Structure
The functionality and structure of these amazing muscles should be studied in detail. The eyelids cover the outer part of the eyes and protect from external factors. Main functions:
- protection against the ingress of small particles and foreign objects;
- uniform distribution of tear fluid;
- responsible for moisturizing the cornea and conjunctiva;
- washes away small particles from the surface of the mucosa;
- protect eyes from drying out during sleep;
- are responsible for the blinking process.
The edges of the eyelids are 2 mm thick. The lower and upper eyelids close tightly when closing the eyes. Eyelashes grow on the smoothed anterior rib. The inner one is sharper and fits tightly to the eyeball. The intermarginal space is located along the length of the eyelids, between the anterior and posterior parts. The skin is thin, so it tends to gather in folds. When the eyes open, it folds inward with the help of the muscles that are responsible for raising the eyelids. This creates a deep crease. Another, less pronounced one is located on the lower eyelid.
There is also a circular muscle, which is located under the skin in the orbital or palpebral part. In the process of closing the eyelids, both muscles contract. The dense tuft that emanates from the frontal origin of the maxilla is the internal ligament of the eyelid. It bifurcates and connects to the ends of the cartilage of the eyelids.
Eyelid exercises
The Facebuilding technique for eyelids offers the following technique for swelling, blue circles and tear troughs:
Place your index fingers on your forehead above your eyebrows, and place your thumbs below your eyes. Cover your eyelids. Spread your fingers outward from the eyelids, gently applying pressure. Do this exercise for 40 seconds and then rest.
Strengthening the orbicularis oculi muscle
- The technique works the orbicularis oculi muscle and others nearby: the temporalis, the procerus muscle. Executes slowly. Find a point at the level of your eyelids and slowly protrude your eyes, looking at this point. By doing this exercise, you will feel how not only the muscles of the eyes work, but also the muscles of the temples and nose. Relax your eyes, close them, then start protruding them again. Repeat slowly ten times. Then relax your eyelids completely. You can rub your palms together and apply them to your eyes;
- Move your pupils in a zigzag pattern, first from left to right, from the imaginary left viewing angle to the right, then gradually going down in a zigzag, then back;
- Then do the same thing, just move in a zigzag from bottom to top, from the imaginary left viewing angle down, then up, gradually moving from left to right and then in the opposite direction;
- With your eyes closed, move your pupils in a circle ten times in one direction and the same number in the opposite direction.
The last technique perfectly copes with age-related sunken eyes when performed regularly.
To widen the outer part of the eye
- Place your hands on your temple in such a way that the fingers of one palm look at the fingers of the other palm: the palm, where the fingers are pointing down, rises slightly towards the hair, the other, where the fingers are pointing up, moves slightly towards the ear;
- After creating tissue pretension, the skin should become slightly moisturized, after which the hands will begin to move on their own.
How to tighten your upper eyelids
- Place your index fingers on top of your closed eyelids. Try to open them by counting to eight. Then blink and repeat 3 times;
- Place the tip of your index finger on the upper eyelid. Pull the outer edges of the eyes towards the temples. Use your upper eyelid to press as hard as you can onto your lower eyelid. Perform sixty presses. Look in the mirror. Pay attention to whether you frown.
Functions
The circular muscles are an irreplaceable part of the visual apparatus, on which the functioning of the eyelids depends. They perform very important functions:
- responsible for the blinking process;
- active muscle is responsible for wakefulness;
- moisturize the mucous membrane;
- prevent drying of the cornea during sleep.
The condition of the eyelids is very important for healthy eyes. Control of the width of the palpebral fissures is also determined by them. Subject to various pathological diseases and processes. The most common is a pathology called ptosis. It can manifest itself in varying degrees of damage and cause severe complications.
During sleep, the eyes have the opportunity to relax and rest. The eyelids provide this rest. They control the distribution of tear fluid, moisturize the mucous membrane, and prevent drying out during sleep. In addition, they protect the eyes from small particles and foreign objects.
If unpleasant eye symptoms occur or occur against the background of endocrine or neurological diseases, then they must initially be cured. Drug therapy is prescribed by a doctor only after confirmation of the diagnosis. In addition, self-medication is prohibited.
Exercises for the main muscles of the eye
External eye muscle training
An effective set of exercises allows you to strengthen your external muscles. This ensures a higher quality and three-dimensional image. Regular exercise helps to achieve good vision and maintain healthy visual organs.
Training:
- Blink quickly for 20 seconds. Close your eyes and open them wide. Blink quickly again.
- Imagine that there is a rainbow in front of your eyes. Smoothly walk around the arc from one end to the other and back. Then imagine an inverted rainbow. Make arcuate movements with your eyes, lingering for a few seconds at the extreme points and lower part of your field of vision.
- Look straight ahead. Imagine that this is the center of the spiral. Make rotational movements with your eyes along a spiral trajectory. With each revolution, increase the diameter of the coil along which the gaze follows. Try to rotate your eyes a little further, beyond the limits of comfort.
- In a sitting position, slowly move your gaze from top to bottom, then from right to left. Repeat the exercise 12 times.
Training the internal muscles of the eye
The ciliary muscle of the visual analyzer is trained using the “mark on glass” method and on an accomodo trainer.
Exercise “mark on glass”:
- Attach a round mark to the window glass. It should be at eye level.
- Sit 30 cm further from her.
- Move your eyes to the mark and a distant object behind the glass (tree, car, walking person).
Perform the gymnastic complex 2 times a day for 3 minutes. After 2 days, increase the training duration to 5 minutes, after another 2 days to 10 minutes.
To make an accomodo trainer, you will need to cut out a figure from thick cardboard, similar to a table tennis racket. Make a 50 cm long slot above the handle into which a ruler can fit.
Draw the letter “C” in the center of the figure. Put on glasses or lenses, add an additional +3 lens to one of them. Close the second eye. Place a ruler next to the open one, slowly move the rocket along it until the contours of the letters merge into a circle.
Perform the training for 7-10 minutes with each eye.
Exercises for the six main muscles of the eye
Gymnastics is performed standing in a relaxed state. Do not move your head or body while performing the exercises.
Complex:
- Look at the ceiling, then at the floor. Do not move quickly, the eyes must do the work intended for them. Shift your gaze slowly, without looking at foreign objects.
- Move your gaze to the right and left. Move your eyes to the sides as far as the extraocular muscles allow. Do not try to complete the exercise if there is pain. In the future, this exercise will make the muscles more elastic and you will be able to completely look away to the side.
- Draw lines diagonally. Stand with your back to the wall. Move your eyes from the upper right corner of the room to the lower left. Then do the exercise in reverse. This workout strengthens the muscles, it loads them and makes them function fully.
- Take a hoop and hang it in front of your eyes or imagine a large circle. Slowly roll your eyes along the line of the hoop. The gaze should glide smoothly along the rim.
Each exercise is repeated 10 times. One workout a day is enough. This complex allows you to load all 6 muscles of the visual analyzer. If you do the work regularly, you will be able to significantly strengthen them.
Symptoms of pathologies of the orbicularis oculi muscle
Ptosis is a pronounced pathology, which is accompanied by drooping of the eyelid (mainly the upper one). In most cases, the pathology is unilateral. Bilateral lesions are rarely observed. Asymmetry of the eyelids not only causes an aesthetic defect, but can also impair vision. In a pronounced form, severe ophthalmological diseases can develop.
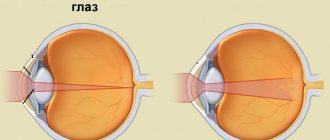
The muscle is attached to the orbit of the superior cartilage. The beginning is the area of the optic opening. It passes into a tendon, the width of which is much greater. Its anterior part is attached to the cartilage and goes to the orbicularis muscle. The fibers, which are located on the back, connect to the conjunctiva and pass into the upper fold.
The fibers located on the middle part of the tendon complete the structure of the muscle. The muscle that raises the eyelid is closely related to the levator muscle. It is located near its front end. In addition, this structure ensures the elevation of not only the eyelid, but also all its parts: cartilage, skin, conjunctiva, which passes into the upper fold.
The innervation of the middle part of the upper eyelid has smooth fibers. Therefore it is considered a sympathetic nerve. The posterior surface is completely covered with conjunctiva connected to cartilage. If the levator tone is normal, then the upper eyelid covers the cornea by about 2 mm. The function that is responsible for raising it is impaired with ptosis.
This ligament passes under the oblique muscle at the back. It then mixes with the fascia and covers the area above the eye. From the outside it is attached to the capsule of the lacrimal gland. The main function limits muscle displacement on the posterior side. This theory is confirmed by the localization of such functionality. When tense, the ligament supports the upper eyelid. If this function is not performed, ptosis will appear.
Causes of wrinkles, drooping eyelids, sunken eyes and bruises under the eyes
It is generally accepted that with age, muscles weaken, losing their tone. In reality, everything happens the other way around. Age-related changes in the eyelids begin due to muscle hypertonicity.
A spasm often occurs in the orbicularis oculi muscle, causing it to decrease from above towards the inner corner, and from below towards the outer edge. Because of this, the skin that was previously stretched over the muscle becomes redundant and begins to sag.
Due to the habit of sleeping on the side, creases are formed that run from the outer corner of the eye to the nose. Changing your sleeping position can correct this problem.
Due to the work of the temporal muscle, crow's feet are formed during squinting and laughing. Also, the reason for their appearance is the drying out of the temporal region of the bone structure with age, due to which the muscle narrows, adapting to the changes in the bone, and the skin folds into folds.
Due to poor lymphatic drainage in the body and deformation of bone and muscle structures, excess fluid begins to accumulate between the skin of the eyelids and the muscles. This is manifested by swelling of the upper eyelid, its overhang, and bags under the eyes.
Drooping of the upper eyelid is also associated with deformation of the orbicularis oculi, frontal and temporal muscles, since these muscles are interconnected.
Deformed muscles in the forehead point downward, causing the skin to sag over the eyes.
A spasmed temporalis muscle causes the skin to sag at the outer corner of the eye, and the skin under the inner part of the eyebrow begins to sag due to hypertonicity of the corrugator muscle.
Why do eyes become smaller, sunken and hollow with age?
Often, due to spasm and narrowing of the orbicularis oculi muscle, with age the eyelids become smaller in size and seem to sink in, their shape changes.
Let us note that such changes are associated, among other things, with psychological aging, when a person loses interest in life, stops looking at everything with wide open eyes, and his eyelids narrow.
When the eyes sink, a protrusion appears under the eyelid in the shape of a “step” - this phenomenon is called “deepening of the tear trough.” It is formed at the junction of the orbicularis eyelid muscle with other facial muscles. In this place, blood circulation deteriorates, and a pronounced darkening appears.
Since with age, most of the muscles on the face are in hypertonicity, the deformed lateral nasal muscle, the muscle that lifts the upper lip and the wing of the nose, increase the manifestations of the tear trough and bruises under the eyes due to the fact that the area of the lateral part of the nose becomes shorter, approaching century. Due to poor blood circulation, the amount of fatty tissue in this area increases, a bulge forms, and the eye appears more sunken.
A block of the orbicularis muscle and other muscles adjacent to it impedes blood circulation in the eye area and lymph outflow. The tissues receive poor nutrients and waste from stagnant lymph poisons them, the color and structure of the skin changes, it becomes thin with a blue tint.
Innervation of the eye
Description
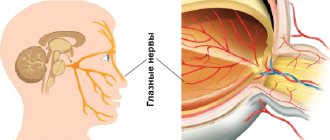
Sensitive innervation of the eye and orbital tissues is carried out by the first branch of the trigeminal nerve - the orbital nerve, which enters the orbit through the superior orbital fissure and is divided into 3 branches: lacrimal, nasociliary and frontal.
The lacrimal nerve innervates the lacrimal gland, the outer parts of the conjunctiva of the eyelids and eyeball, and the skin of the lower and upper eyelids.
The nasociliary nerve gives off a branch to the ciliary ganglion, 3-4 long ciliary branches go to the eyeball, in the suprachoroidal space near the ciliary body they form a dense plexus, the branches of which penetrate the cornea. At the edge of the cornea, they enter the middle sections of its own substance, losing their myelin coating. Here the nerves form the main plexus of the cornea. Its branches under the anterior border plate (Bowman's) form one plexus of the “closing chain” type. The stems coming from here, piercing the border plate, fold on its anterior surface into the so-called subepithelial plexus, from which branches extend, ending with terminal sensory devices directly in the epithelium.
The frontal nerve is divided into two branches: supraorbital and supratrochlear. All branches, anastomosing among themselves, innervate the middle and inner part of the skin of the upper eyelid.
Ciliary
, or
ciliary
, node is located in the orbit on the outside of the optic nerve at a distance of 10-12 mm from the posterior pole of the eye. Sometimes there are 3-4 nodes around the optic nerve. The ciliary ganglion includes sensory fibers of the nasopharynx nerve, parasympathetic fibers of the oculomotor nerve and sympathetic fibers of the plexus of the internal carotid artery.
4-6 short ciliary nerves depart from the ciliary ganglion, penetrating the eyeball through the posterior part of the sclera and supplying the eye tissue with sensitive parasympathetic and sympathetic fibers. Parasympathetic fibers innervate the sphincter of the pupil and the ciliary muscle. Sympathetic fibers go to the dilator muscle.
The oculomotor nerve innervates all the rectus muscles except the external one, as well as the inferior oblique, levator superior pallidum, sphincter pupillary muscle, and ciliary muscle.
The trochlear nerve innervates the superior oblique muscle, and the abducens nerve innervates the external rectus muscle.
The orbicularis oculi muscle is innervated by a branch of the facial nerve.
Adnexa of the eye
The appendage apparatus of the eye includes the eyelids, conjunctiva, tear-producing and tear-draining organs, and retrobulbar tissue.
Eyelids (palpebrae)
The main function of the eyelids is protective. The eyelids are a complex anatomical formation that includes two layers - musculocutaneous and conjunctival-cartilaginous.
The skin of the eyelids is thin and very mobile, freely gathers into folds when opening the eyelids and also freely straightens when they close. Due to mobility, the skin can easily be pulled to the sides (for example, by scars, causing eversion or inversion of the eyelids). The displaceability, mobility of the skin, the ability to stretch and move are used in plastic surgery.
Subcutaneous tissue is represented by a thin and loose layer, poor in fatty inclusions. As a result, severe swelling easily occurs here due to local inflammatory processes, and hemorrhages due to injuries. When examining a wound, it is necessary to remember about the mobility of the skin and the possibility of large displacement of the wounding object in the subcutaneous tissue.
The muscular part of the eyelid consists of the orbicularis palpebral muscle, the levator palpebrae superioris, the Riolan muscle (a narrow strip of muscle along the edge of the eyelid at the root of the eyelashes) and the Horner muscle (muscle fibers from the orbicularis muscle that surround the lacrimal sac).
The orbicularis oculi muscle consists of the palpebral and orbital bundles. The fibers of both bundles begin from the internal ligament of the eyelids - a powerful fibrous horizontal cord, which forms the periosteum of the frontal process of the upper jaw. The fibers of the palpebral and orbital parts run in arcuate rows. The fibers of the orbital part in the area of the outer corner pass to the other eyelid and form a complete circle. The orbicularis muscle is innervated by the facial nerve.
The muscle that lifts the upper eyelid consists of 3 parts: the anterior part is attached to the skin, the middle part is attached to the upper edge of the cartilage, and the posterior part is attached to the upper fornix of the conjunctiva. This structure ensures the simultaneous lifting of all layers of the eyelids. The anterior and posterior parts of the muscle are innervated by the oculomotor nerve, the middle by the cervical sympathetic nerve.
Behind the orbicularis oculi muscle is a dense connective tissue plate called eyelid cartilage, although it does not contain cartilage cells. The cartilage gives the eyelids a slight bulge that follows the shape of the eyeball. The cartilage is connected to the edge of the orbit by a dense tarso-orbital fascia, which serves as the topographic boundary of the orbit. The contents of the orbit include everything that lies behind the fascia.
In the thickness of the cartilage, perpendicular to the edge of the eyelids, there are modified sebaceous glands - meibomian glands. Their excretory ducts exit into the intermarginal space and are located along the posterior edge of the eyelids. The secretion of the meibomian glands prevents the overflow of tears over the edges of the eyelids, forms a lacrimal stream and directs it into the lacrimal lake, protects the skin from maceration, and is part of the precorneal film that protects the cornea from drying out. The blood supply to the eyelids is carried out from the temporal side by branches from the lacrimal artery, and from the nasal side - from the ethmoid artery. Both are terminal branches of the ophthalmic artery. The greatest accumulation of eyelid vessels is located 2 mm from its edge. This must be taken into account during surgical interventions and injuries, as well as the location of the muscle bundles of the eyelids. Considering the high displacement capacity of eyelid tissues, minimal removal of damaged areas during primary surgical treatment is desirable.
The outflow of venous blood from the eyelids goes to the superior ophthalmic vein, which has no valves and anastomoses through the angular vein with the cutaneous veins of the face, as well as with the veins of the sinuses and pterygopalatine fossa. The superior orbital vein leaves the orbit through the superior orbital fissure and flows into the cavernous sinus. Thus, an infection from the skin of the face and sinuses can quickly spread to the orbit and into the cavernous sinus.
The regional lymph node of the upper eyelid is the predural lymph node, and the lower one is the submandibular lymph node. This must be taken into account during the spread of infection and metastasis of tumors.
Conjunctiva
The conjunctiva is the thin mucous membrane that lines the back surface of the eyelids and the front surface of the eyeball up to the cornea. The conjunctiva is a mucous membrane richly supplied with blood vessels and nerves. She easily responds to any irritation.
The conjunctiva forms a slit-like cavity (bag) between the eyelid and the eye, which contains the capillary layer of tear fluid.
In the medial direction, the conjunctival sac reaches the inner corner of the eye, where the lacrimal caruncle and the semilunar fold of the conjunctiva (vestigial third eyelid) are located. Laterally, the border of the conjunctival sac extends beyond the outer corner of the eyelids. The conjunctiva performs protective, moisturizing, trophic and barrier functions.
There are 3 sections of the conjunctiva: the conjunctiva of the eyelids, the conjunctiva of the fornix (upper and lower) and the conjunctiva of the eyeball.
The conjunctiva is a thin and delicate mucous membrane, consisting of a superficial epithelial and deep submucosal layer. The deep layer of the conjunctiva contains lymphoid elements and various glands, including lacrimal glands, which provide mucin and lipids for the superficial tear film covering the cornea. The accessory lacrimal glands of Krause are located in the conjunctiva of the superior fornix. They are responsible for the constant production of tear fluid under normal, non-extreme conditions. Glandular formations can become inflamed, which is accompanied by hyperplasia of lymphoid elements, an increase in glandular discharge and other phenomena (folliculosis, follicular conjunctivitis).
The conjunctiva of the eyelids (tun. conjunctiva palpebrarum) is moist, pale pinkish in color, but quite transparent, through it you can see the translucent glands of the cartilage of the eyelids (meibomian glands). The surface layer of the conjunctiva of the eyelid is lined with multirow columnar epithelium, which contains a large number of goblet cells that produce mucus. Under normal physiological conditions there is little of this mucus. Goblet cells respond to inflammation by increasing their numbers and increasing secretion. When the conjunctiva of the eyelid becomes infected, the goblet cell discharge becomes mucopurulent or even purulent.
In the first years of life in children, the conjunctiva of the eyelids is smooth due to the absence of adenoid formations here. With age, you observe the formation of focal accumulations of cellular elements in the form of follicles, which determine special forms of follicular lesions of the conjunctiva.
An increase in glandular tissue predisposes to the appearance of folds, depressions and elevations that complicate the surface relief of the conjunctiva, closer to its arches; in the direction of the free edge of the eyelids, the folding is smoothed out.
Conjunctiva of the fornix. In the fornix (fornix conjunctivae), where the conjunctiva of the eyelids passes into the conjunctiva of the eyeball, the epithelium changes from multilayered cylindrical to multilayered flat.
Compared to other sections in the vault area, the deep layer of the conjunctiva is more pronounced. Numerous glandular formations are well developed here, including small additional lacrimal jelly (Krause's glands).
Under the transitional folds of the conjunctiva there is a pronounced layer of loose fiber. This circumstance determines the ability of the conjunctiva of the fornix to easily fold and straighten, which allows the eyeball to maintain full mobility.
Cicatricial changes in the conjunctival fornix limit eye movements. Loose fiber under the conjunctiva contributes to the formation of edema here during inflammatory processes or congestive vascular phenomena. The upper conjunctival fornix is wider than the lower one. The depth of the first is 10-11 mm, and the second - 7-8 mm. Typically, the superior fornix of the conjunctiva extends beyond the superior orbitopalpebral groove, and the inferior fornix is at the level of the inferior orbitopalpebral fold. In the upper outer part of the upper fornix, pinholes are visible, these are the mouths of the excretory ducts of the lacrimal gland
Conjunctiva of the eyeball (conjunctiva bulbi).
It distinguishes between a movable part, covering the eyeball itself, and a part of the limbus region, fused to the underlying tissue. From the limbus, the conjunctiva passes to the anterior surface of the cornea, forming its epithelial, optically completely transparent layer.
The genetic and morphological similarity of the epithelium of the conjunctiva of the sclera and cornea determines the possibility of the transition of pathological processes from one part to another. This occurs with trachoma even in its initial stages, which is essential for diagnosis.
In the conjunctiva of the eyeball, the adenoid apparatus of the deep layer is poorly represented; it is completely absent in the cornea area. The stratified squamous epithelium of the conjunctiva of the eyeball is non-keratinizing and under normal physiological conditions retains this property. The conjunctiva of the eyeball is much more abundant than the conjunctiva of the eyelids and fornix, equipped with sensitive nerve endings (the first and second branches of the trigeminal nerve). In this regard, the entry of even small foreign bodies or chemicals into the conjunctival sac causes a very unpleasant sensation. It is more significant with inflammation of the conjunctiva.
The conjunctiva of the eyeball is not connected to the underlying tissues in the same way everywhere. Along the periphery, especially in the upper outer part of the eye, the conjunctiva lies on a layer of loose tissue and here it can be freely moved with an instrument. This circumstance is used when performing plastic surgeries when moving sections of the conjunctiva is required.
Along the perimeter of the limbus, the conjunctiva is fixed quite firmly, as a result of which, with significant swelling, a vitreous shaft is formed in this place, sometimes hanging over the edges of the cornea.
The vascular system of the conjunctiva is part of the general circulatory system of the eyelids and eyes. The main vascular distributions are located in its deep layer and are represented mainly by links of the microcircular network. Many intramural blood vessels of the conjunctiva ensure the vital activity of all its structural components.
By changing the pattern of blood vessels in certain areas of the conjunctiva (conjunctival, pericorneal and other types of vascular injections), differential diagnosis of diseases associated with the pathology of the eyeball itself and diseases of purely conjunctival origin is possible.
The conjunctiva of the eyelids and eyeball is supplied with blood from the arterial arches of the upper and lower eyelids and from the anterior ciliary arteries. The arterial arches of the eyelids are formed from the lacrimal and anterior ethmoidal arteries. The anterior ciliary vessels are branches of the muscular arteries that supply blood to the external muscles of the eyeball. Each muscular artery gives off two anterior ciliary arteries. An exception is the artery of the external rectus muscle, which gives off only one anterior ciliary artery.
These vessels of the conjunctiva, the source of which is the ophthalmic artery, belong to the system of the internal carotid artery. However, the lateral arteries of the eyelids, from which branches supplying part of the conjunctiva of the eyeball arise, anastomose with the superficial temporal artery, which is a branch of the external carotid artery.
The blood supply to most of the conjunctiva of the eyeball is carried out by branches originating from the arterial arches of the upper and lower eyelids. These arterial branches and the accompanying veins form conjunctival vessels, which in the form of numerous stems go to the conjunctiva of the sclera from both anterior folds. The anterior ciliary arteries of the scleral tissue run above the area of attachment of the rectus tendons towards the limbus. 3-4 mm from it, the anterior ciliary arteries are divided into superficial and perforating branches, which penetrate through the sclera into the eye, where they participate in the formation of the large arterial circle of the iris.
The superficial (recurrent) branches of the anterior ciliary arteries and the accompanying venous trunks are the anterior conjunctival vessels. The superficial branches of the conjunctival vessels and the posterior conjunctival vessels anastomosing with them form the superficial (subepithelial) body of the vessels of the conjunctiva of the eyeball. This layer contains the greatest number of elements of the microcircular bed of the bulbar conjunctiva.
The branches of the anterior ciliary arteries, anastomosing with each other, as well as the tributaries of the anterior ciliary veins form the marginal circumference of the limbus, or the perilimbal vascular network of the cornea.
Lacrimal organs
The lacrimal organs consist of two separate topographically distinct departments, namely the tear-producing and lacrimal-discharge parts. The tear performs protective (washes away foreign elements from the conjunctival sac), trophic (nourishes the cornea, which does not have its own vessels), bactericidal (contains nonspecific immune defense factors - lysozyme, albumin, lactoferin, b-lysine, interferon), moisturizing functions (especially the cornea , maintaining its transparency and being part of the precorneal film).
Tear-producing organs.
Lacrimal gland (glandula lacrimalis)
in its anatomical structure it is very similar to the salivary glands and consists of many tubular glands, collected in 25-40 relatively separate lobules. The lacrimal gland, by the lateral portion of the aponeurosis of the muscle that lifts the upper eyelid, is divided into two unequal parts, the orbital and palpebral, which communicate with each other by a narrow isthmus.
The orbital part of the lacrimal gland (pars orbitalis) is located in the upper outer part of the orbit along its edge. Its length is 20-25 mm, diameter is 12-14 mm and thickness is about 5 mm. In shape and size, it resembles a bean, which is adjacent with its convex surface to the periosteum of the lacrimal fossa. The gland is covered in front by the tarso-orbital fascia, and in the back it is in contact with the orbital tissue. The gland is held in place by connective tissue cords stretched between the gland capsule and the periorbita.
The orbital part of the gland is usually not palpable through the skin, since it is located behind the bony edge of the orbit that hangs here. When the gland enlarges (for example, tumor, swelling or prolapse), palpation becomes possible. The lower surface of the orbital part of the gland faces the aponeurosis of the muscle that lifts the upper eyelid. The consistency of the gland is soft, the color is grayish-red. The lobes of the anterior part of the gland are closed more tightly than in its posterior part, where they are loosened by fatty inclusions.
3-5 excretory ducts of the orbital part of the lacrimal gland pass through the substance of the inferior lacrimal gland, receiving part of its excretory ducts.
Palpebral or secular part
The lacrimal gland is located somewhat anteriorly and below the superior lacrimal gland, directly above the superior fornix of the conjunctiva. When the upper eyelid is inverted and the eye is turned inward and downward, the lower lacrimal gland is normally visible in the form of a slight protrusion of a yellowish tuberous mass. In the case of inflammation of the gland (dacryoadenitis), a more pronounced bulge is found in this place due to swelling and compaction of the glandular tissue. The increase in the mass of the lacrimal gland can be so significant that it sweeps away the eyeball.
The lower lacrimal gland is 2-2.5 times smaller than the upper lacrimal gland. Its longitudinal size is 9-10 mm, transverse - 7-8 mm and thickness - 2-3 mm. The anterior edge of the inferior lacrimal gland is covered with conjunctiva and can be palpated here.
The lobules of the lower lacrimal gland are loosely connected to each other, its ducts partly merge with the ducts of the upper lacrimal gland, some open into the conjunctival sac independently. Thus, there are a total of 10-15 excretory ducts of the upper and lower lacrimal glands.
The excretory ducts of both lacrimal glands are concentrated in one small area. Scar changes in the conjunctiva in this place (for example, with trachoma) may be accompanied by obliteration of the ducts and lead to a decrease in the lacrimal fluid secreted into the conjunctival sac. The lacrimal gland comes into action only in special cases when a lot of tears are needed (emotions, foreign agents entering the eye).
accessory lacrimal glands produce 0.4-1.0 ml of tears to perform all functions.
Krause (20 to 40) and Wolfring (3-4), embedded in the thickness of the conjunctiva, especially along its upper transitional fold. During sleep, tear secretion slows down sharply. Small conjunctival lacrimal glands, located in the boulevard conjunctiva, provide the production of mucin and lipids necessary for the formation of the precorneal tear film.
Tear is a sterile, clear, slightly alkaline (pH 7.0-7.4) and somewhat opalescent liquid, consisting of 99% water and approximately 1% organic and inorganic parts (mainly sodium chloride, but also sodium carbonates and magnesium, calcium sulfate and phosphate).
With various emotional manifestations, the lacrimal glands, receiving additional nerve impulses, produce excess fluid that flows from the eyelids in the form of tears. There are persistent disturbances in tear secretion towards hyper- or, conversely, hyposecretion, which is often a consequence of pathology of nerve conduction or excitability. Thus, tear production decreases with paralysis of the facial nerve (VII pair), especially with damage to its geniculate ganglion; trigeminal nerve palsy (V pair), as well as in some poisonings and severe infectious diseases with high fever. Chemical, painful temperature irritations of the first and second branches of the trigeminal nerve or zones of its innervation - the conjunctiva, the anterior parts of the eye, the mucous membrane of the nasal cavity, and the dura mater are accompanied by profuse lacrimation.
The lacrimal glands have sensitive and secretory (vegetative) innervation. General sensitivity of the lacrimal glands (provided by the lacrimal nerve from the first branch of the trigeminal nerve). Secretory parasympathetic impulses are delivered to the lacrimal glands by fibers of the intermediate nerve (n. intermedrus), which is part of the facial nerve. Sympathetic fibers to the lacrimal gland originate from the cells of the superior cervical sympathetic ganglion.
Lacrimal ducts.
They are designed to drain tear fluid from the conjunctival sac. Tear as an organic liquid ensures the normal vital activity and function of the anatomical formations that make up the conjunctival cavity. The excretory ducts of the main lacrimal glands open, as mentioned above, into the lateral section of the upper fornix of the conjunctiva, which creates a semblance of a lacrimal “shower”. From here, the tear spreads throughout the conjunctival sac. The posterior surface of the eyelids and the anterior surface of the cornea limit the capillary fissure - the lacrimal stream (rivus lacrimalis). By moving the eyelids, the tear moves along the tear stream towards the inner corner of the eye. Here is the so-called lacrimal lake (lacus lacrimalis), limited by the medial areas of the eyelids and the semilunar fold.
The lacrimal ducts themselves include lacrimal openings (punctum lacrimale), lacrimal canaliculi (canaliculi lacrimales), lacrimal sac (saccus lacrimalis), and nasolacrimal duct (ductus nasolacrimalis).
Lacrimal puncta
(punctum lacrimale) are the initial openings of the entire lacrimal apparatus. Their normal diameter is about 0.3 mm. The lacrimal puncta are located at the top of small conical projections called lacrimal papillae (papilla lacrimalis). The latter are located on the posterior ribs of the free edge of both eyelids, the upper one is approximately 6 mm, and the lower one is 7 mm from their internal commissure.
The lacrimal papillae face the eyeball and are almost adjacent to it, while the lacrimal puncta are immersed in the lacrimal lake, at the bottom of which lies the lacrimal caruncle (caruncula lacrimalis). Close contact of the eyelids, and therefore the lacrimal openings with the eyeball, is facilitated by constant tension of the tarsal muscle, especially its medial sections.
The holes located at the top of the lacrimal papillae lead into the corresponding thin tubes - the upper and lower lacrimal canaliculi
. They are located entirely in the thickness of the eyelids. In direction, each tubule is divided into a short oblique vertical and a longer horizontal part. The length of the vertical sections of the lacrimal canaliculi does not exceed 1.5-2 mm. They run perpendicular to the edges of the eyelids, and then the tear ducts turn towards the nose, taking a horizontal direction. The horizontal sections of the tubules are 6-7 mm long. The lumen of the lacrimal canaliculi is not the same throughout. They are somewhat narrowed in the bending area and ampullarly widened at the beginning of the horizontal section. Like many other tubular formations, the lacrimal canaliculi have a three-layer structure. The outer, adventitial membrane is composed of delicate, thin collagen and elastic fibers. The middle muscular layer is represented by a loose layer of bundles of smooth muscle cells, which apparently play a certain role in regulating the lumen of the tubules. The mucous membrane, like the conjunctiva, is lined with columnar epithelium. This arrangement of the lacrimal canaliculi allows them to stretch (for example, under mechanical stress - the introduction of conical probes).
The terminal sections of the lacrimal canaliculi, each individually or merging with each other, open into the upper section of a wider reservoir - the lacrimal sac. The mouths of the lacrimal canaliculi usually lie at the level of the medial commissure of the eyelids.
Lacrimal sac
(saccus lacrimale) makes up the upper, expanded part of the nasolacrimal duct. Topographically, it relates to the orbit and is located in its medial wall in the bone recess - the fossa of the lacrimal sac. The lacrimal sac is a membranous tube 10-12 mm long and 2-3 mm wide. Its upper end ends blindly; this place is called the vault of the lacrimal sac. In the downward direction, the lacrimal sac narrows and passes into the nasolacrimal duct. The wall of the lacrimal sac is thin and consists of a mucous membrane and a submucosal layer of loose connective tissue. The inner surface of the mucous membrane is lined with multirow columnar epithelium with a small number of mucous glands.
The lacrimal sac is located in a kind of triangular space formed by various connective tissue structures. The sac is limited medially by the periosteum of the lacrimal fossa, covered in front by the internal ligament of the eyelids and the tarsal muscle attached to it. The tarso-orbital fascia runs behind the lacrimal sac, as a result of which it is believed that the lacrimal sac is located preseptally, in front of the septum orbitale, i.e., outside the orbital cavity. In this regard, purulent processes of the lacrimal sac extremely rarely give complications to the tissues of the orbit, since the sac is separated from its contents by a dense fascial septum - a natural obstacle to infection.
In the area of the lacrimal sac, under the skin of the internal angle, there passes a large and functionally important vessel - the angular artery (a.angularis). It is the connecting link between the systems of the external and internal carotid arteries. The angular vein is formed at the inner corner of the eye, which then continues into the facial vein.
Nasolacrimal duct
(ductus nasolacrimalis) is a natural continuation of the lacrimal sac. Its length is on average 12-15 mm, width 4 mm, the duct is located in the bone canal of the same name. The general direction of the channel is from top to bottom, from front to back, from outside to inside. The course of the nasolacrimal duct varies somewhat depending on the width of the back of the nose and the pyriform opening of the skull.
Between the wall of the nasolacrimal duct and the periosteum of the bony canal there is a densely branched network of venous vessels, this is a continuation of the cavernous tissue of the inferior turbinate. Venous formations are especially developed around the mouth of the duct. Increased blood filling of these vessels as a result of inflammation of the nasal mucosa causes temporary compression of the duct and its outlet, which prevents tears from moving into the nose. This phenomenon is well known to everyone as lacrimation during an acute runny nose.
The mucous membrane of the duct is lined with two-layer columnar epithelium; small branched tubular glands are found here. Inflammatory processes and ulceration of the mucous membrane of the nasolacrimal duct can lead to scarring and its persistent narrowing.
The lumen of the outlet end of the nasolacrimal duct has a slit-like shape: its opening is located in the front part of the lower nasal meatus, 3-3.5 cm away from the entrance to the nose. Above this opening there is a special fold called the lacrimal fold, which represents a duplication of the mucous membrane and prevents the reverse flow of tear fluid.
In the prenatal period, the mouth of the nasolacrimal duct is closed by a connective tissue membrane, which resolves by the time of birth. However, in some cases, this membrane may persist, which requires urgent measures to remove it. Delay threatens the development of dacryocystitis.
The tear fluid, irrigating the front surface of the eye, partially evaporates from it, and the excess collects in the tear lake. The mechanism of tear production is closely related to the blinking movements of the eyelids. The main role in this process is attributed to the pump-like action of the lacrimal canaliculi, the capillary lumen of which, under the influence of the tone of their intramural muscular layer associated with the opening of the eyelids, expands and sucks in fluid from the lacrimal lake. When the eyelids close, the canaliculi are compressed and the tear is squeezed into the lacrimal sac. Of no small importance is the suction effect of the lacrimal sac itself, which during blinking movements alternately expands and contracts due to the traction of the medial ligament of the eyelids and the contraction of part of their circular muscle, known as Horner’s muscle. Further outflow of tears along the nasolacrimal duct occurs as a result of the expelling action of the lacrimal sac, and also partly under the influence of gravity.
The passage of tear fluid through the lacrimal ducts under normal conditions lasts about 10 minutes. Approximately this amount of time is required for (3% collargol, or 1% fluorecein) from the lacrimal lake to reach the lacrimal sac (5 minutes - canalicular test) and then the nasal cavity (5 minutes - positive nasal test).
—
Article from the book: Clinical lectures on ophthalmology | S. N. Basinsky, E. A. Egorov