Structure
The structure of the eyelids is very interesting and unique. Each part is responsible for many functions. The functionality and structure of these amazing muscles should be studied in detail. The eyelids cover the outer part of the eyes and protect from external factors. Main functions:
- protection against the ingress of small particles and foreign objects;
- uniform distribution of tear fluid;
- responsible for moisturizing the cornea and conjunctiva;
- washes away small particles from the surface of the mucosa;
- protect eyes from drying out during sleep;
- are responsible for the blinking process.
The edges of the eyelids are 2 mm thick. The lower and upper eyelids close tightly when closing the eyes. Eyelashes grow on the smoothed anterior rib. The inner one is sharper and fits tightly to the eyeball. The intermarginal space is located along the length of the eyelids between the anterior and posterior parts. The skin is thin, so it tends to gather in folds. When the eyes open, it folds inward with the help of the muscles that are responsible for raising the eyelids. This creates a deep crease. Another less pronounced one is located on the lower eyelid.
There is also a circular muscle, which is located under the skin in the orbital or palpebral part. In the process of closing the eyelids, both muscles contract. The dense tuft that emanates from the frontal origin of the maxilla is the internal ligament of the eyelid. It bifurcates and connects to the ends of the cartilage of the eyelids.
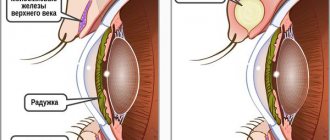
The detailed structure of the eyelids is presented in this image:
Classification and reasons
Muscle weakness can be acquired or congenital. Congenital ptosis of the upper eyelid is a disease of young children, its causes are underdevelopment or absence of the muscles that lift the eyelid, as well as damage to the nerve centers. Congenital ptosis is characterized by bilateral damage to the upper eyelid of the right and left eyes simultaneously.
Watch an interesting video about the congenital form of the disease and treatment methods:
Unilateral lesions are characteristic of acquired ptosis. This type of ptosis develops as a complication of another, more serious pathological process.
Classification of ptosis of the upper eyelid depending on the cause of its appearance:
- Aponeurotic blepharoptosis – excessive stretching or relaxation of muscles, loss of tone.
- Neurogenic ptosis is a violation of the passage of nerve impulses to control muscles. Neurogenic ptosis is a symptom of a central nervous system disease; the appearance of neurology is the first signal for additional examination of brain structures.
- Mechanical blepharoptosis is post-traumatic muscle damage, tumor growth, and scarring.
- Age-related – the natural physiological processes of aging of the body provoke weakening and stretching of muscles and ligaments.
- False blepharoptosis – observed with a large volume of skin folds.
Other causes of blepharoptosis in adults include:
- damage, bruises, ruptures, eye injuries;
- diseases of the nervous system or brain: stroke, neuritis, multiple sclerosis, tumors, neoplasms, hemorrhages, aneurysms, encephalopathy, meningitis, cerebral palsy;
- paresis, paralysis, ruptures, muscle weakness;
- diabetes mellitus or other endocrine diseases;
- exophthalmos;
- a consequence of unsuccessful plastic surgery, Botox injections.
By stages:
- partial;
- incomplete;
- full.
Ptosis has 3 degrees, which are measured in the number of millimeters of distance between the edge of the eyelid and the center of the pupil.
In this case, the patient’s eyes and eyebrows should be relaxed and in a natural position. If the location of the edge of the upper eyelid coincides with the center of the pupil, this is the equator, 0 millimeters. Degrees of ptosis:
- First degree – from +2 to +5 mm.
- Second degree – from +2 to -2 mm.
- Third degree – from –2 to –5 mm.
Orbicularis oculi muscle
Drooping eyelids are a cosmetic problem. The orbicularis oculi muscle belongs to the superficial muscles of the facial area. Being associated with the superficial musculoaponeurotic structures, the muscle moves the overlying tissues through fibrous septa extending from the aponeurotic structures to the dermis.
The orbicularis oculi muscle can be arbitrarily divided into an ocular and palpebral part, the latter being further divided into two parts. The palpebral part of the muscle is associated with the function of blinking and voluntary winking, and the ocular part is used for voluntary squinting.
The muscle is innervated by the temporal and zygomatic branches of the facial nerve. The nerve fibers are oriented horizontally and innervate the muscle fibers from the lower surface.
The ocular part of the muscle is located around the palpebral fissure. It interacts with other muscles of the facial area. This part of the muscle has a curved direction from the medial canthal margin to the maxillary process of the frontal bone, the medial palpebral ligament and the frontal process of the maxilla.
Levator of the upper eyelid / Muscles of the eye / Accessory apparatus / Anatomy of the eye / page
, supercilium. A thick, transversely oriented ridge of skin covered with densely arranged hair. Rice. A.
2.
Eyelid fold, ]
, plica palpebronasalis]. Continuation of the upper eyelid at the lateral wall of the nose. Covers the medial corner of the eye. Rice. IN.
7.
Posterior surface of eyelid
, facies posterior palpebralis. Covered by the conjunctiva, which contains diffusely scattered goblet cells. Rice. D.
8.
Lateral commissure of the eyelids
, commisura palpebralis lateralis. The junction of the upper and lower eyelids at the lateral corner of the eye. Rice. A.
10.
Medial canthus
, angulus oculi medialis. The rounded corner of the palpebral fissure, which limits a triangular space - the lacrimal lake. Rice. A.
13.
Upper eyelid cartilage
, tarsus superior. A curved plate approximately 10 mm high, part of the upper eyelid. It is formed by dense coarse fibrous connective tissue and contains the secretory sections of the glands of the cartilage of the eyelid. Rice. B, Fig. D.
17.
Lower eyelid cartilage
, tarsus inferior. A curved plate about 5 mm high as part of the lower eyelid. It is formed by dense coarse fibrous connective tissue and contains sectoral sections of the glands of the cartilage of the eyelid. Rice. B, Fig. D.
18.
Medial ligament of the eyelid
, lig. palpebrale mediale. Connective tissue cord between the cartilages of the eyelids and the medial wall of the orbit. Passes in front of the lacrimal sac. Rice. B, Fig. G.
19.
Lateral suture of the eyelid
, raphe palpebralis lateralis. A thin cord split off from the lateral ligament of the eyelid, in the formation of which fibers of the orbicularis oculi muscle take part. Rice. G.
20.
Lateral ligament of the eyelid
, lig. palpebrale laterale. Directed from the lateral edges of the eyelids to the lateral wall of the orbit in front of the orbital septum. Rice. B.
21.
Eyelid cartilage glands]
, glandulae tarsales]. Tubular holocrine glands, the secretory part of which is immersed in the cartilage of the upper and lower eyelids. Their excretory ducts open near the posterior edge of the eyelids. They secrete a sebaceous lubricant that prevents tears from overflowing over the edge of the eyelid. Rice. D.
22.
Superior eyelid cartilage muscle
, m.tarsalis superior. Unstriated muscle fibers located near the junction between the aponeurosis of the m.levator palpabrae superioris and the cartilage of the upper eyelid. Rice. D.
23.
Lower eyelid cartilage muscle
,mm. tarsalis inferior. Smooth muscle fibers located between the lower fornix of the conjunctiva and the cartilage of the lower eyelid. Rice. D.
24.
Conjunctiva
, tunica conjunctiva.
Covers the inner surface of the eyelids and consists of double-layered or stratified columnar epithelium with goblet cells, loose connective tissue (lamina propria), in which clusters of lymphocytes are identified, as well as numerous blood vessels. In the area of the fornix, the conjunctiva passes from the eyelids to the eyeball, where the epithelium covering it becomes multilayered squamous. In the region of the edge of the cornea, the conjunctiva passes into its epithelium. Rice. D.
25.
Semilunate fold of conjunctiva
plica semilunaris conjunctivae. Located in the medial corner of the eye between the upper and lower fornix of the conjunctiva. Rice. E.
26.
Lacrimal caruncle
, caruncula lacrimalis. Elevation in the medial corner of the eye, covered with stratified squamous or columnar epithelium. Rice. E.
Symptoms
In many cases of ptosis of the upper eyelid, its mobility is significantly reduced or its mobility is completely absent. A drooping upper eyelid leads to vision difficulties. Therefore, the patient gets used to the position of raised eyebrows.
With significant drooping of the eyelid, most often in children, a forced pose appears - “stargazer's head”. It is characterized by an elevated head position and a wrinkled forehead.
Ptosis of the upper eyelid in a child disrupts the normal development of the visual analyzer and leads to the development of many visual disorders.
Signs of the disease include eye irritation, double vision, and fatigue due to prolonged muscle tension. In cases where it is impossible to completely close the eye, the patient develops symptoms of dry eye, chronic keratitis (inflammation of the cornea of the eye) and conjunctivitis (inflammation of the conjunctiva of the eye) develop.
In rare types of ptosis, additional symptoms appear. So, a sign of Marcus-Gunn syndrome is the disappearance of drooping eyelids when the jaws are tightly clenched or the mouth is opened.
Functions[ | ]
The orbital part (lat. pars orbitalis) narrows the orbital fissure, forms folds in the circumference of the orbit and smoothes out transverse folds in the skin of the forehead. Century part (lat.
pars palpebralis) during contraction closes the eyelids, while the upper tufts pull the skin of the eyebrows down, the lower tufts pull the skin of the cheeks up. The lacrimal part (lat. pars lacrimalis), with its contraction, expands the lacrimal sac and lacrimal canals, facilitating the drainage of tear fluid [2][3][5][6].
Contracting as a whole, the muscle closes the eyes, while the skin around the eyes forms radial folds[4].
Remove drooping upper eyelids. Exercise for the muscle that lifts the upper eyelid
Bartsok-gymnastics course for the face
To prepare and perform the exercise, you need a mirror, attention and careful monitoring of the progress of the workout, and, of course, the desire to achieve your goal. To learn how to perform the exercise correctly, it may take you anywhere from a few minutes to an hour.
Completing the exercise in the future will take no more than a minute or a minute and a half when using audio support.
What this exercise can help you do:
- prevent or remove drooping upper eyelids;
- improve vision and light perception, maintain or restore the natural field of vision.
If mastering the exercise on your own will cause difficulties, take advantage of the opportunity of distance learning and take the lesson you need via Skype or ask any questions you are interested in via the site’s email.
We will not train the facial muscle. This is a muscle of the eyeball, innervated by the same nerve as the extraocular muscles, but its close connection with the skin leads to a huge influence of the muscle on the condition of the skin of the upper eyelid.
The levator palpebrae superioris muscle opens the eyes and is located at the top of the upper eyelid under a cushion of fat. At the site of attachment of the muscle, folds form on the upper eyelids when the eyes are open. When a muscle weakens, it sags and the folds increase.
Of course, one should not confuse sagging of the upper eyelid as an age-related process and swelling of the upper eyelid, which may be associated with problems with cardiovascular activity.
Training the levator palpebrae superioris muscle will not only help tighten the upper eyelid, it should lead to greater eye opening, improve the perception of light by the sclera of the eyes, improve blood circulation in the eye area, promoting good vision. But the main thing is that it will restore the normal position of the muscle, stop the stretching of the skin of the eyelids and help stop the sagging of the skin, tighten or completely remove drooping upper eyelids.
Preparing for the exercise
To reduce or remove drooping upper eyelids, you need to learn how to lift your upper eyelids high to strengthen the muscle. Look at yourself in the mirror. Dim the lights.
Since you will be opening your eyes more than usual, eyes that are not used to this may feel uncomfortable at first. Looking at yourself in the mirror, lift your upper eyelids as if you want to push them under your forehead bone (or under your brow ridge).
Above the iris of the eyes, at least a small white stripe of the sclera, the white of the eye, should be visible.
Try not to strain or push your eyes forward: you raise your upper eyelids without bulging your eyes. Eye bulging is not related to this muscle and will not help you tighten your upper eyelid.
Try to keep your eyes relaxed, as if immersed inward.
If this doesn’t work, read the biologically active text “Look without getting tired” or listen to the audio recording “Immersion of the Eyes”.
Peculiarities
The muscle is striated. The upper muscle is surprisingly smooth and is called the tarsal muscle. Functions with the help of fibers of the cervical nodes. In the treatment of Sudeck atrophy, the risk of blockade of such nodes increases. The occurrence of paresis leads to drooping of the upper eyelid. Against this background, ptosis occurs.
Ptosis is a pronounced pathology, which is accompanied by drooping of the eyelid (mainly the upper one). In most cases, the disease is unilateral. Bilateral lesions are rarely observed. Asymmetry of the eyelids not only causes an aesthetic defect, but can also impair vision. In a pronounced form, severe ophthalmological diseases can develop.
The muscle is attached to the orbit of the superior cartilage. The beginning is the area of the optic opening. It passes into a tendon, the width of which is much greater. Its anterior part is attached to the cartilage and goes to the orbicularis muscle. The fibers, which are located on the back, connect to the conjunctiva and pass into the upper fold. The fibers are located on the middle part of the tendon. They complete the structure of the muscle.
The muscle that raises the eyelid is closely related to the levator muscle. It is located near its front end. In addition, this structure ensures the elevation of not only the eyelid, but also all its parts: cartilage, skin, conjunctiva, which passes into the upper fold.
The innervation of the middle part of the upper eyelid has smooth fibers. Therefore it is considered a sympathetic nerve. The posterior surface is completely covered with conjunctiva connected to cartilage. If the levator tone is normal, then the upper eyelid covers the cornea by about 2 mm. The function that is responsible for raising it is impaired with ptosis.
Interestingly, the levator is surrounded by a slight layer of adipose tissue. In addition, the trochlear, frontal nerves and arteries are located there. This separates it from the apex of the orbit.
It is very easy to distinguish the levator muscle from the superior muscle. They are connected by a fascial membrane. They are also innervated by a branch attached to the optic nerve. It passes into the inferior muscles and is located approximately 12 mm from the top of the orbit. The nerve trunk approaches the levator. The back of the top edge connects to the tissue that supports the eyeballs. In medicine it is called the ligament of Withnell. Features a strong connection. They can only be separated in one place - in the center.
This ligament passes under the oblique muscle at the back. It then mixes with the fascia and covers the area above the eye. From the outside it is attached to the capsule of the lacrimal gland. The main function limits muscle displacement on the posterior side. This theory is confirmed by the localization of such functionality. When tense, the ligament supports the upper eyelid. If this function is not performed, ptosis will appear.
The distance from the transverse ligament to the cartilage is a maximum of 20 mm. The levator is responsible for creating a wide-shaped fibrous cord. It connects to the eye socket. The ligaments are divided into internal and external horns. They are rigid and support the upper eyelid in the correct position with the help of fixation. Also responsible for the blinking process.
The horn is a combination of fibrous tissues that have a very powerful effect. Located in the lower part of the eye socket on the outside of the eyelid. If you do not pay attention to such features and do not perform surgery on time, ptosis may develop. The inner horn resembles a film. Localized over the tendon of the superior oblique muscle. Performs no less important functions. Abnormal development can cause the development of ophthalmic pathologies.
The levator consists of tendon fibers. They are woven into the connective tissue of cartilage. At the moment of muscle contraction, the eyelid rises. The eyelids are well equipped with blood vessels. When the vessels divide into branches, peculiar arterial arches appear. They are located behind a certain pattern. One goes under the lower eyelid, and two go above the upper. The functionality of each structure is very important. The work of all the muscles that are responsible for raising and lowering the eyelids depends on each part.
Levator muscle of the upper eyelid in Latin
Translated from Latin, this name has the following meaning: levare - to raise, palpebral - century-old, superior - upper.
Considering its location and innervation, this muscle is usually classified as an orbital muscle. It is unusual in that it contains visceral and somatic muscle fibers, and is considered to be an antagonist of the eyelid portion of the entire orbicularis oculi muscle, causing palsy of the levator muscle to promote drooping of the eyelid over the eyeball.
The muscle that lifts the upper eyelid - functions and features
- Its origin is at the bottom of the orbit (lesser wing of the sphenoid bone).
- The place of attachment is the skin and tarsal cartilage.
- Innervation is bilateral. The superior branch goes through the oculomotor nerve and enters the levator, which is located below at the very border of the middle 3rd and posterior branches 13 mm from the apex of the orbit.
- Blood supply - lateral artery (branch related to the ophthalmic artery); supraorbital artery (from the internal carotid artery); ethmoidal posterior artery and arterial peripheral arch.
- The length of the aponeurosis is from 20 to 40 mm, the abdomen - maximum 40 mm.
Clinical features
This muscle is striated, innervated by the third pair of cranial nerves .
The superior tarsal muscle is very smooth and innervated by sympathetic postganglionic fibers from the cervical ganglion.
In the treatment of sympathetic reflex dystrophy (Sudek's atrophy), blockade of this node will affect the drooping of the ipsilateral eyelid. When the muscle is paresis, the upper eyelid also droops. Paresis leads to ptosis.
Ptosis is a pathology in which drooping of the eyelid develops.
The most common cases are unilateral ptosis, but cases of drooping eyelids on both sides are possible. When ptosis of the upper eyelid occurs from 1.5 to 2.0 mm, an asymmetrical position of the eyelids occurs, which represents a problem from an aesthetics perspective. In severe cases of ptosis, the pupil is closed by the eyelid, which can lead to visual impairment.
Functions
- raises the eyelid;
- takes part in blinking;
- controls the width of the palpebral fissure (however, the width of the palpebral fissure is most precisely controlled by the sympathetic nervous system and tarsal muscles);
- is an active muscle when awake.
Structural features
This muscle is attached to the orbital superior edge of the cartilage. It starts from the periosteum , which is located in the area of the optic opening. It goes forward along the wall of the orbit, slightly approaching its upper edge, and neatly passes into the tendon, the width of which differs in size in a larger direction.
The anterior fibers of the tendon are attached to the cartilage and directed to the palpebral bundle of the main orbicularis oculi muscle, as well as to the skin of the eyelid itself. The fibers of the posterior part are attached to the conjunctiva of the transitional superior fold.
As for the fibers of the middle part of this tendon, they are also attached to the cartilage and are the end of the muscle. The muscle itself, which raises the upper eyelid, has a close connection with the levator and is located at its anterior end.
With such a harmonious distribution of tendons, the simultaneous lifting of all components of the eyelid is ensured, namely: cartilage, skin and conjunctiva of the transitional upper fold.
This distribution is usually called three portions of muscles. In other words, the muscle that lifts the upper eyelid provides simultaneous movement of the eyelid through cartilage (this is the middle portion), the conjunctival superior fornix (posterior portion) and skin (anterior portion).
As for the innervation, the middle part consists of fibers of distinctive smoothness and is the sympathetic nerve, while the other two legs are the oculomotor nerve.
The rear surface of the eyelid is covered with conjunctiva, which is tightly fused with cartilage.
The upper eyelid, with correct levator tone, occupies a position that promotes corneal closure by 2 mm. The function of the "elelevator" may be impaired due to ptosis , as well as due to flattening of the orbitopalpebral superior sulcus.
The movement of the muscle is located lateral to the superior oblique muscle and slightly superior to the rectus muscle. Anterior to the superior part of the orbit, the entire levator is surrounded by a thin layer of fatty tissue and accompanied by the superior orbital artery, trochlear and frontal nerves. These nerves separate the levator muscle from the roof of the orbit.
The rectus superioris muscle and the levator of the eyelid are separated from each other quite easily, despite the fact that they are in close proximity; but not in the medial part, there they are connected by the fascial membrane.
These muscles equally emerge from the mesoderm and are innervated by a branch that belongs to the oculomotor nerve. The nerve enters the muscles from below at a distance of approximately 12 mm from the apex of the orbit.
The nerve trunk can also approach the levator muscle on the other side of the rectus muscle.
Attached to the levator on the posterior side of the superior edge of the orbit is a small area of fibrous dense tissue that supports the eyeball. This tissue is called the superior transverse ligament of Withnell.
The connection between the levator and the posterior aspect of the superior edge of the orbit is very strong; in the inner and outer parts especially, this means that they can only be separated in areas located in the center.
On the medial side, the Withnell ligament ends closer to the trochlea, but still passes under the appearance of fibrous cords under the superior oblique muscle posteriorly, after which it mixes with the fascia that covers the supraorbital notch. Externally, the ligament of Withnell connects the fibrous capsule of the lacrimal gland and the periosteum of the frontal bone.
Withnell believes that the main function of his ligament is to limit the displacement (tension) of the muscle on the posterior side.
The author of his theory put forward this assumption, based on the localization and distribution of this function, as an analogue of the limiting ligaments of the external muscles. He thought there were similarities.
By straining, the ligament helps support the upper eyelid. If it is destroyed, the levator of the eyelid will become sharply thickened and ptosis will occur inside.
From the transverse ligament to the very bottom of the cartilaginous plate, the distance is from 14 to 20 mm; from the levator aponeurosis to the skin circular insert - no more than 7 mm.
The levator aponeurosis, in addition to the palpebral insert, forms a fibrous cord (quite wide), which attaches to the edge of the orbit behind the external and internal ligaments of the eyelid.
These ligaments are called: internal “horn”, external “horn” .
Due to the fact that they are rigid, during the period of levator resection, the supporting function of the upper eyelid in the correct position is noted by fixing the “horn” with an additional instrument.
The external “horn” is a bundle of fibrous tissue that differs in power and in some places divides the inner part of the lacrimal gland into two parts.
It is located below, attached in the area of the tubercle of the orbit from the outside to the external ligament of the eyelid.
If this anatomical feature is not taken into account and, if necessary, surgery is performed to remove the tumor of the lacrimal gland, ptosis (of the lateral part of the eyelid) may occur.
The internal “horn,” on the contrary, is thin and film-like . The location of this film is over the tendon of the superior oblique muscle, towards the internal ligament of the eyelid and towards the posterior lacrimal crest.
As for the fibers of the levator tendon of the upper eyelid, they are woven into the connective tissue of the cartilaginous plate at the third level. When the muscles contract, the eyelid rises, as a result of which the preaponeurotic eyelid shortens and the postaponeurotic eyelid lengthens.
In general, the eyelids are well vascularized by branches of the ophthalmic artery in the internal carotid artery system and anastomoses of the maxillary and facial arteries in the external carotid artery system. When these vessels branch, arterial arches are formed, one in the lower eyelid and two in the upper.
source
muscle that lifts the upper eyelid - (m. levator palpebrae superioris, PNA, BNA, JNA) see List of anat. terms ... Big medical dictionary
CRYPTOPHTHALMUS - (from the Greek kryptos hidden and ophthalmos eyes), a congenital malformation in which the eyeball is covered with skin continuously stretched over it from the cheek to the forehead. Sometimes in place of the palpebral fissure there is a rudimentary hole, sometimes... ... Big Medical Encyclopedia
Accessory organs - The eyeball has mobility thanks to the muscles of the eyeball (mm. bulbi). All of them, except for the inferior oblique muscle (m. obliquus inferior), come from the depths of the orbit, forming a common tendon ring (anulus tendineus communis) (Fig. 285) around ... ... Atlas of Human Anatomy
The eye is an organ for the perception of light stimulation in some invertebrate animals (in particular, cephalopods), all vertebrates and humans. In most invertebrates, the function of vision is performed by less complex organs of vision, for example... ... Great Soviet Encyclopedia
Basic organs - The main basic apparatus responsible for reception is the eyeball (bulbus oculi) (Fig. 283, 285). It has an irregular spherical shape and is located in the anterior part of the orbit. Most of the eyeball is hidden, and you can see... ... Atlas of Human Anatomy
Facial Action Coding System - Head and Neck Muscles The Facial Action Coding System (FACS) is a system for classifying ... Wikipedia
LICHTENBERG - Alexander (AlexanderLich tenberg, born in 1880), an outstanding modern German. urologist. He was an assistant to Cherny and Narath. In 1924, he received the management of the urological department at the Catholic Church of St. Hedwig in Berlin, to the swarm in... ... Big Medical Encyclopedia
Reflex - I Reflex (lat. reflexus turned back, reflected) is a reaction of the body that ensures the emergence, change or cessation of the functional activity of organs, tissues or the whole organism, carried out with the participation of the central nervous ... ... Medical encyclopedia
Eyelids - I Eyelids (palpebrae) are auxiliary organs of the eye, looking like semicircular flaps that close the front part of the eyeball when closed. Protect the open surface of the eye from adverse environmental influences and promote... ... Medical encyclopedia
Eye movement - Diagram of the extraocular muscles: 1. Common tendon ring 2. superior rectus 3. inferior rectus 4. medial rectus 5. lateral rectus 6. superior oblique 8. inferior oblique 9. levator palpebrae superioris 10 .… … Wikipedia
eyelids - (palpebrae) formations located in front of the eyeball. There are upper and lower eyelids that limit the palpebral fissure. Above the upper eyelid is the eyebrow. The eyelids are covered on the outside with skin, on the inside with the conjunctiva, and in their thickness there are dense... ... Dictionary of terms and concepts on human anatomy
source
muscle that lifts the upper eyelid - (m. levator palpebrae superioris, PNA, BNA, JNA) see List of anat. terms ... Big medical dictionary
CRYPTOPHTHALMUS - (from the Greek kryptos hidden and ophthalmos eyes), a congenital malformation in which the eyeball is covered with skin continuously stretched over it from the cheek to the forehead. Sometimes in place of the palpebral fissure there is a rudimentary hole, sometimes... ... Big Medical Encyclopedia
Accessory organs - The eyeball has mobility thanks to the muscles of the eyeball (mm. bulbi). All of them, except for the inferior oblique muscle (m. obliquus inferior), come from the depths of the orbit, forming a common tendon ring (anulus tendineus communis) (Fig. 285) around ... ... Atlas of Human Anatomy
The eye is an organ for the perception of light stimulation in some invertebrate animals (in particular, cephalopods), all vertebrates and humans. In most invertebrates, the function of vision is performed by less complex organs of vision, for example... ... Great Soviet Encyclopedia
Basic organs - The main basic apparatus responsible for reception is the eyeball (bulbus oculi) (Fig. 283, 285). It has an irregular spherical shape and is located in the anterior part of the orbit. Most of the eyeball is hidden, and you can see... ... Atlas of Human Anatomy
Facial Action Coding System - Head and Neck Muscles The Facial Action Coding System (FACS) is a system for classifying ... Wikipedia
LICHTENBERG - Alexander (AlexanderLich tenberg, born in 1880), an outstanding modern German. urologist. He was an assistant to Cherny and Narath. In 1924, he received the management of the urological department at the Catholic Church of St. Hedwig in Berlin, to the swarm in... ... Big Medical Encyclopedia
Reflex - I Reflex (lat. reflexus turned back, reflected) is a reaction of the body that ensures the emergence, change or cessation of the functional activity of organs, tissues or the whole organism, carried out with the participation of the central nervous ... ... Medical encyclopedia
Eyelids - I Eyelids (palpebrae) are auxiliary organs of the eye, looking like semicircular flaps that close the front part of the eyeball when closed. Protect the open surface of the eye from adverse environmental influences and promote... ... Medical encyclopedia
Source: https://ckiom.ru/myshtsy/myshtsa-podnimayuschaya-verhnee-veko-na-latinskom/
What are the causes of the disease
There are several factors that provoke the occurrence of tics, and the main one is nervous and emotional exhaustion.
It can occur from constant intense mental activity, frequent lack of sleep, moving and flying, lack of rest, regular stressful situations that arise at work or in the family. The reasons may be the following:
The above reasons are usually provoked by the person himself, causing twitching eyelid syndrome.
Sometimes there is also the presence of helminths, the presence of which a person does not even suspect. The onset of tic is caused by the presence of cervical osteochondrosis, when specific nerves associated with the muscle of the upper eyelid are pinched. Sometimes this is a harbinger of serious diseases: cerebral atherosclerosis, Parkinson's disease, meningitis, intracranial pressure.
Return to contents
What types of blepharitis affect the upper eyelid?
There is a certain classification of inflammation of the upper eyelid. These include:
- Catarrhal (simple) blepharitis, which is characterized by minor hyperemia - overflow of blood vessels. The swelling is slightly pronounced;
- Squamous blepharitis, the distinguishing feature of which is an accumulation of scales. Patients may complain that their eyelashes stick together, their eyes begin to hurt from bright light;
- Ulcerative blepharitis, in which crusts form along the edges of the eyes; when they are removed, bleeding ulcers are visible. The patient may develop madarosis - complete loss of eyelashes;
- Demodectic blepharitis, caused by the Demodex mite. It can be detected using microscopic examination. The microorganism lives on the edges of the eyelashes;
- Angular blepharitis, or rosacea, is characterized by reddish purulent “nodules” that form on the eyelids;
- Allergic blepharitis, its source is an allergen, accompanied by increased lacrimation and sensitivity to light.
Blepharitis of the upper eyelid is often accompanied by signs of conjunctivitis, keratitis, and meibomitis. A chalazion or stye may develop.
Hygiene procedures for blepharitis of the upper eyelid
Blepharitis is difficult to cure if hygiene procedures are not followed. Their implementation plays an important role in the treatment and prevention of this ophthalmological disease. The main hygienic procedure is daily eye washing. It is best to use sterile dressings and exclusively boiled water for this. Medicinal infusions of chamomile, marshmallow, rose hips, thyme or calendula, which have an anti-inflammatory effect, will have a good effect.
The prepared solution should be at room temperature. This will avoid damaging the damaged skin of the eyelids. It is necessary to rinse both eyes at once, even if only the eyelid is inflamed. Individual cotton swabs or bandages should be used for each. Reuse of hygiene products is prohibited. This can lead to infection of the visual organs and cause serious complications.
How to cure upper eyelid ptosis
It is necessary to fight ptosis only after finding out the cause. In the early stages of congenital pathology in the absence of visual impairment or a small cosmetic defect, it is recommended not to treat, but to carry out comprehensive prevention.
Treatment of ptosis is divided into conservative and surgical. Conservative methods go well with homemade folk recipes.
For ptosis due to injury or nerve dysfunction, it is recommended to wait about a year after the incident. During this time, effective treatment can restore all nerve connections without surgery or significantly reduce its volume.
What to do if your eyelid droops after Botox
Botox (botulinum toxin) is a drug derived from botulinum bacteria that disrupts the neuromuscular connection. The drug contains a neurotoxin, which in small dosages, when applied locally, attacks and kills nerve cells in the muscles, due to which they completely relax.
When using the drug in the cosmetic industry, a complication of incorrect or inaccurate administration can be ptosis of the upper eyelid after Botox injection, the treatment of which is very long. Moreover, the first few procedures can be successful, but each subsequent one requires an increase in the amount of the drug, which can lead to an overdose, as the body learns to develop immunity and antibodies to botulinum toxin.
The second method helps to speed up this process; for this, physiotherapeutic procedures (UHF, electrophoresis, massage, darsonval, microcurrents, galvanotherapy), injections of proserine, taking large doses of B vitamins, and neuroprotectors are actively used. All this accelerates the restoration of innervation and promotes rapid resorption of Botox residues.
Operation
Surgery to correct ptosis (drooping) of the upper eyelid is called blepharoplasty. The operation is indicated in cases of advanced ptosis with impaired quality of vision. The intervention is performed under local anesthesia on an outpatient basis. The rehabilitation period lasts about a month, during which the patient is observed by the operating surgeon.
There are many methods of operation, but the essence is the same - to shorten the relaxed muscle either by cutting and removing a part, or by folding it in half and stitching it. The cosmetic suture is hidden in a natural fold of skin, and over time it completely dissolves.
The cost of the operation depends on:
- complexity of the operation;
- stages of ptosis;
- additional research;
- the medical institution you have chosen;
- number of specialist consultations;
- number of laboratory diagnostics;
- type of anesthesia;
- accompanying pathologies.
Watch the video to see how the operation (blepharoplasty) goes: