The vitreous body is a substance with a semi-liquid gel-like texture.
On the outside it is covered by the cornea, and on the inside it is connected to the retina through a hyaloid membrane.
In newborns, this substance is homogeneous, but over time, due to natural processes occurring in the body, it is gradually divided into two parts: liquid and dense fibrous, connected by protein compounds.
When the membrane tissue is partially destroyed, the liquid part seeps under it, collects in the lumen and casts a shadow on the light-sensitive retina. This phenomenon is accompanied by the appearance of “flies” and flickering dots before the eyes, since the liquid contains dense, opaque particles. In most cases, this process does not affect the clarity of vision and does not entail defects or complications.
Causes
The destruction of the vitreous body is most often a consequence of natural aging of the body. This is due to the fact that the substance mostly consists of collagen, the production of which decreases with age. In addition, the disease can result from:
- high myopia;
- hormonal disorders and diseases;
- inflammation of the choroid and retina;
- various head injuries;
- physical and psychological exhaustion;
- excessive visual load;
- radiation, exposure to chemicals or toxins;
- previous eye surgeries;
- diseases of the vascular system.
Causes of PVD
Newborns have a homogeneous structure of the vitreous body, which fits tightly to the retina. As the body ages, the tissues of the vitreous body are divided into 2 fractions - liquid (almost water) and fibrous, which is protein molecules glued together - it is this that peels off from the retina. This process is very common and, as a rule, not dangerous. PVD is typical for almost every person. However, with myopia, this phenomenon is especially common and occurs earlier by about 10 years, compared to people with normal vision. However, it is believed that PVD occurs somewhat more often in women, which is associated with hormonal changes inherent in menopause.
Posterior detachment has different heights, lengths and shapes, and can be complete or partial. The vitreous body is firmly attached to the retina in several places. Age-related liquefaction usually provokes a complete posterior vitreous detachment, which is detected along the entire length of the posterior pole of the eye, and has a more or less pronounced shift to the center. In this case, there is a separation of the vitreous body from the optic nerve head, which does not cause damage to the retina, while the subvitreal space is filled with intraocular fluid.
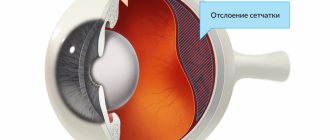
Partial PVD, with the attachment of vitreous fibers to the retina in several places (fixation points), is the most dangerous, as it is associated with a large number of complications that occur with this condition. When the vitreous body decreases in volume, which occurs due to abnormal growth of the eye (usually caused by myopia), inflammation or injury, partial detachment from the retina often occurs. Due to excessive traction of the entire mass of the detached body, as well as swaying of the vitreous body during eye movements, a hole in the retina or its complete detachment in limited areas may occur. When a retinal tear occurs, fluid from the space in the vitreous begins to leak through the hole, flowing between the retina and the back wall of the eye. This aggravates the process by separating the retina from the back wall of the eye, causing retinal detachment.
Risk group
The disease mainly occurs in people over 45 years of age, with women at this age suffering from this disease more often than men. Experts attribute this to hormonal changes during menopause.
In addition, the following are at risk of developing the disease:
- athletes (due to injury risk);
- welders, construction workers and factory workers;
- people who have had eye surgery;
- people with penetrating eye trauma.
Classification
Experts distinguish three main types of detachment, which differ from each other:
- Partial detachment. It is a consequence of thrombosis, penetrating injury, hemorrhage in the retina, its inflammation, as well as inflammation of the choroid. This type of detachment is uncommon, but can gradually become complete.
- An annular detachment is a separation of the vitreous from the optic disc.
- Complete detachment. The cause may be inflammation of the choroid and hemorrhage in the space between the vitreous body and the retina. The risk group for this type of detachment includes people under 35 years of age.
Effective preventive measures
Vitreous detachment can lead to serious complications. Yes, the prognosis for treating the anomaly is favorable. It can be easily corrected, but only if identified at the initial stage. If retinal detachment is diagnosed and other severe consequences of the disease develop, then therapy may be powerless.
The essence of preventive measures is to reduce the risk of complications. Pathologies such as diabetes or thyroid problems must be properly treated in a timely manner. Also periodically give your eyes rest, this is especially important for people who spend a lot of time at the computer.
| If the work involves possible damage to the organ of vision, be sure to use safety glasses and other devices. |
Posterior vitreous detachment
The disease manifests itself in different ways. Cloudiness may occur, which is clearly visible when looking at a plain light background. Most often, over time, the “front sights” fall below the optical axis and disappear. In addition, the patient may see flashes of light similar to lightning. They are especially visible if you close your eyes.
This phenomenon occurs due to the fact that the vitreous body begins to exert a pull on the retina where they are most strongly connected. As a result of the impact, they are perceived by photoreceptors as a bright flash of light.
"Flying Flies"
“Flying flies” are morphologically based on cellular accumulations in the form of tiny opacities. Since the transparency of the vitreous body is ensured by several barriers (the walls of the retinal vessels, the internal limiting membrane, the cortical layer of the vitreous body), if the barrier functions of these structures are disrupted, cellular elements of the blood can enter the vitreous body. Most often, the symptom of “flying flies” occurs in old age with cardiovascular pathology or retinal pathology.
Symptoms
In addition to harmless symptoms, there are also those that signal the danger of the exfoliation process:
- sudden deterioration of vision;
- the appearance of a curtain that blocks the field of view partially or completely;
- a sharp increase in various opacities;
- persistent flashes and floaters.
If you have these symptoms, it is important to quickly contact an ophthalmologist so that he can carry out diagnostic procedures to identify the cause of the disease and prescribe the appropriate treatment.
Diagnosis of the disease
If you suspect a retinal deformation, go to the clinic for a full visual diagnosis. By consulting a doctor in a timely manner, you can stop impending problems. The scale and nature of detachment are determined by the following methods:
- defining visibility fields;
- visual examination;
- determination of the degree of visual acuity;
- biomicroscopy of the pupil;
- fundus diagnostics;
- Ultrasound;
- determination of the integrity of the optic nerve;
- visometry;
- optical coherence tomography;
- tonometry;
- laboratory research.
Diagnosis begins with a standard medical examination. After this, instrumental and biochemical diagnostic methods are added. The doctor determines the direction of treatment. Laboratory diagnostic methods are recommended in cases where the patient is about to be admitted to the hospital.
Diagnostics
The disease can be detected by studying anatomical transformations in the eyes and their consequences. To do this you can do:
- refractometry (determination of eye refraction);
- tonometry (measurement of eye pressure);
- ophthalmoscopy (examination of the fundus of the eye);
- ophthalmometry (measurement of the radius of curvature of the cornea);
- visual acuity test;
- biomicroscopy (study of optical media and eye tissues).
The anteroposterior axis of the eye is also checked. If its value exceeds 24 mm, then the risk of detachment is high. Ultrasound of the eyeball can reveal transformations in the structure, detect voids and compactions, as well as detachment and stretching of the retina.
Optical computed tomography will help to detail the clinical situation. Thanks to it, it is possible to more accurately examine the structure of the retina, measure the thickness of the posterior hyaloid and internal limiting membranes.
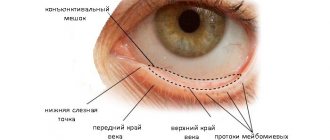
Posterior hyaloid membrane and its properties
The posterior hyaloid membrane (PHM) plays an important role in the structure of the vitreous body, as one of its boundary layers. Some experts argue that normally this boundary layer should not exist. There are only isolated high-density collagen fibers of the vitreous body (VT) in the area adjacent to the retina (the so-called posterior boundary layer). According to them, PGM is formed only in the case of posterior CT detachment, due to the morphological changes that occur.
In fact, the posterior limiting membrane of the CT, the posterior hyaloid membrane, is a structure that surrounds the cortex of the posterior vitreum and firmly attaches the circumference of the optic disc to the underlying tissues at the base of the vitreous. The SGM has a strong connection with certain vessels of the retina, is firmly attached around the macula, as well as in the area of attachment of the oblique muscles to the sclera.
The PGM is relatively weakly connected to the rest of the retinal surface. In young healthy people, the vitreous body has a normal structure, and the posterior halide membrane is attached throughout its entire length to the internal limiting membrane of the retina.
For a variety of reasons, the MLM sometimes separates from the underlying retinal internal limiting membrane. The separation can be complete or partial, which entails its detachment, i.e. posterior vitreous detachment (PVD).
The frequency of such detachments increases with age, and in people over 50 years of age reaches 53% of cases, and in the age group 65 years and older - 65%.
In myopic patients, PVD develops on average 10 years earlier than in people with normal vision and farsighted people. Its risk is also slightly higher in women.
Treatment
In most cases, no treatment is required. If the disease proceeds without complications, the exfoliated fibers fall below visibility, and the symptom in the form of “floaters” goes away on its own. But ophthalmologists can prescribe an additional course of strengthening medications:
- Wobenzym in tablets helps relieve inflammation, pain and swelling, and also strengthens the immune system and resolves blood clots;
- Taufon - drops that are used to stimulate metabolic processes in tissues and accelerate regeneration;
- Emoxipin is an antioxidant that strengthens blood vessels in the retina and mucous membrane of the eye and improves tissue nutrition;
- Potassium iodide is a 2% solution that has an antisclerotic effect and accelerates the resorption of hemophthalmos.
In addition, you need to protect your eyes from bright sunlight, refrain from visual stress and give your eyes a rest every 30 minutes spent at the computer or reading. During breaks, it is recommended to do eye exercises.
In case of a sharp drop in visual acuity and a high risk of complications, surgery is prescribed. There are two methods of surgical intervention, from which the specialist chooses the most suitable one, based on the specific case:
- Vitrectomy – removal of the vitreous body: complete or partial. Instead, the space is filled with a special saline solution. Possible side effects and risks: glaucoma, cataracts, extensive hemorrhage.
- Vitreolysis – YAG laser radiation. With its help, the vitreous body is processed to change its properties and restore transparency. Side effects and risks: damage to the structure of the eye, development of various types of hemorrhages.
These methods are complex and can lead to new vision problems, but there are cases in which surgical intervention is necessary.
Prevention
Attention to existing eye ailments and their timely treatment will help prevent the disease. It is important to maintain normal hormonal levels in case of diabetes and thyroid pathologies. In addition, you need to take care of the safety of your eyes and protect them from injury. For example, when welding, wear special safety glasses.
To prevent various complications and visual impairment in the presence of vitreous detachment, you need to stop smoking and drinking alcoholic beverages, and follow the prescribed diet.
Types and types of PVD
Experts subdivide PVD by height, length, and shape. In addition, detachments are divided by volume into complete and partial.
The attachment of the vitreous body to the retina is localized at several fixation points. When CT liquefies due to old age, which is an irreversible physiological process, complete posterior detachment is especially common. It is detected in the region of the posterior pole of the eye, along its entire length, with a shift to the center, which has different severity. In this case, the vitreous body is detached from the optic nerve head without damaging the retina, and the fluid fills the subvitreal space, which is not dangerous.
Partial PVD is much more dangerous. The vitreous body, in this case, in certain places remains attached to the retina by fixation points, which can lead to serious complications.
Thus, when the volume of the vitreous body decreases due to pathological growth of the eye (typical of myopia), trauma or an inflammatory process, the volume of the vitreous body also decreases. This can cause partial detachment from the retina. The reason is the excessive pull of the mass of the detached vitreous body, which sways when moving the eyes, onto the retina at the places of its attachment, which leads to its separation or the occurrence of local ruptures. In this situation, the aqueous fluid present in the space of the vitreous body penetrates through the resulting hole into the area between the retina and the back wall of the eye. Gradually, the retina separates from the back wall of the eye to varying degrees - its detachment occurs.
Retinal detachment is a dangerous condition that can lead to blindness. It requires emergency surgery. To ensure that prompt assistance is not required at the most inopportune moment, it is necessary to carry out constant ophthalmological monitoring for the seemingly harmless condition of PVD.
Therefore, people who observe signs of posterior vitreous detachment (floating interference in the field of vision) and, especially those who have encountered the phenomena of “lightning” or “sparks”, should definitely schedule a visit to an ophthalmologist as soon as possible.
Retinologists at our clinic have extensive experience in treating pathologies of the retina and vitreous body. If there is no threatening condition with PVD, the patient will be offered a regimen of conservative therapy aimed at reducing the severity of visual interference.
For retinal tears and detachments, laser or surgical treatment of the pathology may be offered. To do this, the clinic has collected all the necessary diagnostic and surgical equipment from the world's best manufacturers, and specialists regularly undergo training in the most progressive ophthalmological clinics in Russia and abroad.
Useful video
You can learn more about the disease and its causes from the following videos.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2031
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 1 ratings, average: 5.00 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.