Indications The essence of the procedure Price Our capabilities
Selective laser trabeculoplasty is currently the most highly effective and reliable method of laser treatment for glaucoma. The operation allows you to normalize intraocular pressure, including in patients for whom drug treatment (using antiglaucomatous drops) does not bring the expected effect or is contraindicated.
The procedure prevents the development of severe complications of glaucoma, avoids surgery and returns the patient with glaucoma to a full life.
Indications
Selective laser trabeculoplasty is the procedure of choice:
- in patients with primary open-angle glaucoma, as well as with narrow-angle glaucoma after iridotomy (grade 1-2, IOP values no more than 30 mm Hg);
- with intolerance or low effectiveness of drug therapy for glaucoma, including in patients who have difficulty complying with the use of antihypertensive eye drops;
- with moderate and severe pigmentation of trabeculae in the area of the anterior chamber angle;
- in patients with postveal, pseudoexfoliative and aphakic glaucoma;
- in case of unsatisfactory results of surgical treatment of glaucoma.
Laser treatment of glaucoma – laser trabeculoplasty, iridectomy, iridotomy
Laser treatment of glaucoma is a unique method of modern laser ophthalmic surgery.
The laser plays the role of a “laser needle” or “laser knife”, with which you can perform operations on the structures of the drainage system of the eye without opening the eyeball, that is, without cutting the eye wall.
Laser treatment of glaucoma has long established itself throughout the world as the most painless and effective method of treating glaucoma.
The widespread use of lasers to combat glaucoma began in the 70s of the last century. Currently, argon, diode and neodymium YAG lasers are most often used for this purpose.
Regardless of the type of laser used, glaucoma treatment is aimed at normalizing the outflow of intraocular fluid from the eye, and, as a result, reducing intraocular pressure.
In this case, treatment of glaucoma with a laser can be performed as an independent method of treating glaucoma, or in combination with microsurgical antiglaucomatous surgery.
Benefits of laser treatment for glaucoma:
- restoration of the outflow of intraocular fluid from the eye through natural pathways;
- the operation does not require general anesthesia and is performed under local anesthesia (instillation of anesthetic drops is sufficient);
- laser treatment of glaucoma is carried out on an outpatient basis;
- low cost treatment;
- non-invasiveness of the method, which contributes to a low likelihood of complications;
- absence of complications from traditional glaucoma surgery;
- minimum rehabilitation period.
Depending on the wavelength used, the action of lasers in glaucoma is based either on causing a local burn followed by atrophy and scarring of the tissue - coagulator lasers, or on a microexplosion, which is accompanied by tissue rupture and a shock wave - destructor lasers. Therefore, of all the proposed types of laser operations, laser iridectomy (iridotomy) and laser trabeculoplasty are the most widespread.
Laser iridectomy (iridotomy)
Laser iridectomy involves creating a small hole in the peripheral part of the iris. Iridectomy is indicated for functional pupillary block and leads to equalization of pressure between the posterior and anterior chambers of the eye and opening of the anterior chamber angle.
Indications for iridectomy:
- narrow-angle glaucoma, primary and secondary angle-closure glaucoma with pupillary block;
- prevention of acute attacks of glaucoma in the fellow eye with positive stress tests;
- flat iris;
- iridovitreal block.
Laser iridectomy (iridotomy) is performed under local anesthesia on an outpatient basis. Instillation of anesthetic drops (Inocaine, Alcaine) leads to anesthesia of the eye.
A special goniolens is installed on the cornea, which focuses laser radiation on a selected area of the iris. Iridectomy can be performed in any quadrant.
However, it is advisable to perform several iridotomies in thinned areas of the iris or natural depressions in the iris stroma (lacunae) in its different sectors.
| Methodology | Iridotomy | Iridotomy. Scheme |
In some cases, the formed iris coloboma is closed by proliferating pigment epithelium. In such cases, a single laser pulse is sufficient to form a repeat iridotomy. In the same way, it is easy to achieve a through iridectomy in cases where the pigment leaf was not removed during surgical iridectomy.
As our experience shows, laser iridectomy, with proper use of laser technology, can relieve increased intraocular pressure in 95-97% of cases.
In some patients, compensation of intraocular pressure cannot be achieved due to pronounced organic changes in the drainage system of the eye.
Therefore, laser iridotomy should be performed as early as possible, before the formation of cicatricial changes in the drainage system of the eye.
| Laser iridectomy for pupillary block | Normalization of intraocular fluid flow |
Laser iridectomy can also be performed for prophylactic purposes in true narrow-angle glaucoma, which occurs in the form of recurrent acute attacks of increased intraocular pressure.
The probability of an acute attack of glaucoma occurring in the fellow eye, if it previously occurred in one eye, is about 15-20%.
Performing prophylactic laser iridotomy in all such patients can prevent the development of glaucoma in the other eye.
Laser trabeculoplasty
Laser trabeculoplasty is the main method of laser treatment for open-angle glaucoma. The essence of trabeculoplasty is the effect of laser radiation on the trabecular zone in the projection of Schlemm's canal. There are several options for laser trabeculoplasty, depending on the type of laser used.
Trabeculoplasty with a pulsed Nd:YAG laser provides a long-term and stable hypotensive effect. This technique, called “hydrodynamic activation of outflow,” was developed in Russia by prof. A.P. Nesterov and prof. E.A. Egorov.
Methods for treating open-angle glaucoma using continuous-wave lasers have become widespread, when laser trabeculoplasty is performed with a copper, krypton or diode laser.
Performing laser trabeculoplasty. The operation is performed under local anesthesia on an outpatient basis. A special three-mirror goniolens is installed on the eye. With the most popular technique today, linear trabeculoplasty, burns are applied to the area of Schlemm's canal in one row.
| Laser trabeculoplasty | Contact lens for trabeculoplasty |
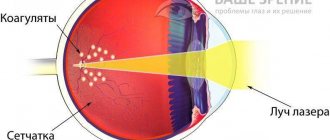
The “gold standard” for laser treatment of glaucoma is argon laser trabeculoplasty, which was proposed in 1979 by Wise and Witter. The surgical technique consists of applying laser coagulates in the projection area of Schlemm's canal using the same laser parameters.
Laser trabeculoplasty with an argon laser causes tension and shortening of the trabecular diaphragm due to wrinkling of the tissue at the burn sites, widening of the trabecular slits located in the area between the burns, and, as a result, leads to an improvement in the outflow of intraocular fluid from the eye and a decrease in intraocular pressure.
Also, argon laser trabeculoplasty helps cleanse the trabecular membrane from pigment granules and increase its permeability to intraocular fluid.
| Argon laser trabeculoplasty |
Laser trabeculoplasty with an argon laser has become so widespread due to its effectiveness. Five-year compensation of intraocular pressure can be achieved in 50% of cases, ten years - in 30% of cases. However, the operation also has its disadvantages.
The range of patients for argon laser trabeculoplasty is limited. The argon laser radiation is absorbed mainly by the pigment cells of the trabecular membrane, that is, trabeculoplasty is quite effective only in eyes with pronounced pigmentation of Schlemm's canal.
Of no small importance is the cicatricial degeneration of the trabecular area under the influence of argon laser radiation, as a result of which the trabecula becomes impenetrable to aqueous humor, the current of which is directed to adjacent, undamaged areas of the trabecula.
Repeated exposure to an argon laser leads to more intense formation of scar tissue and not only does not reduce intraocular pressure, but also worsens the course of the glaucomatous process.
Complications of argon laser trabeculoplasty include a reactive rise in intraocular pressure 1-4 hours after surgery in 30% of operated patients and after 1-3 weeks in 2% of patients. In case of repeated trabeculoplasty, the effect of the operation is observed only in 32% of cases.
In addition, the argon laser has a high cost, a bulky power supply system, poor optical-electrical efficiency and limited operating time due to degeneration of the plasma tube.
These factors force us to look for new ways to deliver laser radiation for trabeculoplasty in patients with open-angle glaucoma.
Selective trabeculoplasty
Selective trabeculoplasty is currently most widespread. The technique of selective laser trabeculoplasty is practically no different from traditional argon laser trabeculoplasty.
Pulses are applied to the trabecular area, but due to the large spot size, the interaction zone of laser radiation is the entire trabecular area, and not just the projection of Schlemm’s canal.
At the same time, selective laser trabeculoplasty does not cause thermal damage to the trabecular tissue and coagulative necrosis of its cells and collagen fibers due to the very short pulse duration.
Selective trabeculoplasty selectively acts on melanin-containing trabecular cells, leaving pigment-free cells completely intact, does not lead to burn damage to trabecular cells, and can effectively reduce intraocular pressure.
| Selective trabeculoplasty |
Selective laser trabeculoplasty is performed as an independent method of laser treatment of glaucoma in the following cases:
- in the initial and advanced stages of glaucoma with subcompensation of intraocular pressure in cases of moderate and severe pigmentation of the trabecular zone of the anterior chamber angle;
- ineffectiveness of previously performed argon laser trabeculoplasty;
- in laser treatment of patients with pseudoexfoliation glaucoma and pigmentary glaucoma.
Selective trabeculoplasty is a safe and effective procedure. Compensation of intraocular pressure is observed by the end of the first day after surgery and is stable.
Selective trabeculoplasty is a more gentle operation, provides a higher hypotensive effect compared to the argon laser procedure, has a less pronounced reactive syndrome and is effective in patients with previously unsuccessful argon laser trabeculoplasty.
Laser treatment of glaucoma. Reviews from doctors
To summarize, we can say that laser treatment of glaucoma today has no analogues in the world. Laser treatment of glaucoma when drug antihypertensive therapy was ineffective allowed many patients to preserve their vision, avoid antiglaucomatous surgery, and returned them to a full life.
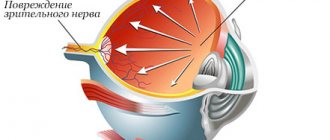
But despite the obvious advantages, using a laser also has a number of disadvantages:
- low efficiency and short duration of the hypotensive effect in advanced stages of glaucoma;
- the possibility of a reactive syndrome, accompanied by an increase in intraocular pressure in the first hours after laser intervention and with the development of an inflammatory process in the future;
- the possibility of damage to corneal endothelial cells, lens capsule and iris vessels;
- formation of scar adhesions in the area of impact - the angle of the anterior chamber, the iridectomy zone.
Laser treatment of glaucoma is effective only in the early stages of glaucoma development. In advanced and terminal stages of the glaucomatous process, laser treatment is no longer indicated due to the low hypotensive effect. We are ready to offer this category of patients an alternative to laser treatment – microsurgical treatment of glaucoma.
Source: //eyesurgerycenter.ru/glaukoma/lazernoe-lechenie-glaukomy.html
The essence of the operation
During selective laser trabeculoplasty, laser beams are selectively exposed to pigment cells in the trabecular region of the anterior corner of the eye. The operation is performed using a high-precision modern laser with a wavelength of 532 nm.
The mechanism of action of selective laser trabeculoplasty is based on the cellular activation of macrophages of pigment cells in the trabecular zone. During the procedure, due to the short-term (3 ns) selective action of laser beams, no thermal or coagulating effect is observed.
During the operation, about 50 laser point applications are applied to a limited area. The procedure guarantees a decrease in IOP levels by 6–8 mm Hg. The effectiveness of the operation is higher in patients with initial and advanced stages of glaucoma; in advanced stages of the disease, it may have an insufficient or short-term effect.
Prevention of glaucoma
Even after successful laser treatment, which has achieved a stable reduction in intraocular pressure, intraocular pressure should still be monitored every 3 months, and visual acuity, visual field and condition of the optic nerve head at least once every 6 months.
You should not work for a long time in an inclined position of the body (when the head is lower than the body, for example, as when washing floors, weeding beds, avoid excess consumption of alcohol, sweets, fatty and salty foods).
Help to avoid glaucoma:
- Moderate physical activity;
- Balanced diet;
- Timely treatment of ophthalmological diseases;
- Preventative examinations with an ophthalmologist.
Paying attention to your own health helps prevent many diseases, glaucoma being one of them. In addition, modern ophthalmology makes it possible to identify the disease at a very early stage, if the patient does not neglect preventive examinations.
Advantages
- Selective laser trabeculoplasty is performed on an outpatient basis; local drip anesthesia is used for pain relief. This avoids the additional stress on the cardiovascular system associated with the use of general anesthesia.
- Thanks to the use of the most modern equipment, selective laser trabeculoplasty is low-traumatic, painless, takes minimal time, and has a low risk of intra- and postoperative complications.
- If there are indications, the operation can be repeated.
- During the operation, the laser does not damage the surrounding tissue, acting exclusively on the selected area.
- The technique is a worthy alternative to medical and surgical treatments for glaucoma, as well as other laser treatment methods (such as argon laser trabeculoplasty).
Pros of the procedure
The advantage of the operation is its painlessness and precision, which does not damage healthy tissue.
Trabeculoplasty has all the advantages of laser ophthalmological operations and shows high efficiency, providing a stable hypotensive result. When performed by qualified medical personnel using modern equipment, the intervention has no negative consequences. The advantages of the laser correction method are as follows:
- painlessness;
- high precision surgery ensures no injury to healthy tissue;
- short duration of the operation;
- bloodlessness;
- fast rehabilitation.
The advantage of trabeculoplasty over medical conservative treatment is the stability of the hypotensive effect. In most cases, a single procedure is sufficient for the patient. If further degenerative processes are detected and intraocular pressure increases, repeated use of the laser is allowed to consolidate the achieved hypotensive result.
Possible complications
After selective laser trabeculoplasty, the following complications may occur:
- postoperative infectious complications (keratitis, conjunctivitis) may occur in 3–5% of cases;
- allergic inflammation (itching, burning, swelling, redness of the mucous membrane of the eye);
- short-term increase in IOP level (on days 1-7 after surgery);
- insufficient effectiveness of the procedure (in approximately 12% of patients), which requires further surgery.
Undesirable consequences
If eye care recommendations are not followed during the rehabilitation period, pathologies such as conjunctivitis may develop.
Trabeculoplasty extremely rarely causes eye complications. Postoperative negative effects include allergic and inflammatory reactions, which can occur 3-5 days after the procedure if the rules of visual rehabilitation care are not followed. The following local complications are recorded in patients:
- conjunctivitis;
- keratitis;
- allergic reaction to eye drops;
- short-term (3 to 5 days) increase in intraocular pressure.
In medical practice, there are cases when an operation does not bring the desired result, even if it was successfully performed. IOP does not decrease. The statistical error of inefficiency is no more than 1%. The reasons for the phenomenon are unknown, however, with the help of repeated laser correction it is possible to achieve a decrease in intraocular pressure to 5 mm Hg. Art. The operation is performed in the clinic after diagnosis and consultation.
Advantages of treatment at MGK
"Moscow Eye Clinic" provides high-quality medical care for patients with various eye pathologies. At the clinic, you can undergo a comprehensive diagnostic examination, receive a comprehensive consultation with a specialist, undergo a course of medication or hardware treatment, and, according to indications, laser and surgical treatment of eye pathologies of varying degrees of complexity is carried out.
The vast professional experience of our specialists and the use of the most modern equipment allow us to minimize possible complications of treatment. In particular, when performing laser operations, the latest generation PurePoint laser from Alcon is used, which allows you to achieve the maximum possible treatment results. Leonid Grigorievich Estrin, a doctor of the highest category with more than 30 years of experience, deals with laser treatment methods at the clinic.
Selective laser trabeculoplasty in the MGK is performed on an outpatient basis, without the use of general anesthesia. The operation is painless, low-traumatic, has a stable effect, a short recovery period and low cost.
Postoperative period
After the operation, the ophthalmologist determines intraocular pressure and prescribes anti-inflammatory eye drops and antiglaucomatous drugs. Days of follow-up visits are required to monitor the effectiveness of treatment and measure intraocular pressure. After trabeculoplasty, you may experience blurred vision and increased sensitivity to light, which may persist for two days after surgery. There should be no discomfort or pain.
Cost of treatment
The price of laser trabeculoplasty is only 10,500 rubles per eye. We also remind you that the patient can partially return the funds spent and take advantage of tax deductions in accordance with Russian legislation. We provide all the necessary documentation for this. You can read more about returns here.
All questions you are interested in can be asked to specialists by phone and (499) 322-36-36 or online, use Skype consultation on the website, in addition you can read the “Prices” section.
Go to the “Prices” section
Dagaev Adam Huseinovich