Structure
The sclera occupies 5/6 of the fibrous membrane of the eye. The thickness varies from 0.3 to 1 mm in different places. The thinnest part is located in the area of the equator of the eye, in the area of the optic nerve exit, near the cribriform plate, where the axons of ganglion cells extend beyond the eyeball. Staphylomas or bumps can form in these areas when intraocular pressure increases.
Sometimes excavation of the optic disc occurs. This condition is characteristic of glaucoma. The scleral membrane along with the attachment of the extraocular muscles is damaged after injury.
The sclera consists of the following elements:
- the episclera is a loose layer through which many veins and arteries pass in the superficial and deep parts of the vascular network;
- the substance of the sclera, consisting of collagen and elastic fibers;
- the dark scleral plate, formed from connective tissue and pigment cells, is located between the vascular network and the sclera.
In the back of the eyeball, the sclera is formed in the form of a narrow lattice plate, allowing the optic nerve and blood vessels to supply the retina with useful substances. The protective layer of the optic nerve is formed 1/3 from the cribriform plate and 2/3 from scleral tissue.
The cornea, sclera and conjunctiva are connected at the limbus. This structural feature affects the development of polymorphic diseases, inflammation, allergic reactions, tumors and genetic abnormalities.
A dense nerve plexus is located on the circumference of the limbus, formed from the ciliary nerves, and the fibers responsible for the sensitivity of the cornea extend from it. The scleral tissue has few nerve endings; this feature affects the development of diseases characteristic of collagenosis.
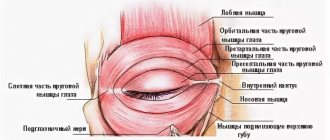
Three pairs of extraocular muscles attach to the surface of the sclera. Nerves and arteries pass to the choroid through special channels or emissaries. A circular groove up to 0.75 mm thick is located on the inner surface of the anterior part of the sclera. The ciliary body is attached to dense tissue in the form of a ring through which blood vessels pass.
The anterior part of the groove is located near Descemet's membrane. At its bottom, near the posterior edge, there is a venous sinus of the sclera, which is called Schlemm’s canal. The trabecular meshwork occupies the remainder of the scleral recess.
What types of this disease occur?
There are a number of diseases that can accompany the formation of inflammation:
- acute rheumatoid arthritis;
- systematic bloody lupus;
- polyarteritis nodosa;
- allergic reactions of the body;
- response to chemicals;
- infectious diseases or parasitic microorganisms.
Inflammations are usually divided into diffuse and nodular. In the first case, inflammation is expressed in redness throughout the entire area of the eyeball. In another case, the disease appears as a small nodule with obvious redness.
The nodular type of pathology lasts much longer than the diffuse one. Sometimes this can drag on for several weeks, and sometimes even 5-6 months. It may happen that the disease spreads to both eyes. After the treatment course, the nodules will begin to dissolve, leaving behind a small black-gray mark. With this type of deviation, photophobia and lacrimation do not appear.
Another type of this deviation is considered to be migratory inflammation. It is a hyperemic infectious focus inside the eye. It may be accompanied by quite severe swelling of the eyelid and frequent headaches. Unlike previous types of illness, this one goes away in a couple of days and not even a trace remains of it.
In episcleritis, symptoms can occur with varying degrees of intensity. It all depends on how exactly the pathology is expressed and how widespread it is. This disease is characterized by the occurrence of pain, which can begin as mild discomfort and end with quite severe pain. This type of disease is not as serious as inflammation of all the membranes of the sclera.
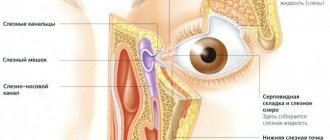
When blood vessels dilate, localized or widespread redness occurs. This depends on the strength of the inflammatory process. The patient will have intense tear production. This is due to the fact that the nerve receptors in the eye are highly irritated, so the body tries to reduce this irritation to a minimum.
Functions
The main functions of the sclera:
- 2/3 of its thickness is the protective sheath of nerve fibers;
- in the area of the equator of the eye, 4-6 vortex veins pass through the sclera;
- the sclera is the attachment point for the eye muscles, which ensure good mobility of the organ of vision in all directions;
- The sclera passes sensory nerve fibers to the eyeball, sympathetic innervation is directed from the superior cervical ganglion.
The arteries pass through the sclera to the back of the eye.
Treatment
In most cases, red eyes are fairly easy to eliminate. If this is caused by overwork, take a little time to walk in the fresh air, try to get a good night's sleep and give your eyes a temporary break while working. Buy special glasses for working at a computer - they will reduce the load on the eye muscles.
It is very useful to do eye exercises: blink frequently; move your gaze several times from a distant object to a near one; make rotational movements with your eyeballs. If the indoor air is extremely dry, purchase a humidifier or use drops with the effect of artificial tears.
You should not delay going to the doctor if redness of the sclera is accompanied by the following symptoms:
- Unbearable headache, dizziness, nausea and vomiting. All this may indicate an increase in blood pressure, or be an attack of glaucoma;
- Visual impairment appears: objects split into two, light spots appear;
- The appearance of purulent discharge;
- The redness lasts for more than two days.
Take care of your vision and carefully monitor your eye health.
Pathologies of the sclera
Congenital diseases:
- Melanosis occurs due to poor carbohydrate metabolism with an increased amount of melanin in the scleral tissues. The tunica albuginea turns yellow in this disorder.
- Aniridia is a rare disorder involving the absence of the iris. The pathology manifests itself due to changes in the gene responsible for the normal development of the visual organs. Sometimes acquired aniridia occurs after injury or inflammation of the iris.
- Blue sclera syndrome, in which the whites turn bright blue. The disorder is accompanied by deterioration of vision, hearing and a decrease in the amount of iron in the body. Sometimes the syndrome develops as a symptom of hereditary pathologies.
Acquired diseases:
- Episcleritis is an inflammation of fibrous tissue that becomes covered with dense nodules. The disorder is diagnosed more often in women over 40, and is rarely detected in children. The pathology affects both eyes and becomes chronic without timely treatment.
- Scleritis is an inflammation of all layers of the sclera. The disorder is accompanied by pain, swelling, and blurred vision. Destruction of the tunica albuginea occurs without timely therapy. The disorder affects only one eye and is more common in women.
Staphylomas occur after loosening of collagen tissues in complex forms of myopia. Patients' vision decreases, fatigue increases, and a feeling of heaviness arises.
Complications of scleritis
Some consequences of an unfavorable outcome have already been mentioned. Sometimes the inflammation is complicated by the cornea, iris and ciliary body. Because of this, adhesions form between the lens and the pupillary edge of the iris. This leads to blurred vision and clouding of the anterior chamber of the eye. The main complications of scleritis:
- keratitis;
- iridocyclitis;
- opacity in the vitreous body;
- thinning of the sclera;
- deformation of the eyeball;
- astigmatism;
- secondary glaucoma;
- retinal detachment;
- corneal clouding;
- endophthalmitis;
- panophthalmitis.
According to medical statistics, 14% of patients have severe vision deterioration in the first year of illness. Approximately 30% of patients notice a decrease in visual function within 3 years after inflammation. 50% of patients diagnosed with necrotizing scleritis die within 10 years. Death occurs mainly from a heart attack.
The outcome depends on the form of the pathology and when treatment is started. An unfavorable prognosis is not often made. It is only important to identify the disease in time.
How is scleral condition diagnosed?
An examination by a doctor is carried out after identifying a violation of the sclera. Symptoms associated with scleral tissue disorder:
- eyes hurt when muscle tissue contracts;
- sensation of a foreign object in the eye;
- uncontrollable tearfulness;
- the color of the sclera changes;
- changes in the structure of the eye, deformation of certain areas of the surface, dilation of the arteries.
Diagnostic methods:
- listing the number of Placido rings;
- scanning through an optical slit;
- examination using a Schleimpflug camera;
- study of raster images;
- laser interferometry.
Deformation or clouding of the cornea is a complication after which a person becomes partially or completely blind.
Diagnostics
Diagnosis of episcleritis includes interviewing the patient, physical examination, and the use of laboratory and instrumental methods. At the appointment, the attending physician will examine the patient’s medical history, since a history of infectious and autoimmune diseases increases the risk of episcleritis.
Questioning and examination will help identify characteristic symptoms and clinical signs of the disease, although the external manifestations of episcleritis may in many ways resemble conjunctivitis.
Laboratory and instrumental methods help clarify the condition of the eye and determine the form of episcleritis. Doctors may order the following tests:
- Complete blood count, including determination of antibodies, rheumatoid factors, erythrocyte sedimentation rate and other parameters. A blood test helps identify the primary disease that caused episcleritis.
- Chest X-ray to detect tuberculosis.
- CT scan.
- Instrumental examination of the eye using a slit lamp.
- Less commonly, ultrasound and biopsy.
An important part of the patient's examination is differential diagnosis. This method helps distinguish episcleritis from similar diseases, including anterior uveitis, scleritis and conjunctivitis.
Doctors rule out scleritis with phenylephrine or neosynephrine eye drops. These substances cause changes in the blood vessels of the eye only in episcleritis.
Useful video
More useful information about the functions of the white membrane of the eye can be obtained by watching the video.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2031
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 1 ratings, average: 5.00 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.
Causes of the disease
The main causes of the development of scleritis are usually considered to be rheumatological diseases, including: Wegener's granulomatosis, polyarthritis nodosa and relapsing polychondritis, as well as some other diseases, the risk of developing scleritis in which is no more than 50% of cases.
It is also customary to distinguish post-surgical scleritis, in which inflammation of the sclera can develop within six months after surgery. However, there is an assumption that the impetus for the disease in this case is some kind of rheumatological disease.
With infectious scleritis, the cause of the disease lies in the spread of a certain bacterial infection from the cornea of the eye.
Scleritis - what is it, types of pathology
Many diseases can resemble scleritis, so only a specialist can distinguish them.
Scleritis is an inflammatory process that covers all layers of the outer layer of the eye. There is both unilateral and bilateral damage.
There are two options for classifying the disease: by morphological nature and by the affected department.
Fundamentally, the eyeball is divided by an invisible line, the equator, into two parts. Hence the logical conclusion is that there is:
- Anterior scleritis – the visible part of the sclera is affected.
- Posterior scleritis - inflammation develops in the area of the sclera that is inaccessible to inspection.
The second option is considered more rare and is characterized by a severe course. Note that these conditions can flow into one another with unsuccessful treatment, or the absence of it at all.
Depending on the substrate of the pathology, the following forms are distinguished:
- Nodular - characterized by the presence of one or several affected areas of the sclera in the form of nodules that do not move and rise slightly above its surface, often having a purple color.
- Diffuse – the disease affects large areas on the surface of the eye.
- Necrotic is the most serious type of scleritis. There are two variants of the course: inflammatory, which is a consequence of an advanced process of inflammation, and the second type is primary necrotizing, when destruction of scleral tissue immediately occurs, without a previous inflammatory component.
The nodular form is the most favorable; with adequate treatment, undesirable consequences can be avoided; vision deterioration occurs in 25% of patients.