chronic inflammatory diseases.
- Diseases accompanied by necrosis (disintegration) of tissues.
- Hypoxemia is a decrease in oxygen content in the blood.
- Actions of toxic substances.
- Oncological diseases.
- Diseases accompanied by immune reactions.
Do I need to prepare in any way?
To obtain reliable analysis results, you must adhere to several recommendations. During the week before the procedure, you should not use ointments, sprays, vaginal suppositories and other medications unless they have been specifically prescribed by your doctor. You should also refrain from sexual intercourse for 2-3 days before visiting a specialist. In the evening before the procedure, wash with warm water without soap; in the morning it is not necessary to undergo this procedure. It is advisable to avoid urinating before taking the test.
Types of leukocytes
Leukocytes are divided into two large groups:
- granular, which are characterized by the presence of a large segmented (divided into parts) nucleus and granules in the cytoplasm (the main semi-liquid mass of the cell, its internal environment). They are also called granulocytes.
- non-granular, which do not have specific granules in the cytoplasm (internal environment of the cell). Their second name is “agranulocytes”.
Each group has its own types of leukocytes. They differ in structure, appearance, properties and functions.
Granular leukocytes:
- Neutrophils.
- Eosinophils.
- Basophils.
Non-granular leukocytes:
- Lymphocytes.
- Monocytes.
Let's look at each subgroup in detail.
Neutrophils
They are the first to arrive at the site of injury - to places where tissues have been damaged and/or where microorganisms have penetrated.
The main task of neutrophils is to capture and digest microorganisms (bacteria and viruses).
A sharp increase in neutrophils in the blood (neutrophilia) indicates an acute inflammatory process, presumably of a viral nature. Most often, the proportion of immature forms—juvenile and rod forms—increases.
Eosinophils
Leukocytes with pronounced granularity of the cytoplasm (internal environment of the cell).
The main task of eoisnophiles is the destruction of parasites and participation in allergic reactions.
An increase in eosinophils in the blood is called eosinophilia. Its presence indicates the presence of a parasitic, allergic (systemic lupus erythematosus, rheumatoid arthritis) or cancer (eosinophilic leukemia, Hodgkin's disease) disease. In addition, eosinophilia is characteristic of bronchial asthma.
Basophils
The smallest population of leukocytes with fine granularity.
The main task of basophils is to release histamine, which is necessary for the inflammatory process and allergic reaction.
An increase in the content of basophils in the blood is called basophilia.
Basophilia indicates increased sensitivity of the immune system, which is typical in allergic reactions. For example, with urticaria or serum sickness.
Lymphocytes
Non-granular leukocytes with a large rounded nucleus. By size they are divided into large, medium and small.
There are 3 types of lymphocytes:
- T lymphocytes. The main components of cellular immunity. They destroy foreign particles, direct and regulate the activity of other immune cells and inhibit an excessive immune response.
- B lymphocytes. Participate in humoral immunity. They recognize foreign structures (antigens) and produce protective proteins (antibodies) to destroy them.
- NK lymphocytes. Destroys cells affected by bacteria and viruses, as well as tumor cells.
The main task of lymphocytes is to provide a specific immune response.
An increase in lymphocytes in the blood is called lymphocytosis. It is characteristic of acute infections and blood diseases (leukemia).
Monocytes
The largest leukocytes. They are not grainy, but have a large core.
Monocytes are macrophages, cells capable of absorbing and digesting large solid particles. After phagocytosis, macrophages, as a rule, do not die.
The main task of monocytes is to “clean up” the lesion from damaged or dead cells and microorganisms.
An increase in monocytes (monocytosis) occurs during infections, blood diseases, cancer, after surgery and during the recovery period.
What other causes of elevated white blood cells are there?
Leukocytosis in cancer
First of all, we are talking about acute and chronic leukemia, in which the number of leukocytes exceeds the norm tens of times.
What increases: neutrophils, monocytes.
Some metastases to the bone marrow can disrupt hematopoiesis (the process of formation of blood cells) and, on the contrary, can cause leukopenia - a decrease in the number of white blood cells.
Increase in leukocytes with tissue necrosis
Diseases and conditions accompanied by tissue breakdown:
- myocardial infarction;
- stroke;
- pancreatic necrosis (severe disease of the pancreas);
- intestinal infarction (abrupt cessation of blood supply to an area or the entire intestine, occurs when thrombosis or compression of the vessel supplying the organ);
- heart attack, injury or rupture of the kidneys;
- heart attack, injury or rupture of the spleen;
- extensive burns, etc.
What increases: neutrophils, monocytes (slightly, during recovery).
Leukocytosis in autoimmune diseases
Autoimmune diseases are pathologies in which the immune system produces antibodies (protective proteins) or NK lymphocytes against its own healthy cells. Simply put, the patient’s own immunity is destroyed, recognizing it as something foreign.
Diseases accompanied by immune reactions and leukocytosis in particular:
- Collagenoses are a group of pathologies characterized by inflammation of the vascular wall due to autoimmune reactions.
- Serum sickness is a severe allergic reaction to the administration of serums or drugs.
- Acute glomerulonephritis is an immune damage to the kidneys.
What increases: eosinophils, basophils, monocytes.
Other causes of leukocytosis
An increase in leukocytes in the blood can be caused by toxic substances (carbon monoxide, mercury, lead, etc.) or aggressive physical factors (ionizing radiation).
Leukocytosis is also characteristic of hypoxemia (decreased oxygen in the blood), which is typical of acute blood loss. In response to this, the body urgently releases formed blood elements from the depot into the vascular bed to maintain organ nutrition.
Leukocytes destroy all pathogenic particles, as well as defective or dead cells of the body. The leukocytes themselves are eliminated by the spleen. Therefore, after splenectomy (removal of the spleen), persistent pronounced leukocytosis is characteristic.
What increases: all white blood cells.
Online consultation with infectious disease specialist, allergist-immunologist Natalia Nikolaevna Gordienko
Online consultation
During the consultation, you will be able to voice your problem, the doctor will clarify the situation, interpret the tests, answer your questions and give the necessary recommendations.
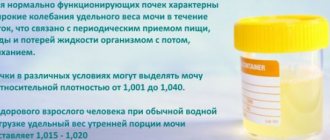
Norm of leukocytes in a smear in women (table)
As noted above, diagnostic material for a smear on the flora is collected from three points - the cervix, urethra and vagina.
And in each smear obtained, similar indicators are assessed, but the norms of some of them differ depending on the area of localization. Below is a table explaining the normal content of leukocytes, normal and pathogenic flora, cellular elements and mucus in a smear in women. Diagnostic criterion
| Normal indicators | |||
| Vagina (V) | Cervix (C) | Urethra (U) | |
| Leukocytes (Le) | 0-10 | 0-30 | 0-5 |
| Slime | moderately | — | |
| Epithelial cells | 5-10 | ||
| Key cells | — | — | — |
| Microflora | Gram-positive rods (bifido- and lactobacilli) ++++ | — | — |
| Yeast (Candida) | — | — | — |
| Trichomonas (Trich) | — | — | — |
| Gonococci (Gn) | — | — | — |
A smear that fully corresponds to the normal parameters is a rather rare phenomenon. However, minor deviations from the norm are allowed when it comes to the vagina. The urethra and cervix, if there are no pathologies, must be sterile - there should be no microflora there. Regarding the vagina, the situation is ambiguous.
Depending on the content of various microorganisms, there are 4 degrees of purity.
An ideal smear, free of leukocytes and pathogenic flora, corresponds to the first. However, most women cannot boast of such results. Often, individual leukocytes are found in the vaginal discharge within the normal range (up to 10 pcs.), an insignificant content of epithelial cells and opportunistic bacteria. This picture is not characterized as pathological, and the smear belongs to the second degree of purity.