Phakic lens implantation is a surgical method of vision correction by installing an intraocular lens into one of the chambers of the eye without removing the natural lens. This operation is advisable for high degrees of myopia, farsightedness, and astigmatism.
During the operation, performed under local anesthesia and under microscope control, a small incision is made in the cornea. Using an ophthalmic syringe-injector, the implant is installed into one of the chambers of the eye. At the end of the operation, after revising the location of the lens, an antibiotic is injected into the eye and covered with a sterile bandage. Complications from phakic lens implantation are quite rare. Known complications include cataracts, endophthalmitis, increased intraocular pressure. The period of complete recovery does not exceed several weeks, but you can return to work within 5-7 days after the procedure.
Phakic intraocular lens
The history of intraocular (that is, implanted inside the eye) lenses began in the middle of the twentieth century.
The first successful implantation of this type of lens was carried out in Italy in the 1960s. In those days, only one option for placing and fixing the lens was possible - in the anterior chamber of the eye. The material for the manufacture of the implant was a solid polymer, polymethyl methacrylate. After the operation, the patient received excellent quality of vision, without experiencing discomfort or feeling a foreign body in the eye. However, in the long term, many patients developed various complications - and the operation became unpopular. In the 1980s, when there was a quantum leap in the development of medical technology, ophthalmologists returned to the practice of using phakic lenses. New methods of positioning and fixing implants, as well as more advanced materials for their manufacture, appeared.
Today, the largest manufacturers of optics for phakic lenses are companies from the USA, Switzerland, Germany, England and Russia.
Modern phakic intraocular lenses (PIOLs) have a number of undoubted advantages:
- Complete reversibility of the operation:
if such a need arises, the doctor can remove the lens without damaging the cornea and lens. - Biocompatibility:
the implant is not rejected by the body. - Minimal trauma:
the microscopic incision heals on its own, vision is restored within a few hours after the procedure, the anatomy of the eye is not disturbed. - Manufacturing according to individual parameters:
each phakic lens is manufactured for a specific patient, according to individual measurements. - Eye protection from ultraviolet radiation.
We can say that such lenses are similar to contact lenses, only they are implanted inside the eye, and not put on top.
Varieties
After cataract surgery or refractive lens replacement surgery, an intraocular lens is implanted to replace the natural lens. two types of intraocular lenses
- hard;
- soft.
Read about caring for long-term contact lenses here.
Rigid intraocular lenses have a permanent shape. They lack flexibility, so the operation to implant them has a significant disadvantage: a large surgical incision is made, and then sutures are applied. The patient's rehabilitation period after such an operation lasts quite a long time.
Most modern ophthalmological centers and clinics recommend implanting soft intraocular lenses made of elastic polymer materials. To introduce them, a self-sealing micro-incision (about 1.8 mm) is made, which does not require sutures after surgery. Soft lenses are inserted into the eye when folded, then they unfold independently and are securely fastened.
Based on the principle of impact on the functioning of the visual organ, intraocular lenses are divided into several types. Let's look at each of them in more detail.
Trifocal
If the patient does not want to wear glasses after cataract removal and still wants to have good vision at all distances, a trifocal intraocular lens is implanted. This lens has three focuses, which provides high quality vision at close, medium and long distances. The optical structure of a trifocal lens is unique. Its design allows for smooth focus shifting. In addition, the trifocal lens is equipped with aspherical properties to correct spherical distortion. This ensures high contrast sensitivity.
Accommodating
Lenses of this type perfectly imitate the work of the natural lens of the eye and provide the patient with excellent vision near, far and at medium distances.
Accommodating intraocular lenses in their properties and characteristics are as close as possible to the natural human lens. Their unique design allows the eye muscles to move and flex just like a real lens.
The characteristics of the accommodating lens provide the user of any age with good vision at any distance. In addition, they relieve the patient from two age-related vision problems at once: cataracts and presbyopia (age-related farsightedness).
Lens implantation
Multifocal
As a rule, with age (usually after 40-45 years), each person begins a natural change in accommodation - the ability of the eye to clearly see objects at different distances. The lens of the eye thickens, becomes less elastic, loses flexibility and the ability to quickly change its shape. All this forces a person to use glasses when working. After some time (at 60–70 years), the ability to accommodate is completely lost and you have to use glasses not only for work, but also for any activity.
Multifocal (pseudo-accommodating) lenses have a special advantage over classic contact lenses. They have not one, but several focuses, thereby making it possible to achieve maximum visual acuity at different distances, as well as reduce a person’s dependence on glasses (or get rid of them altogether).
According to statistics, about 80% of patients who have been implanted with a multifocal contact lens do not use glasses at all.
Depending on the principle of action on the eye, multifocal lenses come in two different designs:
- with mixed diffractive-refractive nature of optics;
- with combined radial sectors.
Toric
In cases where cataracts (partial or complete) are complicated by astigmatism, toric intraocular lenses are used. Astigmatism can be corneal and lens. The first type of astigmatism is more common in patients, since the cornea of the eye has a greater refractive power than the lens.
Some time ago, cataracts combined with astigmatism created great difficulties for the surgeon. Even after cataract removal, the person had to use special cylindrical glasses. The development and active use of toric intraocular lenses has allowed patients with cataracts complicated by astigmatism to gain a new quality of visual life. Such a lens has a significant refractive power, which allows it to reduce and even completely eliminate the patient’s corneal astigmatism and increase distance visual acuity. A toric intraocular implant not only replaces the optical power of the removed cloudy lens, but also corrects the original corneal astigmatism.
Find out how to put on toric lenses in the article.
Aspherical
These lenses are specially designed to correct spherical aberrations, which are very common in patients after implantation of an artificial lens. The reason for their occurrence is usually a mismatch between the optical system: the human eye and the intraocular lens.
The most common type of distortion is spherical aberration. They arise due to the refraction of light at different angles as it passes through the spherical surface of the intraocular lens and the optical media of the eye. Without the necessary correction, light rays do not focus accurately on the retina and the image may be unclear and blurry. Often, after cataract surgery, patients with good visual function suffer from glare, reflections, and halos, which are most pronounced in the evening or at night.
When using traditional lens models, it is impossible to avoid the occurrence of spherical aberrations. Today, special models of lenses with an aspherical surface have already been developed.
Intraocular aspheric lenses have the same optical power in all areas, so light rays refracted through it are focused at one point and not at several points. These unique characteristics of the implant make it possible to obtain higher quality images, especially in low light conditions with a highly dilated pupil.
With yellow filter
In addition to accommodating characteristics, the natural human lens has special protective properties that protect the retina. With age, the lens of all people turns yellow. This is a natural mechanism to protect the retina from the negative effects of UV and blue rays (to prevent the development of retinal dystrophies). During cataract surgery, the surgeon replaces the cataract-damaged lens with an artificial intraocular lens. The yellow filter is also removed along with the lens. Thus, the protective functions of the eye are reduced and the risk of developing age-related retinal diseases increases.
The new generation lenses have a yellow filter similar to the filter of the natural human lens. Its function is to cut off the rays of the blue spectrum without disturbing the balance of color perception. Thanks to the artificial yellow filter, the intraocular intraocular lens protects the retina in the same way as the natural lens of the eye protects it.
Monoblock
Great progress in cataract surgery was the creation of a unique model of intraocular lenses - Monoblock.
Such a lens contains supporting elements – optics and haptics, which are made from the same bioactive material. Thanks to this, the risk of reaction of eye structures and the development of secondary cataracts is minimized.
The single design of the Monoblock intraocular lens made it possible to reduce the incision for implantation to 1.8 mm, as well as avoid numerous risks and complications during surgery. Any possibility of rejection of such a lens is excluded. During the implantation of a monoblock lens, the tissues of the eye are not injured, while they retain their shape and integrity. The lens itself is inserted through a disposable injector, which reduces the risk of lens infection. The experience of implanting Monoblock artificial lenses is already enormous: more than 15 million operations worldwide.
Advantages of posterior chamber phakic IOLs
- Posterior chamber phakic IOLs, while in the eye, do not contact the cornea or iris, which prevents dystrophic changes.
- The lenses are biocompatible with body tissues.
- PIOLs protect the retina from the negative effects of ultraviolet rays.
- Visual function is restored quickly.
- The integrity of the cornea is preserved.
The main difficulty in using intraocular phakic lenses is the high requirements for calculation accuracy and flawless work of the ophthalmic surgeon. This is why a full ophthalmological examination is performed before surgery. Detailed diagnostics, during which a whole range of procedures are carried out, allows the specialist to draw up a detailed picture of the condition of the patient’s visual analyzer and optimally select lenses.
Advantages and disadvantages over other IOLs
Advantages:
- the possibility of simultaneous treatment of cataracts and elimination of corneal astigmatism;
- the quality of vision improves after the first procedure;
- intraocular correction of severe myopia, as well as farsightedness in combination with astigmatism, is performed;
- astigmatism is corrected from 0.5 to 4.5 diopters.
Flaws:
- minimal displacement changes focus;
- the results of the operation are easily deteriorated by the slightest mistakes;
- sometimes patients exhibit individual intolerance;
- they take a long time to adapt to new artificial lenses;
- irritation occurs after foreign objects get into the eyes;
- soft toric lenses do not give good results and slightly increase visual acuity.
An artificial lens belongs to the category of complex optical products and requires the work of a professional surgeon.
Indications and contraindications for implantation of intraocular phakic lenses
The use of phakic lenses is possible only in cases where the visual system has not lost the ability to natural accommodation. First of all, this concerns the lens of the eye - it must function fully. Implantation is guaranteed to help with farsightedness, nearsightedness or high degree of astigmatism.
Phakic lenses are suitable for people who are prohibited from laser correction (for example, due to a very thin cornea or other pathologies).
Although the operation is considered low-traumatic and does not require general anesthesia, it is a penetrating type of surgery and has a number of contraindications:
- glaucoma, intraocular pressure disorder;
- history of eye surgery (eg, affecting the vitreous or retina);
- systemic pathologies (cataracts, corneal dystrophy, lens subluxation, chronic inflammation of the vessels of the eye and others);
- period of pregnancy and lactation;
- age-related changes in the lens;
- diabetes mellitus (insulin-dependent type).
It is most effective and safe to perform implantation before the age of 50 years.
Contraindications
Concomitant diseases sometimes cause exacerbation and cause complete blindness.
Contraindications:
- diabetic form of cataract;
- destruction of the corneal layer;
- glaucoma;
- the retina detaches;
- siderosis;
- tumors.
These factors are associated with contraindications to the installation of toric IOLs.
What is a phakic lens?
Thanks to the development of technology, most people suffering from myopia, farsightedness and astigmatism can count on laser vision correction. But in case of medical contraindications, laser correction may be contraindicated. These cases include myopia and farsightedness, high-degree astigmatism, as well as the category of people who, for whatever reason, do not have the opportunity or desire to undergo excimer laser vision correction.
In our Clinic, this problem can be solved by implanting a phakic lens.
The method involves implanting an additional (positive or negative) intraocular lens inside the eye with the natural lens preserved, resulting in focusing the image directly on the retina (and not in front of it, which happens with myopia, or behind the retina, which happens with farsightedness).
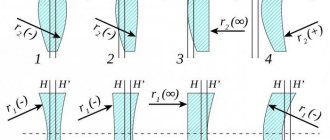
There are three types of phakic lenses that are implanted to correct refractive errors. Their name is determined by their location in the eye: anterior chamber phakic lens, iridofixation phakic lens and posterior chamber phakic lens.
An intraocular lens is a CONTACT LENS, used in adults and children since 1992 after official confirmation of safety and approval of this technique.
The proposed technique makes it possible to obtain an accurate, safe and stable refractive effect even in children over the age of 3 years. The intraocular lens corrects myopia from –3.0 to –29.0 and farsightedness from +3.0 to +11.0 diopters.
The developed software makes it possible to calculate the optical power of the PIOL depending on the anatomical and optical parameters of the eye, the patient’s age and the expected refraction in the early and late postoperative period.
Lens structure
An intraocular lens is an artificial lens that refracts light rays and forms an image on the retina. A conventional implant consists of two elements - optical and supporting.
The optical element is a lens made of a transparent material that is biologically compatible with ocular tissue. There is a special diffraction zone on its surface, which ensures the clarity of the resulting image. The supporting component allows you to securely attach the artificial lens.
The structure of the eyeball
What implantation methods are there?
A phakic intraocular lens (PIOL) can be placed in the anterior or posterior chamber of the eye. Lens models differ in size, shape of support mounts, and material. Accurate calculations when making an implant are the key to the success of the entire operation, so the doctor must conduct a comprehensive diagnosis and take into account all the individual parameters of the patient’s eye chamber. The main task is to secure the lens so that it does not touch the lens and does not affect the natural circulation of fluid inside the eye.
Lenses are made to order and can take quite a long time - up to several months.
Features of implantation in the anterior chamber:
- There is enough free space in this part of the eye for stable fixation of the lens, so this procedure is considered to be an operation of medium complexity.
- Optical calculations and measurements are relatively simple.
- The material for the implant can be either hard or flexible, elastic.
- The lens can be placed in the corner of the camera or on the iris itself.
- Possible complications: risk of damage to the iris or lens, reduction in the number of endothelial cells, changes in the shape of the pupil, chronic inflammation.
Another feature of anterior chamber lenses: they can be visible to others due to glare.
Features of implantation in the posterior chamber:
- This implantation method is technically more difficult, because there is much less free space in the posterior chamber of the eye.
- Optical calculations are complex and require very precise special measurements.
- The lens material must be elastic, repeating the shape of the lens.
- Possible complications: impaired free circulation of intraocular fluid and the risk of developing cataracts.
Posterior chamber lenses cannot be seen from the outside; they are visible only with special examination.
As you can see, both methods have their advantages and disadvantages. Modern clinics usually practice implanting posterior chamber lenses if the patient’s vision level is up to -14 diopters. But the final choice can only be made by a qualified doctor after carefully studying all the features of the patient’s visual system.
Preparation for surgery and progress of the intervention
The main scope of the preoperative examination is identical to laser vision correction operations: examination of visual acuity, autorefractometry and keratometry, intraocular pressure, keratotopography, examination of the retina, etc.
Patients with problem areas in the fundus of the eye - thinning, pre-tears or ruptures - are first treated with laser coagulation (strengthening) of the retina - RPLC. Surgery is possible 2-3 weeks after this.
Implantation of phakic lenses
The operation is performed under local anesthesia - anesthetic drops are instilled. The eyelids are fixed with an eyelid expander.
The surgeon makes a tunnel incision at the border of the transparent and opaque parts of the eyeball, measuring from 1.6 to 3 mm, depending on the type of lens and the intervention technique used. After the operation is completed, the incision closes on its own - it seals itself, and after a month there is not even a trace left of it.
The main condition: phakic lenses should not touch the transparent structures of the eye and interfere with the circulation of intraocular fluid.
A rolled lens is inserted into the eye using a special instrument. If an anterior chamber model is installed (only when installation of a posterior chamber model is impossible), its supporting elements are fixed in the corner of the anterior chamber or “clung” to the iris.
If a posterior chamber PIOL is implanted, the pupil is first dilated as much as possible with mydriatic drops. After introducing PIOL into the anterior chamber, it is straightened and the supporting elements are inserted behind the iris. A drug is instilled that constricts the pupil.
Installation of FIOLs with posterior chamber fixation is technically more difficult, but they are safer.
The choice of type and model is determined by the refractive surgeon, based on the patient’s examination data and his experience.
What is premium phakic lens correction?
Implantation of phakic intraocular lenses is used in our clinic in cases where it is impossible to correct vision using excimer laser methods. Most often this occurs when the cornea is insufficiently thick.
During this operation, an artificial lens is placed inside the eye in front of the lens, while the remaining internal structures of the eyeball must remain intact. Therefore, PIOLs are made extremely thin, and the material from which such a lens is made must have a high refractive index. In addition, the lens must be placed inside the eye through small punctures in the cornea, so it must have high elasticity. Each such lens is a high-tech product and is often made individually, taking into account the size of the patient's intraocular structures.
Currently, lenses from STAAR (Switzerland) are certified for use in Russia. You can view details about the phakic lens on the manufacturer’s website - https://www.staar.com/. Lenses from this manufacturer allow you to correct not only myopia or farsightedness, but also astigmatism.
Like any surgical intervention, implantation of phakic intraocular lenses has its indications and contraindications, therefore the final decision on the possibility of implanting a phakic lens is made by the surgeon only after a thorough examination of the patient.
Cost of implantation of anterior chamber phakic lenses in Moscow
Similar operations are performed in many multidisciplinary ophthalmological centers in Moscow and the Moscow region. The cost of the service will include the price of the selected lens and the work of the surgical team. Important factors in pricing are: the volume of surgical intervention, the cost of consumables, additional procedures performed, the reputation and experience of the surgeon. Surgeries for implantation of anterior chamber phakic IOLs are always somewhat cheaper than implantation of posterior chamber models. In some clinics, an additional article of the pricing policy is the status of the medical institution and its territorial location.
Features of the operation
Let's talk about how the operation itself to implant intraocular lenses takes place. The procedure is very demanding on the level of training of the ophthalmic surgeon, as well as on the technical equipment of the clinic. What features of the operation does the patient need to know:
- Before the operation, local anesthesia (drip) will be administered.
- The procedure cannot be called painful, but rather psychologically unpleasant.
- The incision for lens implantation is microscopic and heals independently, without sutures.
- The operation lasts only 10-15 minutes.
- It is impossible to carry out implantation in both eyes at once.
- Vision restoration occurs within a few hours after surgery.
The recovery period is very short and painless. The patient is prescribed anti-inflammatory drops, which must be taken independently. Restrictions in everyday life are minimal - almost all of them are related to hygiene procedures.
Toric IOL and its features
A toric intraocular lens is a combination of the qualities of a cylindrical and a spherical IOL. The principle of “working” of a toric lens is based on a change in optical power along one of its axes. This functionality is achieved by changing the shape of the front wall of the lens: the surface takes on the shape of a torus - then the radius along one optical axis of the intraocular lens is greater than its radius along the other axis. With all this, the back wall of the lens continues to retain the properties that are inherent in an aspheric lens. Thus, implantation of a toric lens with unique properties allows you to simultaneously solve two problems: correct vision, which has become worse due to the development of astigmatism, and remove cataracts. Conclusion: a toric IOL has greater refractive power in certain areas, and as a result, astigmatism and cataracts are compensated, which means the quality of vision becomes significantly better.
Advantages of PIOL implantation over laser vision correction
- The structure of the cornea is not disturbed when implanting phakic lenses;
- The operation is reversible - it is possible to remove (explant) the lens if necessary;
- Accommodation is preserved;
- Visual acuity is better than with glasses or contact lenses
| Recommended for the correction of visual impairment in patients under 40 years of age. |
ISLSTAAR phakic lenses are produced in Switzerland and certified by the Ministry of Health of the Russian Federation.
Implantation of phakic lenses in the clinic is carried out by ophthalmic surgeon, Professor Vyacheslav Mikhailovich Sheludchenko.
The surgeon is a proctor of the STAARSURGYCAL company in the Russian Federation, an expert in the technology of implanting phakic lenses ISL and can train ophthalmologists in surgical techniques.
To date, over 300 PIOL implantation operations have been performed.
Operation stages:
- Patient preparation. Local anesthesia. Installation of an eyelid speculum;
- Corneal puncture for lens installation;
- Implantation of a phakic lens behind the iris in front of the native lens.
No stitches are required. Outpatient management.
Good vision the next day.
The period of complete recovery and healing under the supervision of an ophthalmologist takes one month.
Implantation of a phakic refractive lens
Benefits of phakic lens implantation:
- being in the eye, they do not come into contact with the iris and cornea, which prevents the possibility of dystrophy;
- unique biocompatibility with the human eye;
- protection of the retina from ultraviolet rays;
- vision is restored 2-3 hours after the operation;
- maintaining the integrity of the corneal structure.
Since 2001, the use of silicone posterior chamber phakic lenses PRL (CIBA Vision, Switzerland, now the lens belongs to Carl Zeiss, USA) has been permitted in Europe. In the United States, it is undergoing phase 3 clinical trials under the Food and Drug Administration, which is yielding promising clinical results.
The idea of correcting myopia and hypermetropia by implanting an intraocular corrective lens into the eye was born approximately 50 years ago. In the late 1980s, this idea was finally implemented clinically. 20 years of improvement of the materials from which lenses are made, honing surgical techniques and improving ultra-precise microsurgical instruments today allows us to use an exclusive technique for implanting intraocular phakic lenses, achieving excellent results.
The thinnest intraocular lens, only 30 microns thick, made of completely biocompatible elastic synthetic material allows you to successfully correct myopia from -3.50 to -30.0D and hypermetropia from +3.0 to +16.0D.
Surgical technique for implanting phakic lenses:
- Under local drip anesthesia (there is no need to make a painful and relatively dangerous anesthetic injection), a minimal corneal incision of only 3.0 mm wide is made.
- An intraocular correction lens is inserted through this incision and gently positioned between the iris and lens in the so-called posterior chamber of the eye.
- Since the incision is very small, traditional sutures are not required at the end of the operation.
The operation is performed on an outpatient basis and lasts about 10-15 minutes, the effect occurs immediately.
The refractive result is comparable to using a regular contact lens.
From the day of surgery, the patient self-therapy, instilling anti-inflammatory drops for 7-14 days.
Possible complications:
- In isolated cases, in the first hours after surgery, a temporary increase in intraocular pressure is possible. To prevent this, diuretics are used prophylactically in the first 1-2 days after surgery.
- Clouding of the lens or the development of cataracts, possible in theory, has not been encountered in practice: it has been clinically proven that the implant is never in direct contact with the lens, but rather “floats” in the narrow space of the posterior chamber of the eye without touching it, and therefore cannot cause cataracts.
The first PRL lens was implanted in 1986. Today's PRL is a 4th generation phakic posterior chamber lens. It was approved for clinical use in the West and received the so-called CEE mark in 2000. To date, more than 20,000 PRL implantations have been performed worldwide with very promising results.
Doctor Dementiev
is the world's leading specialist in posterior chamber phakic lens implantation. He participated in the development of the posterior chamber phakic lens PRL/MPL, developed and improved modern surgical techniques for implanting phakic intraocular lenses. The entire set of microsurgical instruments for performing the operation bears his name.
All doctors who use the PRL/MPL phakic lens implantation technique (there are only 900 of them worldwide) have completed Dr. Dementiev’s master classes, which are regularly conducted by Carl Zeiss, and received the appropriate certificate.
Advantages of implantation of posterior chamber phakic lymph nodes
- 1. Precision and stability of the final result, the final effect does not depend on scarring.
- 2. Immediate refractive effect.
- 3. A quick period of rehabilitation, both physical and visual. There is virtually no postoperative pain, photophobia or lacrimation.
- 4. The only reversible procedure in refractive surgery. If necessary, after implanting a phakic lens, you can always go back by removing the lens. Any surgical error during surgery can be corrected, which is not possible with other types of refractive surgery procedures.
Today, PRL implantation is seen as the future of refractive surgery.
What are the advantages of posterior chamber phakic lenses?
The newest posterior chamber phakic refractive lens is made of silicone and has an ultra-thin design that provides a high refractive index (1.46). The optical part has a diameter of 4.5 or 5 mm and is located on the front surface of the lens. The back is absolutely smooth and matte, which theoretically should reduce the glaze effect after surgery. Silicone is a hydrophobic material and its curvature is identical to that of the natural lens, resulting in a phakic lens that avoids contact with the lens and allows posterior chamber moisture to circulate. The constant flow of fluid allows you to maintain a constant distance between the phakic lens and the lens, the lenses do not touch the anterior chamber of the lens.
Because the phakic lens is made of a hydrophobic material and its curvature follows that of the lens, the edges of the lens are located on the zonular fibers and it floats in the posterior chamber, maintaining distance from the anterior capsule.
While in the eye, phakic lenses do not come into contact with the iris and cornea, which prevents the occurrence of dystrophic changes.
The lenses have unique characteristics of biocompatibility with the human eye.
Phakic lenses have properties that protect the retina from exposure to ultraviolet rays.
Provides rapid restoration of visual functions.
Maintains the integrity of the corneal structure.
SELECTION OF PATIENTS for phakic lens implantation
Indications for implantation of phakic lenses are myopia from -3.0 to -30.0 D and hyperopia from +3.0 to + 15.0 D.
In cases of progressive myopia, operations that strengthen the sclera are indicated.
Contraindications for implantation are:
- cloudy or opaque cornea;
- cataract;
- subluxation of the lens;
- glaucoma or increased intraocular pressure;
- small anterior chamber (less than 2.5 mm);
- problems with the retina or vitreous that make good vision impossible or require surgery in the posterior segment;
- previous eye surgeries such as retinal, vitreous or glaucoma filtration surgeries.
In addition, PRL implantation is most effective and safe in patients under 50 years of age.
RESULTS OF IMPLANTATION OF phakic PRL lenses
PRL implantation is relatively safe, has predictable results, and is reversible.
PRL allows you to achieve an immediate and stable refractive effect.
With promising results and modern surgical and diagnostic equipment, PRL implantation is becoming one of the most interesting and promising areas of refractive surgery. 10 years of experience with PRL implantation gives encouraging results. PRL is used in Europe, South America, and phase 3 FDA trials have been completed in the USA.
The big advantage of PRL over corneal procedures is the ability to remove the PRL if problems arise or to better correct refractive error. Another important advantage of PRL implantation is that it does not affect the optical power of the cornea. There are no cases of cataract formation after implantation.
PRL implantation has proven to be an effective and stable technique for the correction of severe myopia and farsightedness. The optical power of the lens can be accurately calculated, and a good refractive result is achieved immediately after surgery.
Result of the operation
Phakic lenses are a very effective method of refractive correction. After the operation, the patient receives the maximum possible visual acuity in his case. Of course, in case of serious ophthalmological disorders, implantation will not return one hundred percent vision, but the result will be very noticeable.
Predictability of the result is another advantage of the operation for the patient. The doctor can provide accurate information about possible vision improvements already during the calculation of the optical characteristics for lens manufacturing.
And after the procedure, on the same day, a person will see the world around him in a new way, in all its richness of colors and details.
Is preparation required for implantation?
Proper preparation for implantation involves conducting as complete an examination of the patient as possible. This will help establish not only the presence of indications for surgery, but also identify contraindications. The examination should include accurate computer diagnostic methods that will establish all the data necessary for the doctor about the condition of the patient’s visual system.
After the examination, some time passes before implantation, because all IOLs are individual and most often they must be ordered according to the parameters that were determined for the patient during a comprehensive examination.
Arguments for and against surgery
The main disadvantage of implanting intraocular lenses is the financial side of the issue. High-quality diagnostics, ordering optics, implantation itself - all this costs a lot of money. Therefore, very often people choose other methods of vision correction.
Another difficulty is choosing a clinic and a qualified ophthalmic surgeon. Many people are frightened by the very fact of surgical intervention and the possible risks.
However, phakic lenses also have their advantages:
- modern implantation methods reduce the risks of postoperative complications to a minimum;
- the operation is reversible: if problems arise, the lens can always be removed;
- if laser correction is contraindicated, phakic lenses become an ideal alternative;
- the procedure does not violate the natural anatomy of the eye;
- The operation is well tolerated at any age and does not affect the heart and blood vessels.
There is a common myth that after implantation you will have to give up sports and physical activity. We inherited this belief from past, imperfect medical technologies. But today, operations to implant intraocular lenses are carried out at such a level that optics become an organic part of the eye, and a person can live a full life without fear of complications.
Complications
Of course, as with any surgical procedure, there are some risks associated with phakic lens implantation. For example, the risk of developing endophthalmitis, which can cause complete loss of vision, is 0.1-0.7%, but it is the same as when installing aphakic lenses. To prevent pupillary block after PIOL implantation, before or during surgery, iridotomy is successfully performed - a procedure in which several microscopic inconspicuous holes are made in the upper part of the iris.
Each type of phakic lens can lead to specific complications. Thus, ovalization of the pupil, which is accompanied by the appearance of glare, can develop after the installation of anterior chamber lenses. This occurs due to displacement or inaccurate installation of the haptic elements of the lens. In this case, they put pressure on the angle of the camera and cause problems with blood circulation in the iris or secondary fibrous changes. This can also be prevented: it is necessary to make accurate calculations on the eve of the operation and just as accurately install the lens. If such a complication occurs and the “uveitis-glaucoma-hyphema” syndrome or endothelial-epithelial dystrophy develops, then the lens may have to be explanted.
Corneal cell loss and ocular hypertension may occur with anterior chamber phakic lens implantation. The first complication is associated with the difficulty of calculating the optimal size of the lens and the possibility of its rotation after surgery, and the second is with its localization in the anterior chamber of the eyeball.
After implantation of posterior chamber FIOLs, complications such as cataracts and pigment dispersion syndrome are most often observed. They develop as a result of contact of a foreign body with the lens or iris of the patient, which occurs in hyperopics due to the narrow posterior chamber of the eye or due to inaccurate selection of the lens size.
Surgical trauma can lead to the development of cataracts. Due to some differences in the design of different lens options, its risk is more pronounced with ICL implantation than PRL implantation. Occasionally, zonular fibers may be torn during PRL implantation, resulting in displacement or decentration of the lens itself.