Formation of germ layers
At the beginning of the week, at the tail end of the epiblast, cells multiply and line up, forming the Linea Primitiva. The head end ends in a thickening called the Hensen, or primordial node. From the line, the primary groove, sulcus primitivus, is formed, and from the node, the primary groove, fovea primitiva. The cells of the furrow and pit begin to purposefully descend under the epiblast and migrate. This process is called entry, retraction, capture or invagination. The time, location and direction of movement determine the further fate of the cells.
Literary sources interpret the formation of germ layers differently. Recent evidence confirms that the germinal endoderm and notochord are derived from cells captured through the anterior end of the primitive sulcus and the primitive pit. Some of these cells completely penetrate the hypoblast, pass between its cells and form the endoderm of the embryo.
Other cells migrate directly to the head end of the disc and form a spinal cord process, processus notochordalis, which, after complex rearrangements, turns into the spinal cord, or chord, notochorda. The notochord is the axis of the germinal disc. As the embryo grows, it disappears (remains are found only in the nuclei of the intervertebral discs and the nucleus pulposus).
Formation of germ layers and notochord
Cells captured through the primary groove migrate under the epiblast in a craniolateral direction. They form the embryonic mesoderm. Epiblast cells that have not passed through the primary pit and furrow give rise to the germinal ectoderm.
The body of the future embryo is formed anterior to the primordial sulcus, as a result of which the embryonic disc grows in a cranial direction, and the primordial sulcus shortens until it disappears (at the end of 4 weeks).
During this period, the embryo develops an oropharyngeal membrane and a cloaca (cloacalis). At these two sites, the ectoderm is in direct contact with the endoderm. Along the edges of the embryonic disc, the germ layers are connected to the corresponding non-embryonic leaves covering the walls of the amniotic and yolk sacs.
When and how is acrania detected?
The Ministry of Health of the Russian Federation insists on early registration of pregnant women for good reason. Many pregnancy pathologies are detected precisely at the initial stages of development - already at the first screening ultrasound. And only during this period can a pathological pregnancy be terminated using a safe medication method.
In connection with the above, women are recommended to contact an antenatal clinic at the first suspicion of the possibility of pregnancy. Significant disturbances in the baby’s neural tube appear just at the initial stages of its intrauterine development - pathology develops already in the 3rd week of pregnancy. The abnormalities are clearly visible on the first routine ultrasound, so there is no need to waste time confirming the diagnosis. If during a diagnostic ultrasound the specialist clearly distinguishes the brain tissue, but the main bone tissues have not yet formed, the diagnosis of acrania is inevitable. In this case, the woman is recommended to have an abortion before the 12th week of pregnancy. If the pathology is detected before 6 weeks, it will be possible to terminate the pregnancy with pills directly at the consultation.
Brain formation
Between the anterior end of the chord and the pharyngeal membrane of the mouth there is a prechordal layer, lamina prechordalis. Its cells emit molecular signals that promote the development (cephalization) of the future brain, which is why this area is called the organizational center of the head.
Thus, the two-leaf disc becomes the three-leaf embryonic disc, disc embryonicus trilaminaris, about 1.5 mm long, and the two-leaf, three-leaf blastocyst, blastocystis trilaminaris.
Formation of the nervous system
At the end of the third week, neurulation begins in the ectoderm (the neural plate is formed), and somitogenesis, somitogenesis and vasculogenesis begin in the mesoderm.
Neurulation is the formation of the neuroectoderm (neural tube and region) stimulated by the notochord. The notochord causes the cells of the ectoderm located above it to rise and thicken. This forms the neural plate in the ectoderm, lamina neuralis. It begins to bend, forming a neural groove, sulcus neuralis, with folds on the sides, plicae neurales. As the folds grow, the neural tube and tubular nerve cells form in the brain and spinal cord. There are openings at its ends: neuropores of the head and tail.
Formation of the nervous system
As the folds grow, the tube separates from the surface ectoderm. Some of the fold cells are separated and located on both sides between the tube and the surface of the ectoderm. This creates the neural layer, crista neuralis. Its cells quickly spread throughout the embryo and differentiate into cells of the peripheral nervous system, adrenal glands, peritoneal septum, pigment and other cells.
Spreading to the embryo in the head, the cells of the nerve spot turn into mesenchyme, mesenchyma capitis, from which various derivatives of the connective tissue of the head and neck (bones, ligaments, dura maters, dental dentin, cement, etc.) are later formed. Migration, proliferation, adhesion, etc. of these cells occurs. Disturbances in the process can lead to defects and syndromes in the development of various organs, usually called neurocristopathies. From the surface of the ectoderm, ectoderma superficialis, will later form the skin epithelium of the entire body and its derivatives.
How does damage to the nervous system occur in the fetus and infant?
Prepared by: Polina Rokhman
How does damage to the nervous system occur in the fetus and infant?
How does damage to the nervous system occur in the fetus and infant?
Damage to a child's brain, leading to cerebral palsy (CP), can occur even at the stage of intrauterine development of the fetus. Sometimes the cause of cerebral palsy is birth trauma. Also, cerebral palsy can occur after the birth of a child.
discuss in the cerebral palsy community
Cerebral palsy, cerebral palsy, cerebral palsy and other paralytic syndromes
What can affect the fetus during pregnancy?
As a rule, cerebral palsy is caused by brain damage that occurs during the fetal development stage. Damage to the child’s brain can be caused by chronic sexually transmitted infections, placental insufficiency, maternal illnesses during pregnancy (including viral infections, especially in the first trimester of pregnancy), exposure of the fetus to such unfavorable factors as radiation, chemical agents, and stressful situations. The number of household and office devices around us is constantly increasing, especially personal computers and mobile phones, on which some workers spend the whole day. Pregnant women are also increasingly exposed to electromagnetic radiation, which can cause disruption in the development of various organs and systems in the fetus, including the brain. One of the most significant mechanisms of intrauterine damage to the developing fetus is chronic oxygen starvation of its organs and tissues (especially the brain), which occurs as a consequence of the above reasons.
Conflict over blood groups and Rh factor
A significant cause of damage to the child’s nervous system is the conflict in blood groups and Rh factor between the mother and the unborn child. In these cases, the mother's body synthesizes antibodies (special proteins) that destroy red blood cells in the child's body. The breakdown products of these cells poison the body, causing the so-called protracted jaundice of newborns, and affect the baby’s nervous system. Usually, these complications can be avoided if the child’s mother registers with the antenatal clinic on time, regularly visits the doctor throughout pregnancy and carefully follows his instructions; and also if the pediatrician promptly pays attention to one of the manifestations of the breakdown of red blood cells (jaundice) and carries out timely and adequate treatment.
Birth injuries
Sometimes the cause of cerebral palsy is birth trauma. Birth trauma is defined as damage to the brain during childbirth, when the fetal head passes through the birth canal. Often, brain damage is caused by the entanglement of the umbilical cord around the neck of a newborn fetus, which causes disruption of the blood supply to the brain and its prolonged hypoxia, that is, lack of oxygen. As a result, certain parts of the baby’s brain die (this process is similar to a stroke in adults). It is worth noting that the brain of a newborn child is much more stable than the brain of an adult, and under influences that could lead to the death of an adult, the child is able to survive and develop, but with deviations from the norm, therefore, in the process of pathological childbirth, a child who is already in utero usually suffers was weakened by some adverse effect.
Infections and injuries in infancy
Cerebral palsy can also occur after the birth of a child if, in the first month of life, he suffers from severe infectious diseases complicated by meningitis or encephalitis, that is, an infectious process affecting the brain.
Source:
Methodological recommendations for parents about cerebral palsy, developed by the Scientific and Practical Center for Child Psychoneurology of the Moscow Department of Health.
The material used photographs belonging to medpro.ru
Formation of the body and internal organs
The mesoderm on both sides of the notochord is divided into axillary, paraxiale, intermediate and lateral plates. The mesoderm consists of segmented somitomeres and somites. The first somitomeres appear at the end of the 3rd week on both sides of the notochord head. Others develop alternately in a craniocaudal direction over two weeks (three pairs per day). In the neck and body of the embryo they become denser, forming a total of 42–44 pairs.
Scheme of somite development
In the embryo, the first seven somitomeres do not form compact somites; their cells proliferate and, together with the cells of the nervous sclera, form the mesenchyme of the head, which is the source of muscles and connective tissues of the head.
The interstitial mesoderm connects the somite to the lateral mesoderm. In the region of the neck and chest of the embryo, it is segmented and called somitial legs, or nephrotomes. The intermediate mesoderm in the lumbar region forms unsegmented metanephrogenic tissue.
The lateral mesoderm consists of two non-segmented layers - somatic (border) and intestinal. The border layer of mesoderm, together with the superficial ectoderm, will lead to the formation of the lateral and anterior wall of the body, and the leaf of the intestine, together with the endoderm, forms the respiratory and digestive system.
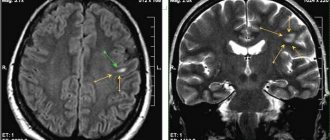
Embryogenesis of the brain
The brain is the most complex and advanced system of the human body. In its development, it, being the pinnacle of cellular organization, goes through several difficult stages (development).
It should be noted that during the periods when the main elements of the brain are formed, the fetus is most vulnerable. Knowledge about teratogenic periods makes it possible to protect the fetus from pathological influences, therefore, it is more likely to get healthy offspring.
We also note that for a better understanding of the macroprocesses of GM development, it is necessary to understand the microprocesses.
Actually, embryogenesis
So, at the stage of gastrulation, as a result of complex morphogenetic changes, 3 germ layers are formed, one of which is the ectoderm - the source of the primordia of the NS organs. Next, a neural plate is formed from the dorsal ectoderm, which is located along the midline of the back of the embryo.
Then the neural folds and n. are formed from the latter. groove. Of which, in turn, is the neural tube. At the early stages of embryogenesis, the neural tube is a multirow neuroepithelium; later, 4 concentric zones differentiate in it.
The cells of the first, ventricular zone, are the precursors of neurons and macroglia. The cells of the subventricular zone are devoid of nuclei and have great proliferative potential. The intermediate/mantle/mantle zone is the source of the gray matter of the spinal cord and brain. And finally, the fourth, marginal or marginal zone of the neural tube precedes the cerebral cortex, as well as the cerebellum.
Then the precursors of the cavities and sections of the brain begin to form - the brain vesicles. In the fourth week of intrauterine development, the stage of three brain vesicles begins.
At this stage, the GM consists of three structures: the forebrain (lat. Prosencephalon), the midbrain (lat. Mesencephalon), the hindbrain or rhombencephalon (lat. Rhombencephalon)
After 2 weeks, the stage of five brain vesicles begins, during which the forebrain is divided into the final (lat. Telencephalon) and intermediate (lat. Diencephalon) brain. And the rhomboid is divided into the hindbrain (lat. Metencephalon) and the medulla oblongata (lat. Myelencephalon, hereinafter – Medulla oblongata).
Subsequently, the following are differentiated from the telencephalon: the lateral ventricles of the brain, the hemisphere of the brain, the corpus callosum, the fornix, the septum pellucidum, and the anterior commissure of the brain.
From the diencephalon are formed: the third ventricle, thalamus, pineal gland, geniculate body, hypothalamus.
From the midbrain develops: the aqueduct of Sylvius, the cerebral peduncle, the quadrigeminal plate.
The fourth ventricle, pons, and cerebellum arise from the hindbrain.
Conclusion
The brain is a complex structure, so to speak. A structure consisting of several elements, the development of each of which is individual - and at the same time, inextricably linked with the other elements.
The loss or underdevelopment of any part is almost always fatal both for the fetus and for the already formed organism, because pathological changes in the brain lead to a chain of degenerative somatic changes in the entire body. All this once again proves and emphasizes the importance of this structure of the body.
Education of the cardiovascular system
In front of the pharyngeal membrane of the mouth, where the lateral mesoderm of both sides of the body connects, a field is formed for the formation of the heart.
Here, at the end of the 3rd week, the heart, primordium cardiacum, begins to develop, which on days 21-22 already begins to pulsate at a speed of 65 rpm. The cardiac conduction system begins to form. From the angioblasts, which originate from the lateral mesoderm, the first blood vessels are formed, which connect with the non-embryonic bloodstream that appeared a few days earlier in the yolk sac. Thus, the cardiovascular system of the embryo is the first organ system that begins to function.
From the lateral leaves and somites of the mesoderm, cells are formed that fill the gaps between the rudiments of organs - they form mesenchyme. Between the leaves is a cavity called the intraembryonic cell, the coelom, which later becomes the cavities of the pericardium, thorax and peritoneum.
Mesenchyme
Violations of embryo formation at 3 weeks of pregnancy
- Tumor of the chord, chordoma
. Remnants of the chord can lead to the formation of benign or malignant slow-growing tumors - chordomas. They usually form at the base of the skull or in the sacrum and coccyx. - Neural tube defects
. They include not only the lack of growth of the neural tube, but also disturbances in the distribution of surrounding tissues and structures (meninges, spinal arteries, muscles, skin). One of them is a fissure (cleft) of the spinal cord, myeloshisis. This is a neurulation defect in which the folds of the neural groove do not connect, do not grow, and all or part of the neural tube remains open. A rupture of the spinal cord is always accompanied by an open rupture of the spine, spina bifida aperta. - Cutaneous sinus
. When the neuroectoderm is not completely separated from the superficial ectoderm during neurulation, a depression or duct remains at the site, connecting the skin to deeper tissues (subcutaneous tissue, spinal cord, or brain). Most often, the pathology is found in the sacrum and tail bone (called the sacrococcal cavity) along with a closed divided spine, spina bifida oculta. - Caudal dysplasia, sirenomelia.
During germinal leaf formation, cell proliferation and migration may be impaired for certain genetic or teratogenic reasons, and deficient mesoderm may remain at the caudal end of the germinal disc. This can lead not only to hypoplasia and fusion of the legs (mermaid tail), but also to other defects in the distribution of mesoderm derivatives of the lumbosacral region (urinary and genital organs, spine, anus). It is believed that this defect may also be caused by poor circulation in the caudal part of the fetal body. - Reverse position of organs, situs inversus visceralis.
This is the location of all or some of the internal organs, such as the heart, on the back side of the body. This defect is caused by the movement of oscillating monocilia in the cells of the primary ganglion.
According to the “nodal flow” theory, the primary node secretes morphogens that are pushed onto the left side of the embryonic disc by monocilia. Consequently, there is an asymmetric distribution of morphogens, which determines the corresponding location of the internal organs. Some patients with inverted organs have Kartagener syndrome, which is caused by primary ciliary dyskinesia due to a mutation in the dynein protein gene.
MAKE AN APPOINTMENT
Abortion and contraception clinic in St. Petersburg - department of the medical gynecological association "Diana"
Make an appointment, tests or ultrasound via the contact form or by calling +8 (812) 62-962-77. We work seven days a week from 09:00 to 21:00.
We are located in the Krasnogvardeisky district, next to the Novocherkasskaya, Ploshchad Alexander Nevsky and Ladozhskaya metro stations.
The cost of a medical abortion in our clinic is 3,300 rubles. The price includes all pills, an examination by a gynecologist and an ultrasound to determine the timing of pregnancy.
Share link:
What is a neural tube?
The formation of the nervous system in the fetus directly depends on the development of the tube. It is formed from a neural plate, which gradually closes into a tube, forming a small process - the rudiment of the future nervous system. If you examine the neural tube in section, you will notice several layers: internal, marginal and intermediate. The intermediate and marginal layers provide the production of gray and white matter of the spinal cord, which is then located in the spine. Several processes occur in the inner layer at once: cell division and synthesis of future material responsible for the baby’s genetics.
It takes the first weeks of pregnancy for the baby's neural tube to develop.
Development of the nervous system at 4-5 weeks of pregnancy
So, we found out at what period the fetal nervous system is formed. But what happens to her next?
The neural tube has some extensions called medullary vesicles. When the fetal nervous system is established, three brain vesicles appear. One of them turns into the forebrain (it includes two hemispheres), the other into the visual center of the head, and the third into the rhombencephalon, which includes several more sections.
The marginal part of the neural tube also produces a new organ, the neural crest, which is responsible for the development of several systems. At 4-5 weeks, only a black dot is visible on ultrasound. So far, this is all that has managed to grow. However, this is already a lot for a child, because at that moment the cells responsible for his brain were born. At this point, folic acid is needed for good neuronal development. Under no circumstances should you treat your teeth in the first trimester! Any medications, even local anesthesia, can reverse the normal course of cell division in the nervous system. Because of this, the baby may be born with disabilities.
Development of the fetal nervous system at 6-12 weeks of pregnancy
When the nervous system of the fetus is formed, the mother should be at rest. The first weeks of pregnancy are important because the health of the child depends on them. Already at 7-8 weeks the baby is capable of reflexes. For example, it was noticed that when his lips came into contact with the processes, he tilted his head back, thereby protecting himself from danger. This is how a protective reflex develops. At 10 weeks, the baby is able to open his mouth if something irritates his lips. At the same time, the grasping reflex occurs when something bothers the baby’s hand.
By the twelfth week, the baby can move his toes. From this, doctors concluded that those parts of the brain that are responsible for the lower part of the fetal body begin to function first. Until the child reaches three months of uterine age, he will not be able to fully respond to irritations. His movements will be sharp and short. This happens because excitation is still affecting small areas of the nervous system. But the fetus grows and develops, and over time its systems become more advanced.
Fetal development at 14-20 weeks of pregnancy
The norms of development of the fetal nervous system can only be determined using ultrasound. If you are told that the fetus meets all developmental standards, you don’t have to worry. But what is your child doing at this time? By the fourteenth week the baby becomes quite active. If before he could not move yet, then by the fifteenth week one can already count about 15 new movements the baby has mastered.
When the nervous system of the fetus is formed, the mother feels the first tremors of the baby. They appear at 19-20 weeks. An ultrasound can already distinguish movements of the arms and legs, as well as hiccups, swallowing, yawning and other mouth movements. Between 15 and 20 weeks, the number of synapses, the places in the nervous system to which signals are transmitted, increases. Due to this, the scope of the baby’s activities expands.
Condition of the fetus at 20-40 weeks of pregnancy
After the 20th week, when the nervous system is still developing, the fetal medulla begins to branch. This means that the exposed nerve cells will be covered with a layer of fat and will be able to function fully. The baby's nervous impulses will accelerate, and he will soon be able to add new movements to his range of skills. The fetal limbs are the first to develop. The sense of smell improves a little later (about 24 weeks). In parallel with these changes, the brain also develops, in which a framework for nerve cells is built.
It is noteworthy that the mass of the brain accounts for up to 15% of the total mass of the fetus. After the main processes in the brain have ended, it is time for another one - the destruction of certain types of cells. According to scientists, there is nothing terrible in this process. This is simply how the body cleanses itself of unnecessary structures that have already done their job. So, when the nervous system of the fetus is formed, the body spends all its energy on its proper development.