Tuesday, November 26, 2019
Stress urinary incontinence is a disease that affects predominantly the female population, although men are no exception. The problem brings discomfort, inconvenience, disrupts the usual rhythm of life and reduces self-esteem. The quality of life is significantly reduced.
Medical statistics claim that at the age of 20-50 years, approximately 35% of European women suffer from this disease. With age, rates increase to 50%.
The scale of the disease among Russian women is even more impressive. After 40 years, out of 10 female representatives, every fourth suffers.
The official introduction of diagnosis into medicine occurred less than a century ago. The term has been established in the international statistical classification of diseases and health-related problems (stress urinary incontinence code according to ICD 10).
Until this time, the involuntary release of urine was considered an irreversible process of aging of the body. This opinion still exists, which reduces the number of people going to the hospital. This approach is fundamentally wrong. The disease is treatable and correctable.
There are several types of urinary incontinence: stress, urgency, mixed. Stress urinary incontinence is the most common. This is a disease associated with involuntary loss of urine. It is caused by dysfunction of the urethral sphincter or weakening of the pelvic floor muscles. As a result, urine is released every time the abdominal muscles tense. Can provoke:
- sneezing;
- laughter;
- hiccups and fright;
- vomit;
- cough;
- lifting weights;
- sudden change in body position;
- sexual intercourse;
- exercise stress.
The absence of a pain symptom prevents contacting a medical facility. Leveling the disease can worsen the situation, then radical methods of treatment become necessary. Therefore, it is necessary to contact a professional at the first manifestation of symptoms. Doctors will carefully approach the problem and offer an effective plan for getting rid of the pathology.
Highly qualified doctors at the Clinic for Men's and Women's Health in Moscow treat stress urinary incontinence using innovative methods using new equipment. Professionals have knowledge and experience in treating diseases of the reproductive and urinary system.
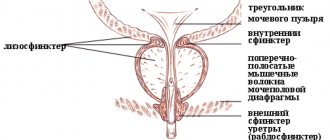
Causes of occurrence. Female predisposition
There are many common causes of stress urinary incontinence in women and men. Due to the anatomical difference in the structure of the genitourinary system, there are purely female reasons. The female urinary system is 3-5 cm in length, while the male one is 24-30 cm. Comparatively, the female canal is much thicker. Therefore, in women, the sphincter is less able to hold back pressure when exposed to pressure from urine or internal muscles. Physiological features are added by a smaller composition of collagen and elastic tissue.
Causes of stress urinary incontinence:
- physical labor associated with heavy lifting;
- genetic predisposition;
- traumatic birth, multiple or with multiple ruptures;
- inflammatory diseases of the pelvic organs;
- age-related changes (menopause, decrease in collagen in soft tissues);
- prolonged immobility (coma, surgery);
- psychophysical breakdown;
- injury to the central nervous system or spinal cord;
- excess weight;
- poor nutrition;
- diabetes;
- gout.
To find out how to treat stress urinary incontinence, it is imperative to consult a professional. At the “Men’s and Women’s Health Clinic”, certified urologists and urogynecologists will conduct a full cycle of diagnostic procedures to correctly determine the causes of the disease and prescribe the correct therapy.
2. Reasons
The main group of reasons consists of factors and conditions that weaken the muscular-ligamentous and sphincteric apparatus of the pelvic organs: difficult childbirth, especially repeated, intense physical activity due to professional specifics (especially if it involves constant lifting of weights), a tendency to constipation, some types of injury , incl. surgical (consequences of certain urological and/or gynecological surgical interventions), sexual excesses. Etiopathogenetic factors of NMPN include situations of chronic stress, menopause, pathology of the central and peripheral nervous system, and chronic urogenital infections.
The predisposing background is also the anatomy of the female urinary system - a short urethra of much larger diameter compared to the male one.
Visit our Urology page
When should you see a doctor? Symptoms of the disease
The main signal of the disease is the involuntary passage of urine naturally. The process occurs spontaneously, without urge, with the slightest tension in the abdominal muscles. Against this background, secondary symptoms may appear:
- unpleasant sensations in the pelvic area (pulling and aching);
- discomfort when urinating (stinging, itching, pain);
- irritation and swelling in the area of the external urinary organs;
- difficulties with defecation, etc.
The more symptoms appear, the more the problem gets worse. If you do not pay proper attention, the disease may progress to a stage where surgery for stress urinary incontinence is required.
Doctors at the Clinic for Men's and Women's Health are interested in offering clients the latest painless methods of treating genitourinary diseases. The work of the team of doctors is based on the European approach - maximum help with minimum discomfort.
Diagnostics and algorithm for correct medical treatment
Before starting treatment, the patient must undergo a set of diagnostic procedures. The information obtained will help the doctor determine the cause of the disease and prescribe a preliminary treatment plan.
A diagnosis of “stress urinary incontinence” can be made based on the results of diagnostic procedures:
- initial examination;
- studying the results of a urine test;
- electromyography of the pelvic muscles;
- uroflowmetry;
- maintaining a urination schedule.
The “Men's and Women's Health Clinic” has the latest diagnostic equipment and laboratory tools, with the help of which it is possible to accurately determine the cause and degree of development of stress urinary incontinence in men, women and children.
Features of the course of the disease
The disease has characteristics depending on the age and gender of the person suffering from the pathology. The features can be found in the table below.
Risk group | Features of the disease |
| Men | In representatives of the stronger sex, the disease occurs with similar symptoms. The treatment algorithm is established by the treating urologist. The range of methods used is from conservative to surgical intervention. The peculiarity of the course of the disease is caused by the presence of age-related ailments in the genital organs (prostate adenoma, cystitis, urethritis). |
| Women | The peculiarity of ICD 10 stress urinary incontinence in women is due to its close connection with the reproductive system, labor and hormonal levels. The doctor prescribes a urination plan, according to which the degree of development of the disease is determined and the necessary therapeutic measures are selected. The schedule should be followed for 3 months. Medication treatment for stress urinary incontinence, physiotherapy, exercise therapy, diet, and avoidance of physical activity are mandatory. |
| Children. | The release of urine in a child under 3 years of age may occur unconsciously. During this period, the regulation of urges has not yet been formed, so this is considered the norm. A wet bed at night for a child under 5 years of age may be caused by immaturity of the central nervous system or disease (enuresis). Therefore, you need to consult a doctor to determine the cause. After 6 years of age, stress urinary incontinence in children is subject to mandatory medical supervision. Stress urinary incontinence in a teenager can be caused by puberty, overstimulation of the central nervous system, or illness. Consultation with a doctor is essential. |
| Elderly people | Stress urinary incontinence in women aged 55 is caused by hormonal changes. Drug treatment and exercise therapy are carried out. In men over 60, the incidence is lower. A special feature is the lower effectiveness of treatment in later stages due to age-related changes. Therefore, it is recommended to immediately consult a doctor at the first symptoms. |
| Pregnant women | Particularly worrying is stress urinary incontinence after childbirth or during pregnancy. While carrying the fetus, pressure is exerted on the bladder, so urine leakage is not critical. It is recommended to empty it regularly to avoid unpleasant situations. Labor can injure the vagina, which plays a direct role in controlling urination. Therefore, if symptoms are observed during the postpartum period, consultation with a doctor is required. Tablets for stress urinary incontinence, exercises, and electromagnetic stimulation to strengthen the pelvic muscles may be prescribed. |
Thanks to the experience of the team at the Men's and Women's Health Clinic, patients of different age groups can receive appropriate care. Laser treatment for stress urinary incontinence is carried out here, which gives patients a minimum of discomfort and pain.
The range of pathologies that doctors struggle with is the widest in Moscow. Practicing in European and American clinics, doctors effectively treat stress urinary incontinence cystocele - downward prolapse of the vagina and bladder.
Urinary incontinence
Definition
Urinary incontinence is a disease characterized by involuntary loss of urine.
There are three types of urinary incontinence.
Stressful (SNM)
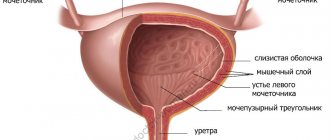
Stress urinary incontinence is an involuntary loss of urine caused by a defect in the ligamentous-fascial apparatus of the urethra.
Normally, the urethra is fixed (inactive) due to the ligament between it and the pubic bone and due to the fascial hammock, which is located under it.
For understanding, I will give a comparison. Imagine that the urethra is a hose for watering a vegetable garden, which lies on a path lined with stone tiles. The tile is a good ligamentous-fascial apparatus. Intra-abdominal pressure is the boot you stepped on the hose with. Water will not pass through the place where you stepped. Now place the hose on the garden bed. The loose soil of the bed is a poor ligamentous-fascial apparatus injured during childbirth. Water will easily pass through the place where you stepped, because... the hose will collapse under the pressure of your foot and will not be pinched.
Urgentnoye (UNM)
Urge urinary incontinence is the involuntary loss of urine due to the bladder becoming “overactive.”
This means that the bladder is more sensitive. There is an indomitable urge to urinate when there is a small amount of urine in the bladder. The bladder contracts prematurely, regardless of the woman's wishes. The cause of an urgent bladder may be a defect in its ligamentous-fascial apparatus (cystocele or uterine prolapse), inflammatory diseases of the bladder (cystitis, leukoplakia), organic damage to the bladder (tumor). If the doctor does not see any of the listed reasons, then we say that the cause of the urgency is unknown.
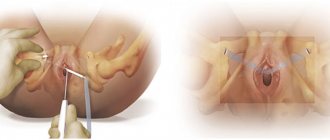
As a consequence of operations
A special form of urinary incontinence is urinary incontinence after surgery on the anterior vaginal wall. These are operations that were aimed at correcting her prolapse. Whether using synthetic prostheses (mesh), such as anterior prolift, Elevate, TVT-O or any others, or using your own tissue (anterior colporrhaphy). When fibrosis (overgrowth of connective tissue due to surgery) forms in the bladder neck area, the mobility of this area is lost. This zone seems to be constrained by fibrous tissue. To implement the mechanism of urinary retention, there must be mobility between the urethra and the bladder, like in a joint. If this mobility is not present, then the bladder and these organs resemble a bottle.
Symptoms
Stressful (SNM)
Involuntary loss of urine in small portions during physical activity (coughing, sneezing, laughing, jumping, lifting heavy objects). In severe forms, patients lose urine when walking or changing body position.
Urgentnoye (UNM)
- frequent urination (about 10 per day)
- night urination (more than two)
- a strong, uncontrollable urge to urinate (such patients live from toilet to toilet, when traveling they plan a route taking into account places where they can urinate)
- loss of urine when approaching the toilet, when running water, or when washing hands.
As a consequence of operations
The main symptom is loss of urine when the patient gets up and puts her feet down from the bed. In this case, urine pours out like water from an overturned bottle.
Treatment
Stressful (SNM)
- Treatment of mild forms: exercises to strengthen the muscles and ligaments of the pelvis.
- Surgical.
Urgentnoye (UNM)
Treatment of urge incontinence remains a big challenge because its cause is often unknown.
There is a misconception that overactive bladder needs to be treated only with medication.
If you go to the doctor complaining of a frequent, uncontrollable urge to urinate, tell him that you live from toilet to toilet, that traveling on public transport somewhere far away, going to the theater, to an exhibition, etc. has become a whole problem for you, then the doctor is 99% likely to prescribe you pills (Vesicar, etc.). Drug treatment is a burden. You must remember to take pills; medications have side effects (dry mucous membranes, rapid heartbeat, etc.), and treatment is expensive. Studies have shown that all patients stop drug treatment after a period of about a year and return to their previous state.
The cause of an overactive bladder, as I said above, may be prolapse of the anterior vaginal wall (cystocele) or prolapse of the uterus.
Here I will also make a comparison. Imagine a herniation on a car tire. This is a round protrusion. So, the same protrusion forms in the wall of the bladder when the anterior wall of the vagina or uterus prolapses. Bordering the anterior wall of the vagina is that part of the bladder wall where there are receptors (pressure-sensitive cells) responsible for the urge to urinate. When a hernia forms in the wall of the bladder, a small amount of urine entering this hernia affects the receptors and the urge to urinate occurs when there is a small amount of urine in the bladder.
If so, then you're in luck. You can get rid of trouble with a small operation and forget about pills. To make sure that a cystocele or uterine prolapse is the cause of urinary incontinence, you need to do a pessary test. The patient wears a rubber cube in her vagina and within a week understands whether there is an effect. If the pessary relieves the symptoms of hyperactivity, then the operation is highly likely to be successful.
If the test shows that the pessary does not help, then surgical treatment will not help. The choice will be drug treatment.
As a consequence of operations
Treatment of this form of UI is a very difficult task for a doctor. It is necessary to restore mobility in this area. This is at least two operations. The operations are reconstructive and plastic and are not always successful.
This disease corresponds to:
- Operations Urinary incontinence surgery
- Surgery complications
- Small pelvis
Effective ways to treat the disease
In the early stages, getting rid of the disease occurs without problems. Timely treatment means the fastest recovery and minimal medical intervention. Exercises against stress urinary incontinence can help in the early stages. A set of Kegel exercises is designed to strengthen the pelvic floor muscles.
Any treatment occurs only after the provoking factor has been eliminated.
The Clinic for Men's and Women's Health uses conservative and surgical treatment methods:
- drug treatment of stress urinary incontinence in women - antidepressants, estrogens, hormonal drugs, systemic HRT are prescribed.
- Biofeedback therapy – control of the pelvic floor muscles according to a schedule;
- laser treatment;
- shock wave therapy;
- tvt o surgery for stress urinary incontinence (prolene loop surgery);
- artificial sphincter implantation;
- bulinotherapy (introducing a gel to increase elasticity);
- urethrocystopexy.
Experts may recommend physiotherapy:
- warming up;
- electrophoresis.
Drugs for stress urinary incontinence are selected taking into account contraindications. The clinic’s doctors will study the disease in detail to prevent allergic reactions.
Laser treatment of stress urinary incontinence is recognized as one of the most effective techniques in the world. In our clinic, the treatment procedure takes place in 4-5 sessions.
Surgical treatment of stress urinary incontinence is prescribed only in extreme cases when conservative methods do not bring the desired result.
Highly qualified doctors will perform tvt o surgery for stress urinary incontinence. The intervention occurs with minimal tissue damage. The patient can leave the clinic the next day and wait for recovery at home.
In the clinic, patients are required to receive psychotherapeutic assistance in the treatment of delicate illnesses. A positive emotional background contributes to the patient’s recovery. Therefore, the time frame for complete recovery is reduced.
Treatment of stress urinary incontinence
Existing methods of treating incontinence are divided into conservative and surgical. The first include taking medications, Kegel exercises, and physiotherapy. The main goal of a set of therapeutic measures is to strengthen the pelvic floor muscles, and gymnastics, in the absence of contraindications, can provide real help. The essence of Kegel exercises comes down to contracting and relaxing the muscles responsible for urination. You can repeat the set of exercises three times during the day. Over time, the duration and level of stress increase.
Women can temporarily get rid of incontinence with the help of a special device - a pessary. A silicone or plastic device is inserted into the vagina to support the rectum, uterus and bladder. There are several types of devices, the choice of which depends on the doctor.
Drug treatment is not so effective, so it does not always help. It is possible to prescribe adrenergic agonists, antidepressants (if neurological causes of stress urinary incontinence are identified), anticholinergic drugs, nootropics, estrogens, and hormonal agents. Suppositories, ointments and creams are prescribed locally.
Physiotherapeutic procedures in the form of low-intensity currents improve the contractile functions of the pelvic muscles, which increases the chances of returning them to their previous abilities. The doctor may prescribe electrosleep, electrophoresis, magnetic therapy, Darsonval.
To reduce discomfort during the treatment period, it is worth purchasing urological pads or panties. The pads are attached to the laundry and can quickly absorb liquid and eliminate unpleasant odors. The product consists of several layers - a soft natural material is in contact with the skin, inside there is a special absorbent filler that does not let liquid out, and on the bottom there is a waterproof material. A special anatomical cut makes wearing urological underwear invisible, while ensuring the patient’s comfort when performing daily activities.
A wide variety of surgical techniques includes manipulations of varying degrees of complexity. Among them are sling operations, paraurethral injections, laparoscopic colposuspensions, and colporrhaphy. The doctor selects an option taking into account the degree of incontinence and the anatomical characteristics of the patient.
Traditional medicine in the fight against disease
Next to medical treatment, traditional medicine, which has more than one way to eliminate the disease, takes pride of place. You can check the effectiveness yourself.
Recipe 1. Pour 1 tsp. St. John's wort with a glass of hot water. Leave for 15-20 minutes. Defend. Drink twice a day.
Recipe 2. Pour a glass of boiling water over the dill seeds. Leave for 2 hours. Take a glass before meals.
Traditional methods can accompany medical prescriptions, since their effectiveness is low. Clinical recommendations for stress urinary incontinence should be followed. If you violate the doctor's recommendations, the problem can worsen.
Preventative ways to avoid stress urinary incontinence
The simplest method of treatment is to prevent the disease from taking over the body. Therefore, it is necessary to adhere to preventive measures. Especially women and individuals who have had the disease in previous generations.
Prevention:
- diet, weight control;
- smoking cessation, moderate exercise;
- strengthen muscles with special exercises for stress urinary incontinence in women;
- timely treat inflammatory processes of the internal organs of the small pelvis;
- empty your bowels on time.
At the Men's and Women's Health Clinic, patients receive qualified, timely care without queues or appointments. Experienced specialists will correctly diagnose and choose the right tactics to overcome the disease. Do not tolerate inconvenience and discomfort! Get effective help!
Symptoms of stress urinary incontinence
The main symptom of the problem is the random release of urine without objective reasons or urge. Often episodes of incontinence are associated with physical stress, even minor ones. The more advanced the pathology, the more noticeable the accompanying symptoms of stress urinary incontinence:
- the amount of fluid released increases from a couple of drops until the bladder is completely emptied;
- physical activity is more difficult to tolerate;
- It becomes less and less possible to control urinary retention;
- there is no strong urge to urinate.
The stress type of incontinence is diagnosed in 50% of cases and manifests itself when the peritoneum is tense. ICD-10 assigns pathology code R32. The generally accepted classification divides the disease into the following types:
- lung - urine leakage when coughing, hard work, physical exertion;
- average - urine is released when running, standing up suddenly, or walking;
- severe - leakage at rest.
Most often, able-bodied women 40–50 years old turn to doctors with this problem, which is due to hormonal instability and the peculiarities of the anatomical structure of the female body. Men suffer from pathology less often and usually seek help after the age of 70, when the pathology manifests itself due to the aging of the body.