Home / Welding technique
Back
Reading time: 3 min
0
1204
Electroophthalmia occurs when welding is carried out without taking into account safety regulations. This process can greatly damage your health.
Use special masks or goggles when there is a risk of damaging your eyes.
The disease can occur when you look at an ultraviolet spark without protection. In our article we will tell you what you can use at home to save yourself from burns.
- Is there really a problem?
- Immediate actions immediately after receiving a burn
- Therapy for electroophthalmia
- Conclusion
Types of welding eye drops
As a result of violation of safety precautions when welding on metal, a feeling appears as if sand was poured into the eye sockets, profuse lacrimation begins, and photophobia develops. Red or black dots from the burn may appear on the cornea, and the mucous membrane becomes very red. The eye is the most vulnerable organ, and it must be treated with care. When working with welding, you need to be aware of ultraviolet radiation, excessively bright light, infrared radiation, sparks emanating from the welding machine, fumes and harmful smoke.
If your eyes are damaged by welding, how to treat the disease? Therapy is prescribed by an ophthalmologist, since different drugs act on the mucous membrane of the eye in different ways, and in order not to worsen the situation and avoid allergic reactions of the cornea, it is better to see a doctor. There are the following types of eye drops for welding:
- pain relievers - analgesics;
- for the inflammatory process - antibiotics;
- vasoconstrictor drugs.
For inflammation of the conjunctiva, you can use some pharmaceutical products, but you should consult your doctor.
Welding eye drops that can be used before visiting a doctor:
- Visine. The product is intended to eliminate discomfort. It is used for redness, irritation, dryness of the cornea, burning, lacrimation, and a feeling of sand.
- Prokulin. The drug is used for non-infectious inflammation of the cornea and allergies.
- Visoptic - drops for irritation of the conjunctiva, itching, swelling, burning, lacrimation, redness of the cornea.
Prognosis and prevention
The consequences of electroophthalmia and the prognosis depend on the severity of the injuries and the timing of specialized care. The sooner the victim seeks help from a specialist, the greater the chance of a full recovery and restoration of vision. Even the most insignificant, at first glance, injury can lead to serious consequences in the future.
With a mild degree of damage, good and timely treatment, healing occurs within 3-4 days. The recovery process after degrees III-IV burns takes more than 3-4 months and requires observation by an ophthalmologist for at least 1 year after completion of treatment.
When working with welding, to avoid eye injury, you should:
- strictly follow all safety precautions;
- use personal protective equipment. A welding mask must be made of high-quality materials with a protection level of at least 13 DIN from infrared and ultraviolet radiation.
- Undergo preventive medical examinations for the purpose of early diagnosis. If changes are detected due to exposure to ultraviolet radiation, referral for inpatient treatment.
In rooms where welding work is carried out, all surfaces must be covered with oil paints, which contain zinc and iron oxide. These substances help absorb UV rays.
Welding arc radiation is very dangerous to the eyes.
Compliance with caution and safety rules will help not only prevent burns, but also avoid the harmful effects of medium and short waves of ultraviolet radiation. In order not to “catch bunnies”, do not look in the direction of welding work
The influence of welding on the organs of vision - systematization of knowledge
kluchnik wrote: Much worse than a welder breathing....
I think many people, both beginners and serious welders, will be interested in this article.
Compiled by: Chief freelance specialist-expert of the Main Directorate of Health Care of the Kurgan Region, chief occupational pathologist Marina Vasilievna Lukina.
Major occupational diseases
The main, most frequently developing occupational diseases of gas-electric welders include:
- Manganese toxicity (neurotoxicosis)
- Pneumoconiosis of electric welders
- Occupational eczema
- Dust bronchitis
- Bronchial asthma.
Manganese toxicity
Manganese is one of the neurotropic poisons that can cause the development of the most severe form of occupational neurotoxicosis. Manganese is a fragile metal, easily combines with oxygen, is soluble in acids, is of vital importance, is part of enzymes, is a cofactor for a number of enzymes, and is necessary for erythropoiesis, the synthesis of hemoglobin, ascorbic acid, glycogen, and the formation of cartilage tissue. Manganese accelerates the production of antibodies and the synthesis of vitamin C. It affects the activity of the pituitary gland and endocrine glands, the functioning of muscles and nerves. In industrial conditions, manganese is found in the form of dust, vapors, aerosols containing manganese oxides or salts. Manganese is part of high-quality electrodes used for welding, and during operation it is released into the environment as part of the welding aerosol. Thus, manganese in the form of an aerosol enters the body through the lungs, and to a lesser extent through the gastrointestinal tract and skin. Manganese is deposited in bones, brain and parenchymal organs. Blood normally contains 0.012 - 0.050 mg% manganese. Excretion occurs mainly in feces, less in urine, saliva, and breast milk. The maximum permissible concentration (MPC) of manganese in the air of the working area is 0.3 mg/m3 for disintegration aerosols and 0.05 mg/m3 for condensation aerosols. Manganese has a pronounced tropism for the subcortical nodes of the brain. It disrupts the exchange of biogenic amines and a number of enzymes, inhibits adrenergic and activates cholinergic systems, increases the content of acetylcholine in the synapses of the subcortical nodes and hypothalamus. But the main thing in its toxic effect is a violation of the synthesis and deposition of dopamine, an imbalance in the content of acetylcholine and dopamine, as a result of which muscle tone, accuracy, dexterity and smoothness of voluntary movements are disrupted, and autonomic disorders develop. Manganese also causes hypofunction of the endocrine glands, functional liver failure, vasomotor insufficiency, reduces blood supply to the brain (in the vertebrobasilar artery basin) and total cerebral blood flow. Manganese has an allergenic effect, so in addition to damaging the nervous system, it can cause bronchial asthma and eczema. When inhaling dust from manganese ores, the development of pneumoconiosis (manganoconiosis) is possible; when inhaling welding aerosol, dust bronchitis and pneumoconiosis of electric welders are possible. It should be noted that manganese does not cause acute poisoning; in industrial conditions, chronic manganese intoxication develops. Signs of intoxication develop slowly. In electric welders working with manganese-containing electrodes in closed containers and exposed to elevated concentrations of manganese in combination with carbon monoxide, the clinical picture of damage to the nervous system is characterized by asthenic, vegetative-vascular, and sometimes mild polyneuritic disorders. The severity of extrapyramidal disorders depends on the concentration of manganese oxides in the working area. The stage of functional impairment is characterized by general weakness, increased fatigue, decreased physical and mental performance, motor activity, and increased drowsiness. The range of interests narrows, complacency appears, and there is a lack of adequate assessment of the state of one’s health, which causes the patient to seek medical help later. The lack of specificity and bright clinic at this stage causes diagnostic difficulties. Objectively, the patient has mild muscle hypotonia, hyperhidrosis, hypomimia, pulse and blood pressure lability, and sensory disturbances. This is a mild degree of chronic manganese intoxication. In most cases, stabilization of the process is possible, less often - restoration of health. With continued contact with manganese, these manifestations are accompanied by signs of intellectual-mnestic disorders, extrapyramidal insufficiency (bradykinesia, moderate increase in muscle tone, coordination disorders), damage to peripheral nerves (distal polyneuritic type hypoesthesia). The changes are minor or irreversible, often progressive. This is the average severity of chronic manganese intoxication. Severe intoxication develops rarely and is characterized by the presence of akinetic-rigid or amyostatic syndrome or manganese parkinsonism. Manganese parkinsonism develops more often in short-term patients (from several months to 2-3 years) and is characterized by diffuse damage to the nervous system, motor and mental disorders. In addition to manganese parkinsonism, the development of toxic polyneuropathy with distal hypalgesia, decreased strength, muscle soreness on palpation, decreased potency in men, menstrual irregularities in women, and gastritis with reduced secretion is possible. It should be noted that many people who work for a long time in contact with manganese do not develop intoxication or, under the influence of carbon monoxide accompanying manganese, electrode combustion products, and metal aerosols, damage to other organs and systems develops. Obviously, this is due to the fact that manganese parkinsonism syndrome develops mainly in individuals with a genotypically determined increased vulnerability (inferiority) of the striopallidal system. As a result, a subclinical course of manganese intoxication is possible, which, under the influence of atherosclerosis, neurotrauma, neuroinfection, etc., acquires a clinical course in the form of manganese parkinsonism syndrome. It should be noted that the clinical manifestations of manganese intoxication continue to progress for many years after cessation of contact with it. Differential diagnosis at the stage of functional disorders is carried out with neuroses and neurosis-like conditions, polyneuropathies of diabetic, post-infectious, and alcoholic origin. In the stage of organic disorders (toxic encephalopathy) - with brain tumors, acute cerebrovascular accidents, post-infectious and post-traumatic encephalopathies, parasitic lesions of the brain. Treatment and further observation of the patient is in the professional center.
Pathology of the lungs and respiratory tract in electric welders
During the work associated with electric welding, a highly dispersed aerosol is formed, including dust of iron and other metals, as well as gases with toxic and irritating properties, and silicon dioxide. The composition and amount of highly dispersed dust generated depends on the type of welding, the composition of the welding materials and metals being welded, the mode of the welding process, etc. In addition to iron dust, and in some cases free silicon dioxide, welding aerosol may contain toxic substances - manganese oxides, chromium oxides , compounds of nickel, copper, zinc, vanadium and other metals, as well as nitrogen oxides, carbon monoxide, ozone, hydrogen fluoride, etc. If the welding aerosol contains a large amount of dust of iron oxides and silicon dioxide, then pneumoconiosis of electric welders is regarded as siderosilicosis. With a high content of free silicon dioxide in the aerosol, classical forms of silicosis can develop. There are known cases of manganoconiosis (pneumoconiosis from exposure to manganese dust) in electric welders using high-quality manganese-containing electrodes. When using electrodes with calcium fluoride coating, electric welders often experience acute respiratory diseases and pneumonia, which to a certain extent can be associated with the toxic effect of hydrogen fluoride formed during welding. Gas cutters who have contact with irritating and toxic gases are also prone to repeated pneumonia and frequent acute respiratory diseases. It is possible to develop acute lesions of the upper respiratory tract and lungs, including toxic pulmonary edema (hydrogen fluoride, nitrogen oxides, etc.), as well as foundry fever from exposure to condensation aerosols of zinc, copper, nickel and other metals. Thus, a highly dispersed welding aerosol of complex composition can have not only a fibrogenic, but also a toxic, irritating, and sensitizing effect. In this regard, electric welders and gas cutters, in addition to pneumoconiosis, may develop chronic bronchitis and bronchial asthma (from exposure to chromium, nickel and other compounds). Exposure to industrial dust among welders is often combined with exposure to unfavorable micro- and macroclimate factors, with a forced uncomfortable working posture, which accelerates the development of the pathological process and causes polymorphism of the clinical picture. Working in closed containers (tanks, tanks, etc.) also plays an important role, where in a confined space and in the absence of ventilation, the welder is forced to breathe air with a high concentration of welding aerosols. Welders do not use a respirator due to inconvenience (simultaneous use of a shield and a respirator is almost impossible), and enterprises are not provided with special hose gas masks with air supply. Pneumoconiosis, caused by exposure to dust released during welding and gas cutting, is characterized in most cases by a benign course. Typically, the coniotic process occurs 15 to 20 years after the start of work. In isolated cases, when welding work is carried out in closed containers, pneumoconiosis may develop earlier (after 5–6 years). Clinical manifestations of pneumoconiosis of electric welders, like many pneumoconiosis, are very scarce. Typically, patients complain of a dry cough or with a small amount of sputum, moderate shortness of breath during physical exertion, and sometimes chest pain. At the same time, physical examination data remain normal for a long time, indicators of external respiration function remain unchanged for a long time. Later, signs of pulmonary emphysema are detected, and respiratory function indicators slightly decrease, mainly in a restrictive manner. X-ray examination reveals diffuse enhancement and deformation of the vascular-bronchial pattern in the initial stage of pneumoconiosis. Against this background, clearly defined, round, nodule-like formations of the same shape and size are identified, which, as the disease progresses and with continued work under conditions of exposure to aerosol, fairly evenly dot both lung fields. These changes are caused mainly by the accumulation of radiopaque particles of metal dust. Unlike silicosis, there is no significant enlargement of the lymph nodes of the roots of the lungs, pneumofibrosis is weakly expressed, fibrous nodules characteristic of silicosis are not formed. Pneumoconiosis of electric welders is characterized, as a rule, by a benign course without progression of the process in the post-dust period. Its distinctive feature is the possibility of regression or reverse development of the pathological process after stopping work in contact with dust. The observed decrease in the number and size of nodule-like formations in the lungs is due to the fact that with this form of the coniotic process, the cellular reaction in the lungs prevails over the processes of fibrosis. In this regard, the reverse development of cellular dust foci is possible due to the elimination of radiopaque dust and the resorption of cell accumulations and young collagen fibers. Pneumoconiosis of electric welders is relatively rarely complicated by tuberculosis. Quite common complications are chronic bronchopulmonary infection with the symptom complex of bronchitis. Predispose to the development of this complication are acute poisonings with irritating and toxic gases or frequent acute respiratory diseases, under the guise of which mild, erased forms of the consequences of acute exposure to gases generated during welding and gas cutting of metals often occur. It is necessary to differentiate pneumoconiosis of electric welders from other diseases of the respiratory system, characterized by the development of pneumofibrosis and/or having a similar radiological picture: tuberculosis, sarcoidosis, pulmonary carcinomatosis, lymphogranulomatosis, diffuse fibrosing alveolitis, etc. In the treatment of pneumoconiosis, the emphasis is on etiological (cessation of contact with dust) and pathogenetic. The latter includes expectorants, mucolytics, vitamins, biogenic stimulants, and, according to indications, bronchodilators, inhaled corticosteroids. Physiotherapeutic treatment, exercise therapy, and sanatorium treatment show good results.
Prevention of occupational diseases of electric welders
- Improvement of technological processes.
- Regular use of personal protective equipment (for electric welders, these are hose gas masks, which provide the supply of air suitable for breathing from a clean area; there are also autonomous gas masks, which provide the supply of respiratory mixtures from an individual air supply source; filtering personal protective equipment for the respiratory system, gas-dust-proof).
- Availability, serviceability and regular use of collective protective equipment: local supply and exhaust ventilation and humidification of processed materials.
- High-quality pre-employment preventive medical examinations, the main purpose of which is to determine professional suitability for work in contact with welding aerosols. The main contraindications to admission are listed in the order of the Ministry of Health of the Russian Federation dated March 14, 1996 No. 90 “On the procedure for conducting preliminary and periodic medical examinations of workers and medical regulations for admission to the profession.”
- High-quality and regular conduct of periodic preventive medical examinations, the main purpose of which is to identify the initial signs of occupational diseases and the initial signs of general diseases that prevent continued work in contact with dust and welding aerosols.
- Improvement of health of persons who have contact with dust in a dispensary, boarding house, health troupe.
- Time protection (exclusion of excessively long work experience with welding aerosols and dust and exclusion of overtime work). The recommended maximum experience for electric welders is 12.5 years.
- Availability and regular use of paid breaks in addition to lunch to visit the inhaler. 9. Regular use of additional nutrition.
- To give up smoking.
Welding eye burn: first aid, treatment, drops, traditional medicine
> First aid >
07.11.2019
The welding profession is included in the group of dangerous and harmful to human health. However, eye burns from welding occur not only in production.
Now that purchasing your own welding machine is not a problem, you can “catch bunnies” anywhere. But regardless of where the injury occurred, the result is the same: in the late afternoon, the burned person literally washes himself with tears, household members have no idea about the causes of the strange symptom, and precious time is running out.
But in some cases, a minute of delay leads to irreversible impairment of visual functions
To save a victim from blindness, it is important to know the symptoms of an eye burn and the basic rules of first aid.
The main causes of eye burns from welding
Neglecting the rules for working with a welding machine can result in a burn to the cornea of the eye. Often the organs of vision are affected in the following cases:
- Assembling metal structures without the help of a partner and fasteners. Without wearing a mask, the welder holds the parts with his own hands and places tacks.
- Using a low-quality mask. Ultraviolet rays penetrate into the gaps between the filters and the mask frame.
- Using the wrong mask. To perform some tasks, an automatically darkening chameleon mask is required. In a mask with a regular shield, a worker simply will not have time to cover his face.
Presence during welding work (forced or accidental). The risk of injury increases on bright sunny days. Having succumbed to the deceptive sensation of the faint glow of the arc, a person loses his vigilance and by the evening he receives a full bouquet of burn symptoms.
What causes electroophthalmia?
Electrophthalmia is a burn of the eyes caused by welding, quartz or other powerful light source in medical language. The main cause of injury is the effect of ultraviolet rays on the mucous membrane, involving the cornea and retina.
The depth of damage depends on the scale of irradiation. A burn to the mucous membrane occurs when:
- a particle of hot metal or a spark gets into an unprotected eye;
- open contact with fumes of metals and gases;
- ultraviolet/infrared radiation;
- failure to comply with safety regulations (described above);
- exposure to thick toxic smoke (from a melted electrode) in the eye.
Symptoms of a welding burn
Immediately after a welding burn to the eyes, there are practically no symptoms. They grow within 6–12 hours. During this time, a person who has “picked up bunnies” can prepare everything necessary to provide first aid. If the burn is deep, it is better to see a specialist when the first symptoms appear.
Let's look at the general signs that help identify electroophthalmia:
- The first sign of a welding burn is a strong or mild burning sensation in the eyes, developing into a sharp pain. If you close your eyes tightly, it becomes easier. However, this is a deceptive feeling, because when you open your eyes, the pain returns.
- Tears constantly flow from the eyes, it hurts the victim to look at the light.
- With deep damage and involvement of the retina, a person sees nothing. However, there is no need to panic; in most cases, vision returns after 48 hours.
- When looking at the light, spots of light “stand” before the eyes. The duration of the symptom is determined by the duration of contact with the traumatic factor.
- You can feel the sand under your eyelids. Do not rub your eyes under any circumstances! This can accelerate the development of the inflammatory process and lead to swelling of injured tissues.
- The eye pain gradually spreads to the head, intensifying when you try to move your gaze to the side.
Signs of eye damage depend on the severity of the burns. In medicine there are:
- I degree (mild) – a burn of the cornea of the eye is expressed by decreased transparency, darkening of the cornea, and redness of the conjunctival membrane. In some cases, there is a slight burning sensation and itching. The victim can be helped at home.
- II degree (medium) – after an injury, the eye becomes covered with a film, the cornea is damaged, becomes loose and erosive. Victims experience photophobia and severe pain.
- III degree (severe) – visual functions sharply decrease, the eyelids swell, and severe aching pain occurs. There is a constant sensation of a foreign body under the eyelids (as if sand had been poured into the eyes). You cannot do without medical help.
- IV degree (extremely severe) – the injured tissue begins to die, the cornea becomes whitish, the victim screams in pain and cannot open his eyelids. Without timely medical assistance, a person becomes blind.
Symptoms of electroophthalmia
Clinical manifestations of electroophthalmia differ at different stages:
Signs of a mild eye burn (grade 1) are as follows:
- Itching on the inside of the eyelid;
- Redness of the mucous membrane;
- Burning sensation;
- Slight clouding of the cornea.
With a burn injury of 2nd severity, the following symptoms are observed:
- Damage to the epithelial layer of the cornea;
- Increased sensitivity of the eyes to light;
- The appearance of a film on the conjunctiva;
- From time to time there is pain when moving the eyes.
- White spots in the eyes;
Symptoms of eye burn 3rd degree of severity:
- Eyelids swell;
- A nagging pain appears;
- A sharp decrease in visual acuity;
- Severe clouding of the cornea;
- Sensation of a foreign body in the eye.
Signs of grade 4 burn injury:
- Necrosis of tissue of the damaged eye;
- Severe pain does not allow you to open your eyes;
- The cornea becomes faded and colorless;
- The cells of the conjunctival cavity begin to die;
- At the last stage, the risk of complete blindness increases.
First aid for retinal burns
The first symptoms begin to appear 4-5 (up to 9) hours after a UV burn. There is anxiety and a feeling of itching in the eyes. The eyelids become swollen and red. A person tends to rub his eyes and remove a non-existent foreign object from under his eyelids. Later, sharp pain appears when rotating the eyeball or opening the eyelids. More severe symptoms appear progressively.
When the first symptoms appear, you should immediately contact an ophthalmologist. If this is not possible, take emergency first aid measures yourself:
- Rinse eyes with cold bottled water or tea or chamomile infusion;
- Apply a cyproplegic drug to the eyes, for example: Cyclopentanol (1%) or Tropicamide (1%).
- Apply a pressure bandage or compress to the eyes with cold astringent solutions that accelerate epithelization: Artificial tears, Korneregel (Dexpatenol 0.5%), Actovegin or Solcoseryl (eye gel), Vitamin A (Retinol).
- To relieve severe pain symptoms, you can use pain-relieving eye drops: Lidocaine, Alcaine, Tetracaine, and take analgesics in tablets: Analgin, Ketanov, Nise, etc. You can use anti-inflammatory drugs: Diclofenac, Ketoprofen.
You should not put the first eye drops that come to hand into your eyes!
For example, anti-fatigue drops such as Albucid. They contain preservatives that inhibit regenerative (restorative) processes in the retina.
You should not use eye drops and ointments containing antibiotics on your own. They can smooth out the picture of more serious inflammatory eye diseases and complicate correct diagnosis.
What is prohibited in case of a corneal burn?
Patients with electroophthalmia are contraindicated:
- Rub your eyes. When a burn occurs, itching and discomfort appear in the eyes. Sometimes blepharospasm appears. Reflexively, the patient tries to feel better and begins to rub his eyes. This leads to damage to the surface of the cornea, so the pain syndrome only intensifies. The severity of the inflammatory response also increases.
- Unauthorized use of eye drops is prohibited, because most of them contain preservatives. These substances slow down regeneration processes and support inflammatory phenomena.
- It is not advisable to rinse your eyes with ordinary tap water, since it contains active ions (magnesium, calcium, chlorine) that have an irritating effect on the mucous membrane of the eye.
What happens to the eyes during welding and what are the consequences?
Welding is not only the joining of metal parts; it is also used when working with other materials. Electric current is used as a source of formation of the welding arc. So what exactly causes harm?
When welding, rays of three spectra are released at once: infrared, ultraviolet and light. The intensity is too high for the human eye, it exceeds the permissible level.
There is a common expression among welders: “catching a bunny.” This means that the cornea of the eye has been burned. We do not perceive infrared and ultraviolet rays with our eyes, but they have a very intense effect on the eyes. Moreover, negatively. Damaging the mucous membrane, retina and lens of the eye, causing a burn.
The main eye disease that occurs under the influence of light radiation from welding is electroophthalmia.
What other causes of eye damage from welding are there?
- Negligent attitude towards work. Often welders do not use special safety glasses, which are required to be used for safety reasons. Or the use of low-quality glasses purchased in order to save money;
- Smoke effects on the mucous membranes of the eyes;
- Release of gases affecting the eyes;
- Foreign body getting into the eye. Most often, these are very small pieces of metal that stick into the cornea.
What happens to the eyes during welding and what are the consequences?
Welding is not only the joining of metal parts; it is also used when working with other materials. Electric current is used as a source of formation of the welding arc. So what exactly causes harm?
When welding, rays of three spectra are released at once: infrared, ultraviolet and light. The intensity is too high for the human eye, it exceeds the permissible level.
There is a common expression among welders: “catching a bunny.” This means that the cornea of the eye has been burned. We do not perceive infrared and ultraviolet rays with our eyes, but they have a very intense effect on the eyes. Moreover, negatively. Damaging the mucous membrane, retina and lens of the eye, causing a burn.
The main eye disease that occurs under the influence of light radiation from welding is electroophthalmia.
What other causes of eye damage from welding are there?
- Negligent attitude towards work. Often welders do not use special safety glasses, which are required to be used for safety reasons. Or the use of low-quality glasses purchased in order to save money;
- Smoke effects on the mucous membranes of the eyes;
- Release of gases affecting the eyes;
- Foreign body getting into the eye. Most often, these are very small pieces of metal that stick into the cornea.
List of drugs
Painkillers
The first step is to relieve eye pain resulting from welding. To do this, drops with a local anesthetic effect are used. The most effective remain:
Lidocaine. Use a 2% solution. Inocaine. This drug helps reduce pain without leading to the development of irritation of the conjunctiva and cornea, which cannot be said about the previous medication.
The pain can be relieved within 30 seconds after using the selected drug.
Antibiotics
Once the pain syndrome has been relieved, it is worth taking care that no infection has penetrated into the wound canals. To do this, you will need to use drops with an antibacterial effect. The following drugs remain effective:
Sulfacyl sodium. An effective medication that is often used in the presence of purulent discharge from the affected organ of vision. Tsipromed. This medicine has a powerful antibacterial effect. It can be effectively used in the treatment of burns of the cornea and retina. In this way, the development of infection can be prevented. Phloxal. This tool is one of the most advanced. It has a serious antibacterial effect for burns and infections of the inner surface of the mucosa. Normax. This drug is characterized by all the same properties. It effectively copes with the bacterial environment that affects the eye during a burn. Dexamethasone. This is a corticosteroid medication that perfectly relieves swelling. Positive dynamics from these drops can be seen after 4-6 hours.
Vasoconstrictors
With the help of these drugs, you can relieve swelling of the cornea of the visual organ, inflammation and redness. Drops such as Visin, Proculin and Visoptin remain very effective today. They should be dripped 1 drop 3 times a day.
Recovery drops
At the last stage of treatment, it is necessary to eliminate all the consequences of the injury. To do this, it is effective to use drops with a restorative effect.
Thus, the following drugs can be used in turn:
Emoxipin. This drug has a tonic effect on the blood vessels of the eyes. When using drops, it is possible to resolve hemorrhage in the mucous membrane of the visual organ, as well as normalize blood flow in the vessels. Derinat. This product is suitable for quickly and scar-free removal of burns resulting from welding. Due to the active components, it is possible to accelerate the restoration of damaged tissues. Vitasik. The action of this drug is aimed at improved healing of lesions in the internal environment of the visual organ.
First aid
How to help your eyes after welding? First of all, you should not ignore the symptoms that arise. If you help a person in a timely manner, you can not only alleviate his condition, but save his vision.
In addition, first aid to a person who has caught bunnies from welding comes down to the following:
- To relieve eye pain, a person must be given an anesthetic. Analgin and Ketanov are best suited. In addition, first aid involves the use of anti-inflammatory drugs - Tavegil, Diclofenac.
- Rinse your eyesight with a large volume of purified water.
- If small metal particles have entered the eye, you should use a sterile cotton pad or black cloth to remove them. If you cannot cope with this process on your own, then you should consult a doctor, as he has special equipment.
- Apply a cold compress to the skin of the eyelids. You can use a cold decoction of chamomile for this. In addition to the cooling effect, chamomile will prevent the development of inflammation. The duration of the cold effect is 5-10 minutes.
- Treat the eyelid skin with antiseptic ointment. Tetracycline ointment has proven itself to be excellent.
As soon as a person has been provided with first aid, an urgent need to visit a doctor for consultation. Examination and timely diagnosis are excellent prevention against various eye complications.
Vasoconstrictor drops
After pain relief, a drug is used that will effectively treat pathological symptoms: relieve swelling, remove redness and inflammation, relieve itching.
These drugs are based on adrenergic agonists that act on the receptors of the vascular walls. They cause the blood vessels to constrict, resulting in relief of the symptoms of the disease.
Vasoconstrictor eye drops are very effective, but they cannot be used for a long time. Otherwise, they will cause the opposite effect.
Eye drops after welding with a vasoconstrictor effect are used for no longer than 5 days. Otherwise, addiction to the drug develops and then the symptoms that needed to be eliminated intensify.
How long will your eyes hurt?
Symptoms of a burn do not appear immediately. Symptoms increase gradually over 7 hours. If there is no damage to the retina, the pain will be felt for a couple of days. In this case, there is a feeling of anxiety, spasms and lacrimation. But after a while all this passes. If the mucous membrane is burned, the course of therapy is determined by the doctor, so the duration of the pain will be determined taking into account the severity of the injury. Often, after completing a course of therapy, pain still occurs.
Any thermal injury cannot go away in one day. In order for complete recovery to occur, you must endure unpleasant symptoms for 7 days, or maybe longer. it all depends on the complexity of the pathology. If a person feels relief the next year, then this is not a reason to refuse treatment. All therapeutic measures must be carried out daily. It’s better not to go to work, but to take sick leave.
What to put in your eyes after welding
Treatment for burns of the mucous membrane of the eye, forms 1–3, involves the use of a complex of medications, the main place among which is taken by drops. The choice of their variety is individual in each case, since it depends on the degree of damage to the organ of vision.
Self-prescription of medications is unacceptable. Using inappropriate medications may make the situation worse.
Painkillers
In order to relieve pain resulting from a burn to the mucous membrane, ophthalmologists often prescribe anesthetic drops. The active substances included in their composition act on nerve endings, blocking pain impulses.
The most common eye painkillers used for damage from welding “bunnies” are drugs such as Novocaine, Lidocaine, Alcaine, Tetracaine. Anesthesia of the conjunctiva and cornea occurs 1–2 minutes after their administration and lasts for 1.5–2 hours.
To avoid side effects, painkillers should be used after consultation with a specialist, without exceeding the dosage and duration of therapy indicated by him.
Anti-inflammatory and decongestant
The next stage of complex therapy for eye burns is the fight against the inflammatory process developing in the organ of vision. For this purpose, the following categories of drops are used:
- Vasoconstrictors and decongestants, for example, Visin, Octilia, Visoptic. The introduction of these drugs helps eliminate redness and swelling of the mucous membrane, restore its microflora, and relieve burning and itching.
- Non-steroidal anti-inflammatory drugs - Diklo-F, Prenacid, Diclofenac. The drops help stop the acute inflammatory process, reduce pain caused by damage to the corneal epithelium, and minimize the risk of developing post-burn complications.
To achieve a positive effect, ophthalmologists recommend using this category of eye drops for at least three days.
Regenerating
Elimination of the consequences of burns resulting from welding work is carried out through the use of special restorative preparations based on dexpanthenol. This active component promotes the regeneration of microdamages of the cornea and erosions formed on the mucous membrane of the eye, and also accelerates the healing of damaged conjunctiva. Most often, ophthalmologists prescribe drugs such as Khilozar-Komod, Korneregel.
Another category of drops used to restore the eye shell damaged as a result of a burn from a welding arc are immunomodulators. When they are administered, the permeability of blood vessels is significantly reduced and their walls are strengthened, and the process of resorption of hemorrhages proceeds better and faster. Derinat, Emoxy-Optic, and Emoxypin drops are especially popular.
Antimicrobial
To avoid the development and reproduction of pathogenic microflora in the damaged surface of the eye, ophthalmologists recommend the use of broad-spectrum antibacterial drugs. The most commonly prescribed drops are:
- Dexamethasone;
- Sulfacyl sodium;
- Levomycetin;
- Phloxal;
- Normax.
These drugs protect the mucous membrane of the organ of vision from the development of gram-positive and gram-negative pathogens on it, and fight purulent discharge. The duration of therapy with antimicrobial drops is 7–10 days.
Cleaning products
Before injecting medications into the conjunctival sac, you should rinse your eyes with a solution recommended by your doctor. This can be either saline solution or a variety of antiseptic liquids. In addition, you can use a weak solution of potassium permanganate or freshly brewed chamomile decoction.
This procedure has a bactericidal and antioxidant effect and prevents the spread of infection.
For rinsing, disposable cotton pads or napkins are used. They are generously moistened with a disinfectant solution and then applied to the eyes.
Antibacterial agents for treatment
Often, the use of antibiotics is a necessary measure to relieve the inflammation that has begun .
In addition, antibacterial drugs are often prescribed to prevent conjunctivitis.
For your information! Typically, the course of treatment with such drops is 7-10 days, depending on the degree of damage. The dosage of the drug is selected individually and can range from 1 to 6 drops.
The most common antibacterial drops include:
- Tobrex;
- Oftaquix;
- Gentamicin.
The use of antibiotics is possible only after consultation with an ophthalmologist . Self-medication with such drugs can significantly aggravate the situation.
Welding eye burn: first aid, treatment, drops, traditional medicine
> First aid >
07.11.2019
The welding profession is included in the group of dangerous and harmful to human health. However, eye burns from welding occur not only in production.
Now that purchasing your own welding machine is not a problem, you can “catch bunnies” anywhere. But regardless of where the injury occurred, the result is the same: in the late afternoon, the burned person literally washes himself with tears, household members have no idea about the causes of the strange symptom, and precious time is running out.
But in some cases, a minute of delay leads to irreversible impairment of visual functions
To save a victim from blindness, it is important to know the symptoms of an eye burn and the basic rules of first aid.
The main causes of eye burns from welding
Neglecting the rules for working with a welding machine can result in a burn to the cornea of the eye. Often the organs of vision are affected in the following cases:
- Assembling metal structures without the help of a partner and fasteners. Without wearing a mask, the welder holds the parts with his own hands and places tacks.
- Using a low-quality mask. Ultraviolet rays penetrate into the gaps between the filters and the mask frame.
- Using the wrong mask. To perform some tasks, an automatically darkening chameleon mask is required. In a mask with a regular shield, a worker simply will not have time to cover his face.
Presence during welding work (forced or accidental). The risk of injury increases on bright sunny days. Having succumbed to the deceptive sensation of the faint glow of the arc, a person loses his vigilance and by the evening he receives a full bouquet of burn symptoms.
What causes electroophthalmia?
Electrophthalmia is a burn of the eyes caused by welding, quartz or other powerful light source in medical language. The main cause of injury is the effect of ultraviolet rays on the mucous membrane, involving the cornea and retina.
The depth of damage depends on the scale of irradiation. A burn to the mucous membrane occurs when:
- a particle of hot metal or a spark gets into an unprotected eye;
- open contact with fumes of metals and gases;
- ultraviolet/infrared radiation;
- failure to comply with safety regulations (described above);
- exposure to thick toxic smoke (from a melted electrode) in the eye.
Symptoms of a welding burn
Immediately after a welding burn to the eyes, there are practically no symptoms. They grow within 6–12 hours. During this time, a person who has “picked up bunnies” can prepare everything necessary to provide first aid. If the burn is deep, it is better to see a specialist when the first symptoms appear.
Let's look at the general signs that help identify electroophthalmia:
- The first sign of a welding burn is a strong or mild burning sensation in the eyes, developing into a sharp pain. If you close your eyes tightly, it becomes easier. However, this is a deceptive feeling, because when you open your eyes, the pain returns.
- Tears constantly flow from the eyes, it hurts the victim to look at the light.
- With deep damage and involvement of the retina, a person sees nothing. However, there is no need to panic; in most cases, vision returns after 48 hours.
- When looking at the light, spots of light “stand” before the eyes. The duration of the symptom is determined by the duration of contact with the traumatic factor.
- You can feel the sand under your eyelids. Do not rub your eyes under any circumstances! This can accelerate the development of the inflammatory process and lead to swelling of injured tissues.
- The eye pain gradually spreads to the head, intensifying when you try to move your gaze to the side.
Signs of eye damage depend on the severity of the burns. In medicine there are:
- I degree (mild) – a burn of the cornea of the eye is expressed by decreased transparency, darkening of the cornea, and redness of the conjunctival membrane. In some cases, there is a slight burning sensation and itching. The victim can be helped at home.
- II degree (medium) – after an injury, the eye becomes covered with a film, the cornea is damaged, becomes loose and erosive. Victims experience photophobia and severe pain.
- III degree (severe) – visual functions sharply decrease, the eyelids swell, and severe aching pain occurs. There is a constant sensation of a foreign body under the eyelids (as if sand had been poured into the eyes). You cannot do without medical help.
- IV degree (extremely severe) – the injured tissue begins to die, the cornea becomes whitish, the victim screams in pain and cannot open his eyelids. Without timely medical assistance, a person becomes blind.
What to do if your eyes hurt from welding?
There is a certain group of professions that are constantly at risk of visual impairment. In the first place is the profession of a welder. This person is dealing with massive ultraviolet rays that affect the cornea of the eye, and the pain that occurs is called electroophthalmia. Occurs due to sparks that fly when working with a welding machine.
Therefore, you need to be extremely careful, because the eye is a very sensitive organ.
A welding machine is a complex structure, and if basic safety rules are not followed, you can get a corneal burn, which is preceded by “sun spots,” or get a serious disease called electroophthalmia.
Symptoms of electroophthalmia
The symptoms of the lesion completely depend on the stage of the burn; there are 5 of them:
1. light:
- unpleasant burning of the eye, but not yet painful;
- redness of the conjunctiva;
- irritation of the eyelid;
- clouding of the cornea of the eye.
2. medium:
- a pronounced sharp pain in the eye is felt;
- it is unpleasant to look at the light - photophobia;
- a film appears on the conjunctiva;
- Erosion begins in the cornea - damage to the corneal epithelium.
3. heavy:
- severe clouding of the cornea of the eye;
- sore eyes and swollen eyelids;
- vision decreases.
4. extremely severe stage:
- terrible pain and the person cannot open his eyelids;
- the cornea is colorless.
5. blindness.
The objective possibility of developing pain is very high if a person, while performing his professional work, often takes off his welding mask and works without it.
First aid
The first steps to take if sparks get into your eyes:
- The patient should take a painkiller (Ketone or Analgin are perfect).
- Rinse eyes with plenty of clean water.
- Use a clean, sterile cloth, untreated, to remove foreign objects from the eye, if any.
- Apply a cold compress. Moisten a clean cloth with cold water.
- Apply tetracycline.
After all procedures, consult a doctor for advice. In severe cases, hospitalization is prescribed. If you seek medical help in time, it is quite possible to save your vision.
At home, to prevent the development of electroophthalmia, you can make herbal compresses.
What medications will help relieve the symptoms of a burn?
The use of medications to treat various diseases is very popular. Each person decides for himself how to deal with the disease. For electroophthalmia, it is best to consult an ophthalmologist, and the doctor will prescribe the necessary medications. The main goal of treatment is to relieve pain, but you cannot stop there and you need to continue treatment. You cannot use painkillers such as Novocaine and Lidocaine. Homemade cold compresses or special herbal solutions are often used along with pain relievers.
Incompetent people should not get too involved in home pharmacy!
Eye moisturizers are often used and are often called artificial tears. Gels are also applied to the cornea of the eye, which promote rapid healing and accelerate the epithelization of the ocular cornea. For example:
- Actovegin gel;
- Solcoseryl gel;
- Korneregel;
- Retinol;
- 5% thiamine ointment.
All pharmacy methods for treating electroophthalmia can be grouped into 3 categories:
- Eye drops to relieve puffiness can only be purchased after consultation with a specialist. The ophthalmologist will determine the degree of the burn and prescribe the necessary individual remedies. The main function of such drops is to relieve swelling. Most often, Visoptin, Proculin, Visin are suitable for this. They eliminate pain, which is manifested by itching and burning, and at the same time fight the burn, rather than mask it.
- Drops that relieve pain - Alcaine and Tetracaine.
- Antibiotics for the eyes - vitalize the cornea and reduce crippling pain. A good remedy for disease prevention. Gentamicin, Tobramycin, Levofloxacin should be highlighted. And tablets: Indomethacin, Diclofenac. Dust-like agent - Nimesil. In the form of eye drops – Clodifene.
To prevent keratitis, prevent complications and accelerate healing of the cornea, use the following eye drops:
- Tobrex;
- Tobradex;
- Levofloxacin.
Some experts recommend treatment with urine therapy. But this method is quite ambiguous and doubtful.
At home, it is better to wear an eye patch for 24 hours. This will help speed up the regeneration of the epithelium.
Folk remedies for electroophthalmia: how to get rid of “bunnies in the eyes” from welding
A home pharmacy differs from drug treatment in its general availability. It's simple and inexpensive, but it does require effort. Beneficial treatment methods include:
- Honey and aloe. It is not recommended to use at stage 1 of a burn. The aloe needs to be crushed so that the plant releases juice, and mixed with homemade honey to a uniform consistency.
- Porridge with chamomile and butter. Relieves inflammation well.
- Cut potatoes. The juice of this product relieves pain if you hold it well on the eye. You can also grate the vegetable, place the porridge on a small sheet and bring it to the painful eye. The action lasts 15 minutes.
- Infused herbal decoctions of calendula, linden and chamomile. Very useful for preventing eye diseases.
- Wormwood extract is extremely effective. A small pinch per 1 glass of hot water will be enough.
To prevent eye diseases, ophthalmologists advise drinking chamomile tea for 3 weeks, 3 cups a day.
What should you not do if you have an eye burn from welding?
It is not recommended to do homework when treating electroophthalmia. Herbal infusions are allowed, but after high-quality medicinal treatment. You cannot ignore pain and suppuration of the eyes. It is recommended to schedule a consultation with an ophthalmologist immediately. Also, you should not take antibiotics or instill eye drops into your eyes without a prescription from a specialist. It is not advisable to take painkillers - Lidocaine and Novocaine.
With electroophthalmia, sand is felt in the eyes and many patients begin to rub their eyes to get rid of the discomfort. Such actions are contraindicated.
Cooling the eye after rinsing with tap water does not relieve pain.
You can instill honey and aloe juice only after the inflammation has subsided.
A working method to restore vision! You will throw your glasses in the trash in just 3 days...
Restoring vision. Real life story.
The main thing is not to neglect safety precautions when working with a welding machine. It is necessary to do everything strictly according to the instructions and follow safety precautions - wear professional glasses for this type of work and use a special welding helmet.
What are the symptoms of eye damage from welding?
Symptoms of eye damage from welding are very similar to the symptoms of many ophthalmological and even allergic diseases. However, it is clear that such symptoms occur immediately after welding work, which means that the influence of the spectrum of the welding arc is to blame.
Main symptoms:
- Severe lacrimation;
- Redness and swelling of the eyelids and eyeball;
- Sharp cutting pain in the eye;
- Sensation as if sand had been poured into the eyes;
- Fear of light;
- Tight closure of the eyelids as a result of spasm.
All symptoms, especially pain, begin to intensify after a few hours. This means that the burn was still received. If the pain does not intensify and gradually the vision and condition of the eyes return to normal, after about 1-3 days there will be no burn.
What to do if some part of the eye is burned after welding, pain and discomfort intensify? The answer is clear – contact a specialist. The hospital will conduct an examination, determine the extent of the damage, and prescribe therapy.
However, the profession of a welder requires frequent business trips, trips out of town and other places where it is not always possible to receive qualified assistance at any time of the day. And ordinary people who accidentally receive such a specific eye burn do not always have such opportunities. What can be done, what preparations should I use, are there any universal drops after welding?
When to see a doctor
If you have been treated at home for some time, but after 3 days you have not been able to get rid of the pain and white spots (popularly known as “bunnies”), then immediately go to the doctor. In this case, the likelihood of negative changes in the visual apparatus increases.
You should immediately visit a doctor if complications occur:
- Cloudiness of the cornea;
- The appearance of erosions;
- Deterioration of vision;
- Inflammation of the cornea (keratitis).
You cannot do without qualified medical care for electroophthalmia of 3–4 degrees.
Severe damage is indicated by nagging or unbearable pain, swelling of the eyelid, the sensation of a foreign body in the eye, severe clouding of the cornea, and a sharp decrease in vision. In such cases, surgery may be necessary to avoid blindness.
Which drops after welding to choose
The choice of medicine is made based on the stage of the burn. Each stage has its own symptoms.
First stage
Characteristic symptoms:
- Very severe itching;
- Redness of the whites of the eye, which can be regarded as minor. Characterized by a faint pink color;
- Burning;
- Cloudy iris.
During this period, the use of drops after welding is the most effective means for therapy and prevention of the development of the disease.
What medications will be needed:
- Anesthetic drops after welding. They will help relieve all unpleasant symptoms: pain, itching, feeling of sand in the eyes and others;
- Vasoconstrictor drops. They will relieve swelling and inflammation;
- Antibacterial drops. They will prevent infection from developing and accelerate tissue regeneration.
Second stage
- Erosion of the cornea of the eye;
- The conjunctiva is covered with a film;
- Severe photophobia, resulting in spasms;
- Very strong sharp pain when moving the eyeballs.
At this stage, to treat an eye burn, it is possible to use the above types of drops.
There are also third and fourth stages. Self-treatment is not recommended. These are very difficult stages, at the fourth stage tissue necrosis is already possible and only surgical intervention will help here. At these stages, the use of any medications in the form of drops is practically useless.
Important: do not delay your visit to the doctor! Be sure to tell us exactly which drops after welding were used for treatment. If you receive a burn as a result of exposure to welding, then most likely inflammation has begun
This means the use of antibiotics will be required. But they must be in shape. Which will allow you to apply them topically, directly to the affected area
If you receive a burn as a result of exposure to welding, then most likely inflammation has begun. This means the use of antibiotics will be required. But they must be in shape. Which will allow you to apply them topically, directly to the affected area.
The most famous drops with an antibacterial effect:
- Tobrex;
- Oftaquix;
- Gentamicin;
- Dexamethasone;
- Taufon or Taurine.
The mechanism of action of antibacterial drugs is to block the formation of bacterial proteins by binding to bacterial ribosomes.
Method of application: by introducing drops onto the conjunctival sac. The dose of use always depends on the severity of the condition, but the usual dosage is:
- For infections with moderate symptoms, antibacterial eye drops after welding are used in the amount of 1-2 drops with an interval of 4 days;
- For infections with symptoms of high severity, it is recommended to reduce the interval of drug administration - 1-2 drops every hour;
- Antibacterial drops can be used for a course of no more than 2 weeks.
Contraindications for use:
- Intolerance to components;
- Infancy (less than 1 year);
- Severe kidney pathologies;
- Pregnancy and breastfeeding;
- Myasthenia;
- Acoustic neuritis.
Side effects:
- Reaction to light in the form of a spasm;
- lacrimation;
- Burning and itching;
- Development of bleeding of mucous membranes;
- Hallucinations.
Important: before using eye drops after welding, contact lenses must be removed. In addition to the main treatment for a burn, active restoration of the mucous membrane is required.
For this purpose, medications are used that have a reparative and regenerative effect.
In addition to the main treatment for a burn, active restoration of the mucous membrane is required. For this purpose, medications that have a reparative and regenerative effect are used.
Revitalizing drops:
- Emoxipine is used for the treatment and prevention of burns and hemorrhage in the sclera. The antioxidant agent is used 1-2 drops. up to 3 times a day Emoxipin can be used for 30 days. If the medicine is well tolerated, treatment is extended to 6 months.
- Derinat is an immunomodulatory agent. It forms systemic immunity, allowing tissues to regenerate faster. Derinat activates the lymphatic system, reduces the severity of inflammation. Can be used during pregnancy.
- Actovegin is an eye gel. Activates metabolic processes, stimulates tissue regeneration and trophism. Actovegin is used for therapeutic and prophylactic purposes.
- Sicaprotect is a remedy used for diseases when the patient cannot mechanically close the eyelids. It improves tear secretion, accelerates healing and restoration of the mucous membrane. Use up to 6 times a day, 1 drop. into the affected organ of vision.
- Korneregel stimulates the healing process. Recommended for use on burns of any degree.
- Vitasik activates cellular metabolism. The drops restore the corneal epithelium with long-term use. After opening the bottle, Vitasik should be used within 2 weeks.
Is it possible to work as a welder with astigmatism?
Many people dream about them since childhood, others don’t know how to get there. Those who have them are looked upon with respect and envy, and almost half of the world's population are unable to access them due to poor eyesight.
You will soon find out why the pilot is so happy)
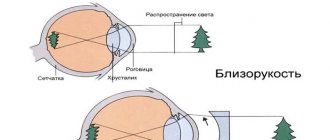
When determining contraindications to a particular profession, persons with slight and non-progressive mild myopia are considered practically healthy
.
All professions are available to them, with the exception of those in which it is impossible to wear glasses, as well as those in which the loss or failure of optical correction means poses a danger to the life of the worker himself or those around him.
Such professions include most specialties on space, air and water ships, combat vehicles, as well as those associated with work in hot and dusty workshops, mines, at heights and in other places of increased danger.
Lunch at the New York High Altitudes
Persons with moderate to high myopia
, as well as with complications in the fundus (regardless of the degree of refractive error), are considered as a group with an increased risk of visual disability. Professions associated with lifting and carrying heavy objects, exposure to vibration and acceleration on the body, as well as prolonged exposure of the body to a bent position with the head down are contraindicated for them.
It is customary to distinguish several categories of refractive errors:
1️⃣ Myopia up to 1.0 diopter
. At the same time, professions that require very high visual acuity without glasses are contraindicated;
Maria Sharapova
????
Sports star:
350,000 – 17 million rubles/month.
???? Test pilot:
150,000 – 350,000 rubles/month.
???? Cosmonaut:
250,000 – 1.5 million rubles/month.
???? Paratrooper:
50,000 – 250,000 rubles/month.
????
Marine:
50,000 – 250,000 rubles/month.
???? Work in special forces:
80,000 – 250,000 rubles/month.
???? Bodyguard:
150,000 – 1 million rubles/month.
???? Forensic expert:
80,000 – 200,000 rubles/month.
????
Lifeguard:
75,000 – 250,000 rub./month.
Another change of the ISS team
2️⃣ Myopia from 1.0 to 2.0 diopters
.
Persons with this type of myopia are not contraindicated for work that requires eye strain. They can even work as gas or electric welders. According to the assessment of the quality of work, people with low myopia are better at precise work than those with normal vision. ????
Racer: 450,000 – 14 million rubles/month.
RedBull Racing
3️⃣ Myopia from 2.0 to 4.0 diopters
.
It is contraindicated for professions related to movement at heights, control of large mechanisms (construction, road, loading, metallurgical), most professions of flight personnel and crew, as well as those related to work in hot and dusty workshops, in coal mines.
With the progression of myopia, it is also undesirable to choose professions that involve precision work and require constant use of optical instruments (magnifying glasses, microscopes, stereo devices, etc.): ???? Metallurgist:
50,000 – 150,000 rub./month.
????
Diver: 80,000 – 150,000 rub./month.
???? Jeweler:
150,000 – 400,000 rub./month.
????
Miner: 50,000 – 150,000 rub./month.
????
High-altitude installer: 80,000 – 200,000 rubles/month.
????
Crane operator: 100,000 – 240,000 rub./month.
????
Polar explorer: 70,000 – 250,000 rubles/month.
????
Airplane pilot: 350,000 – 650,000 rubles/month.
Because, because, we drank...
Pilot vision requirements in Russia (for commercial and line pilots)
Minimum visual acuity: 0.6 for each eye separately, with correction - 1.0.
Refraction: ranging from -3 to 3 diopters. Anisometropia (difference between the refraction of the eyes): no more than 1 diopter. Astigmatism: no more than 2 diopters. Not allowed: acute or chronic eye diseases, presbyopia over 4 diopters, strabismus.
Vision requirements for pilots in Russia (for private pilots)
Minimum visual acuity: 0.5 for each eye separately, with correction - 0.8.
Refraction: ranging from -3 to 3 diopters. Astigmatism: no more than 2 diopters. Not allowed: acute or chronic eye diseases, strabismus.
Glasses and contact lenses, surgical vision correction:
correction with glasses or contact lenses is allowed.
At the same time, unlike other countries, visual acuity is checked not only with lenses/glasses, but also without them, so in some cases correction with glasses or contact lenses does not help. 4️⃣
Myopia from 4.0 to 8.0 diopters
. In addition to those listed above, professions associated with constant driving of a car and other vehicles, as well as work in low light conditions, are undesirable.
???? Driver:
50,000 – 150,000 rub./month.
????for drivers of category “B” (restriction as - the driver can drive a car with a steering wheel) visual acuity must be at least 0.6 units in one eye and 0.2 units in the other; ???? for drivers of category “C” – not less than 0.8 units in one eye and 0.4 units in the other;
???? for drivers of category A, A1 or B2 with a motorcycle-type steering wheel - not lower than 0.6 on one and 0.2 on the other.
Source: https://mir-ua.ru/mozhno-li-rabotat-svarshhikom-s-astigmatizmom/