This site was made by experts: toxicologists, narcologists, hepatologists. Strictly scientific. Tested experimentally.
Author of this article, expert: Gastroenterologist-hepatologist Ekaterina Kashukh
Briefly: Liver parenchyma is its functional tissue. If the organ is sick, then the parenchyma can no longer fully perform its work. When treating the liver, in addition to medications, it is necessary to maintain a healthy lifestyle: a balanced diet, weight loss, blood sugar control.
- What tissues does the liver consist of?
- What is parenchyma
- What is the microstructure of the liver
- How the parenchyma changes during diseases
- Cell dystrophy
- Hepatocyte necrosis
- Inflammation
- Fibrosis and cirrhosis
- Symptoms of parenchymal damage
- How is diagnostics carried out?
- How are changes in the liver parenchyma treated?
What is parenchyma
The word “parenchyma” literally translated from Greek means “poured around, nearby.” In medicine, this term refers to the main functionally active tissue of all dense (not hollow) organs: for example, the liver, kidneys, lungs, pancreas and prostate glands.
The parenchyma in the liver is represented by glandular epithelium, which in appearance resembles a sponge. Thanks to this structure, the filtration function of the liver is ensured.
- The outside of the gland is covered with stroma: it is a durable capsule that consists of connective tissue fibers. It plays a protective, supportive and organ-forming role. The stroma protects the parenchyma from external influences.
- Partitions (trabeculae) extend from the capsule deep into the liver, dividing the entire organ into lobes and segments. Nutrient blood vessels, bile ducts and nerves pass through their thickness.
- Inside the liver, connective tissue fibers from the stroma branch to form cells. Each of them contains a mass of cells forming parenchyma. In humans, this cellular structure is weakly expressed (but, for example, in the liver of pigs it is highly developed).
Important! Parenchymal organs differ from hollow ones in that they consist of a dense mass of cells, which is covered on top with a strong connective tissue capsule. The processes of the outer shell divide the entire organ into separate structural elements.
Meristem (Educational tissue)
Meristem (Educational tissue)
Educational or Meristem (from the Greek meristos - divisible). The cells are living, thin-walled, have thin cell walls with a small amount of cellulose, with a large nucleus, and often divide. They give rise to almost all cells of other tissue types and ensure the growth of the plant throughout its life. With each division, one of the newly formed cells remains meristematic, and the second turns into a cell of some tissue. Division is regulated by phytohormones.
Types of educational fabrics
Based on their location, apical, intercalary and lateral meristems are distinguished. The apical ( apical ) is located in the zone of root division and the growth cone at the tip of the shoot. It ensures their growth in length. It is laid in the body of the embryo. Each lateral shoot and lateral root develops its own apical meristem.
The lateral one is located inside the stem or root and covers their central part. Ensures the growth of these organs in thickness. For example, cambium is found mainly in trees, sometimes in herbaceous plants.
The intercalary (intercalary) is found at the base of the stem internodes in some plants (cereals, horsetails) and provides intercalary growth. This meristem ceases to exist and turns into permanent tissues when the growth of the stem section or leaf ends.
There are also primary and secondary meristems. The primary meristem develops in the embryo and determines the growth and development of the seedling. It is formed at the tops of the embryonic root and stalk. The secondary is formed from the primary and is formed later. Secondary meristems provide secondary growth in thickness of the stem and root (cambium and phellogen). The cork cambium arises from the cells of the main tissue or epidermis. Among the secondary meristems, a wound one is distinguished, which gives rise to special protective tissue in places of damage.
Parenchyma (Main tissue)
The main tissue or parenchyma (from the Greek parenchyma - poured nearby). It makes up the majority of all plant organs. It fills the gaps between conductive and mechanical tissues and is present in all organs. The parenchyma consists of living cells with relatively thin walls. They may have large spaces - intercellular spaces . Individual parenchyma cells can perform a secretory function. Under certain conditions, parenchyma cells can restore the ability to divide and form a cork cambium, etc.
Types of main fabric
There are: assimilation, storage, air-bearing, aquiferous parenchyma.
- Types of plant tissues: educational, integumentary, basic mechanical conductive
Assimilation , or chlorophyll-bearing (chlorenchyma) . Photosynthesis occurs in it. Consists of living cells containing chloroplasts. It is found in green plant organs, mainly in leaves. In leaves it is also called mesophyll .
Storage . Found in all plant organs (stem, root, rhizome, etc.). Sometimes it forms separate layers. The storage parenchyma consists of colorless cells with a large number of inclusions. Leucoplasts are located in the cells, and sometimes chromoplasts are located in the parenchyma of flowers and fruits. Storage substances - carbohydrates, proteins, fats.
Pneumatic , or aerenchyma (from the Greek aer - air). This tissue has large intercellular spaces filled with air. Performs the functions of gas exchange and transfer of gases to different tissues. Characteristic mainly of aquatic plants.
Aquifer . The cells have vacuoles that help retain moisture. Characteristic of plants that grow in dry places.
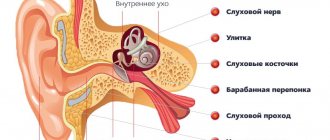
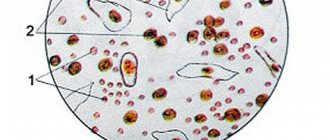
What is the microstructure of the liver
The hepatic lobule is the main morphological and functional unit of the organ. All lobules have a shape similar to a prism and are inserted into one another. The size of each of them does not exceed 2 mm. There are about a million lobules in the liver.
The most important and numerous cells of the parenchyma are hepatocytes (from the words “hepar” - liver, “citus” - cell), all the main biochemical reactions take place in them. In addition, there are other cells:
- endotheliocytes - located in the wall of intralobular capillaries, participate in the restoration of liver tissue, the formation of lipoproteins and sugars;
- Kupffer cells (stellate macrophages) - promote the disposal of old red blood cells, take part in blood detoxification, protect the liver from infection;
- pericytes - needed for the formation of connective tissue in damaged areas of the parenchyma;
- intrahepatic lymphocytes (pit cells) - kill hepatocytes damaged by viruses and have antitumor activity.
Important! All structural particles of the liver are in complex interaction with each other, aimed at maintaining the health of the organ. In liver diseases, this cooperation is disrupted.
Flatworms
Parenchyma is a tissue consisting of cells and intercellular spaces that fills the interior of the human body. flatworm, which is an acoelemate. It is a spongy tissue, also known as mesenchymal tissue, which contains extracellular matrices. Parenchymal cells include: myocytes, and many types of specialized cells. Cells often attach to each other, as well as to nearby epithelial cells, primarily through gap junctions and hemidesmosomes. Parenchyma cell types vary greatly depending on the species and anatomical region. Its possible functions may include skeletal support, nutrient storage, movement, and many others.[13]
How the parenchyma changes during diseases
Liver tissue undergoes changes under the influence of various unfavorable factors (alcohol, viruses, toxins). They may be different.
How to protect the liver parenchyma from damage. Infographics.
Cell dystrophy
Cell dystrophy is the morphological expression of a disorder of tissue and cellular metabolism. According to the nature of metabolic disorders, there are fatty (the most common), protein, carbohydrate, and mineral dystrophy:
- With the fatty type (lipidosis), there is an increase in the concentration of neutral fat in the cytoplasm, followed by oxidation and cell destruction. The causes may be alcohol intoxication, fasting, obesity, pathology of the endocrine system (diabetes, thyroid disease).
- With a disorder of protein metabolism (dysproteinosis), changes in cytoplasmic proteins and destruction of cell membranes are observed. The cause may be viruses, alcohol, toxins, electrolyte imbalances, and circulatory disorders.
- Carbohydrate (glycogenosis) dystrophy can be congenital (enzymepathies) and acquired (diabetes). Changes in cells are caused by impaired metabolism of glycogen (a storage form of glucose) and glycoproteins (protein-carbohydrate compounds). This can happen with leukemia, anemia, inflammation.
- Mineral dystrophy appears when there is excessive accumulation of copper (this is hereditary Wilson-Konovalov disease) or iron (hemochromatosis) in liver cells.
The listed morphological changes are characteristic of a group of liver diseases called hepatoses.
They can lead to the development of fibrosis and cirrhosis of the liver. Subscribe to our YouTube channel!
Hepatocyte necrosis
Hepatocyte necrosis is an irreversible process of tissue destruction and cell death. It can develop when the blood supply to an organ is disrupted or stopped, as well as under the influence of mechanical, infectious, chemical, and temperature factors.
The distribution of necrosis is:
- Local (occurs in a separate part of the liver).
- Focal (a group of adjacent lobules).
- Scattered (in several places of the liver at the same time).
- Massive (death of most of the parenchyma).
The most common causes of necrosis:
- viral hepatitis,
- extensive injuries,
- autoimmune pathologies,
- metabolic diseases,
- acute poisoning, including alcohol intoxication.
Also read the article about how to identify and treat necrotic processes in the liver, what the prognosis depends on and how to prevent cell necrosis.
What causes inflammation
Inflammation of the parenchyma begins when cells are damaged by viruses, alcohol, toxins, and drugs. Inflammatory processes in the liver are called hepatitis (from the Greek “hepar” - liver, “itis” - a suffix denoting inflammation of this organ). Wherein:
- There is degeneration of hepatocytes, sometimes turning into necrosis.
- In response to cell damage, substances that provoke inflammation are released and vascular permeability increases.
- This leads to the appearance of inflammatory cell infiltration (compaction) in the parenchyma.
- The end result is proliferation - restoration of damaged tissue and limitation of the source of inflammation due to the formation and accumulation of collagen fibers.
Fibrosis and cirrhosis
In conditions of chronic degeneration of hepatocytes, their death occurs, and connective tissue, similar to a scar, accumulates at the site of destruction. Gradually, normal parenchyma is increasingly replaced by functionally inactive dense fibrous tissue.
The most common causes of fibrosis:
- alcoholism,
- long-term exposure to toxins,
- chronic inflammatory diseases (viral hepatitis C and B),
- severe systemic pathologies,
- heredity.
Fibrosis can be focal or diffuse (distributed throughout the organ). If left untreated, sooner or later it turns into cirrhosis.
At the same time, the connective tissue permeates the entire organ; normal parenchyma tries to break through between its fibers due to regeneration. This leads to the formation of nodules and knots. They compress the vessels, blood circulation is disrupted, which aggravates the pathology.
Symptoms of parenchymal damage
Symptoms of dystrophy correspond to the underlying disease. The liver itself cannot hurt, since it has no nerve endings. Pain appears only when the liver is significantly enlarged and the capsule is stretched.
Before this, a person may be concerned about:
- general malaise, weakness;
- dyspepsia (nausea, loss of appetite);
- hepatitis due to cell destruction and disruption of bilirubin metabolism is manifested by jaundice, darkening of urine and lightening of feces;
- with serious protein dystrophies, there is a tendency to bleeding, bruising, and swelling;
- with extensive necrosis of hepatocytes, a lot of bilirubin is released, which affects the brain, encephalopathy occurs (impaired memory, attention, consciousness) and the risk of hepatic coma.
Subscribe to our YouTube channel!
Fibrosis has no specific symptoms; pathology can be discovered accidentally during an examination for another reason. Jaundice, ascites, skin itching and bleeding appear in advanced cases, already with the development of liver cirrhosis. In such patients, characteristic signs are also:
- spider veins on the body,
- erythema on the palms,
- expanded network of saphenous veins in the abdomen,
- accumulation of fluid in the abdomen (ascites).
For more information on how to identify this disease, read the article about the symptoms of cirrhosis.
How is diagnostics carried out?
Detection of liver diseases is carried out using laboratory and instrumental methods. A blood test for liver tests helps to determine the presence and degree of inflammation activity, to suspect the presence of bile stagnation, cirrhosis or a tumor process in the parenchyma.
Advice to a sick person from gastroenterologist Daniela Purgina, an expert on the website Pokhmelye.rf.
Don't refuse to get tested. Since the liver parenchyma does not have nerve endings, we can only find out that a pathological process is occurring in it by donating blood. To check, a biochemical blood test is taken for ALT and AST. The enzymes ALT and AST are found in many cells of our body, but the largest amount of ALT is found in liver cells, so its increase in the blood serves as a marker of pathological processes in the liver. AST, in addition to the liver, is also found in the heart muscle and skeletal muscles, pancreas, kidneys, lungs and blood cells. In the liver itself, ALT is located in the internal environment of the cell (cytoplasm), AST is in the cytoplasm and mitochondria (an organ inside the cell that provides it with energy). And when cells are destroyed, these enzymes enter the bloodstream.
There is always a certain amount of ALT and AST in the blood, since a certain number of liver cells die during the renewal process: old cells are replaced by new ones, and this is a normal physiological process. With normal renewal of liver cells, the level of ALT and AST is within certain limits, which are indicated on the laboratory form.
Ultrasound diagnostics allows:
- find out the size, shape, contours of the liver;
- assess the condition of the structure of the liver, bile ducts and blood vessels;
- see focal changes, the presence of neoplasms.
In a healthy person, the structure of the parenchyma looks like this on the monitor:
- the image of the organ is fine-grained (many evenly spaced linear and point structures);
- echogenicity - corresponds to or slightly higher than the standard (this is the renal cortex);
- sound conductivity of deep structures is good.
With pathology of the parenchyma, the ultrasound picture changes:
- Fatty degeneration. The size of the liver may be increased slightly, the contours of the organ are clear and even, the shape does not change, and the outer capsule is not visible. The tissue structure is moderately heterogeneous, the vascular pattern is depleted, and sound conductivity is reduced. The general echogenicity is increased; in the focal form it is detected in the form of single volumetric formations.
- Hepatitis. In the acute form of the disease, an increase in the size of the organ is detected. Prominent vessels are characteristic. In chronic inflammation, the structure of the parenchyma is uneven, the vascular pattern is depleted.
- Cirrhosis. The shape of the organ can change, the contours are lumpy and uneven, the size of the liver can be either increased or decreased. The structure is heterogeneous and uneven. The vascular pattern is poor, the veins are dilated (portal, hepatic, splenic).
Important! It is not always possible to unambiguously interpret changes in the liver parenchyma detected on ultrasound. A definitive diagnosis may require computed tomography or magnetic resonance imaging with contrast, sometimes a liver biopsy or elastometry.
If ultrasound is not enough, then the liver parenchyma is checked by other methods.
References
- "Parenchyma". Merriam-Webster Dictionary
. Retrieved 2017-06-08. - "Parenchyma". Oxford Dictionaries British Dictionary
. Oxford University Press. Retrieved 2017-06-08. - Lemone, Priscilla; Burke, Karen; Dwyer, Trudy; Levett-Jones, Tracey; Moxham, Lorna; Reid-Searle, Kerry; Berry, Kamari; Carville, Keryln; Hayles, Majella; Knox, Nicole; Luxford, Yoni; Raymond, Debra (2013). "Parenchyma". Medical-surgical nursing
. Pearson Australia. paragraph G – 18. ISBN 978-1-4860-1440-8. - Virchow, R.L.K. (1863). Cellular pathology based on physiological and pathological histology
[…] Rudolf Virchow. Translation from 2nd ed. original by Frank Chance. With notes and numerous corrections, mostly from MS. author's notes. 1–562. [Wed. p. 339.] link to the site. - Geiger, S. S. 1915. Ballot for naming the façade of the laboratory building, Brooklyn Botanic Garden. Rec.
Brooklyn Bot. Guard. IV, pp. 105–123. link. - “What is brain parenchyma? (With illustrations)".
- "Lung parenchyma." Retrieved February 9, 2021.
- Suki, B. (July 2011). "Mechanics of the lung parenchyma." Integrated Physiology
.
1
(3):1317–1351. doi:10.1002/cphy.c100033. ISBN 9780470650714. PMC 3929318. PMID 23733644. - Kmieć Z (2001). Liver cell collaboration in health and disease
.
Adv Anat Embryol Cell Biol
.
Advances in anatomy, embryology and cell biology. 161
. pp. iii–xiii, 1–151. Doi:10.1007/978-3-642-56553-3_1. ISBN 978-3-540-41887-0. PMID 11729749. - Ashton, Leah; Gullekson, Russ; Hurley, Mary; Olivieri, Marion (April 1, 2021). "Correlation of kidney size with the number of renal pyramids in goat kidney". FASEB Magazine
.
31
(1_addition): 899.5. DOI:10.1096 / fasebj.31.1_supplement.899.5 (inactive 09/10/2020) - via fasebj.org (Atypon).CS1 maint: DOI inactive as of September 2021 (link to website) - Walter F. Boron (2004). Medical Physiology: A Cellular and Molecular Approach
. Elsevier/Saunders. ISBN 978-1-4160-2328-9. - Connolly, James L.; Schnitt, Stewart J.; Wang, Helen H.; Longtine, Janina A.; Dvorak, Anne; Dvorak, Harold F. (2003). "Tumor structure and tumor stroma formation." Holland-Frei Cancer Medicine.
6th edition . - Conn, D. (1993). "Biology of flatworms (Platyhelminthes): parenchyma cells and extracellular matrices". Proceedings of the American Microscopic Society
.
112
(4):241–261. Doi:10.2307/3226561. JSTOR 3226561.