Main reasons
Headaches are primary, i.e. not associated with the course of any disease, and secondary, when headache is one of the symptoms of the underlying disease. The most common primary headaches during pregnancy include migraine
, tension headache, and
cluster headache
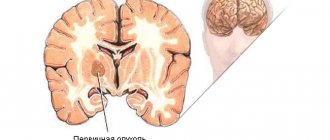
. Primary headaches are not life-threatening. Less common are secondary headaches, which can be a symptom of a life-threatening condition - stroke, aneurysm, cerebral venous thrombosis, subarachnoid hemorrhage, pituitary tumor, choreocarcinoma, eclampsia, preeclampsia, idiopathic intracranial hypertension, reversible cerebral vasoconstriction, so they must be excluded first.
Is it important how exactly a woman describes the pain (sharp, dull, etc.)? Of course, it is very important - a detailed history of the disease is necessary to make an accurate diagnosis, and in this case it is important to know the intensity, frequency, nature, time of headache attacks, accompanying symptoms, etc.
Among the primary headaches during pregnancy, the most common are migraine and
tension headache
, and in some cases, very rarely, cluster headache.
Why does my head hurt?
During pregnancy, all organs and systems go into increased work mode. At the same time, the expectant mother often experiences worries about her unborn child. Against this background, headaches develop. There are several reasons for their occurrence:
- increased blood pressure -
may be associated with an existing chronic disease or with fluid retention in later stages; - severe weight gain -
during pregnancy, weight gain should occur gradually, observing certain standards, in order to prevent too much stress on the blood vessels, including the brain; - low blood pressure -
occurs due to chronic diseases or redistribution of blood from the upper parts of the body to the lower parts: to the uterus; - lack of nutrients -
the need for vitamins and minerals in pregnant women increases several times, so they are advised to take them additionally; - stress -
pregnant women often experience anxiety about their condition or anxiety about their unborn child; - chronic pathologies -
ARVI, osteochondrosis, damage to the kidneys and eyes can lead to increased pressure, temperature or pinching of nerve endings, which provokes pain; - weather change -
pregnant women often become weather-sensitive and have a hard time experiencing changes in air temperature or pressure.
A doctor can determine the cause of headaches. To do this, a pregnant woman needs to come to her gynecologist and get a referral from him for an examination or consultation with a specialist.
Migraine
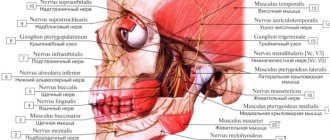
With migraine, the headache is usually pulsating in nature and unilateral, predominantly frontotemporal, with irradiation of pain to the eyes on the side of the pain, although there are cases of bilateral localization.
The intensity of the headache is very pronounced. Such a headache takes a woman away from her daily activities, forces her to lie down with her head in the pillow and not move, since any movement intensifies the headache. Another characteristic symptom of migraine is increased sensitivity to sound and light, combined with sweating, palpitations and nausea, and sometimes vomiting. Sometimes a migraine attack can be preceded by dizziness, the sensation of strange smells and even visual disturbances (zigzags, sparkling dots, sparks from the eyes). However, approximately seven out of ten women note that headaches during pregnancy either regress completely or bother them significantly less, and are easier in the second and third trimester, which is associated with changes in the level of estrogen in the hormonal system of a pregnant woman. However, one in ten women report worsening headache symptoms during pregnancy. After childbirth, in most women, migraines return to their previous course. In addition, migraines have certain provocateurs: imbalance of estrogen levels, bright light, sound, lack of sleep, oversleeping, stress, hunger, red wine, etc.
Treatment methods
Treatment of headaches in early pregnancy is carried out under the supervision of a doctor. At home, you can only take medications that are approved by your doctor after an examination. In the early stages, paracetamol and its analogues (Solpadeine), as well as drotaverine in various tablets (No-Shpa), are allowed. Minor headaches can be eliminated with simple techniques that do not require the use of medications:
- proper rest - must necessarily include long walks in the fresh air, physical activity;
- complete cessation of bad habits;
- proper nutrition with a sufficient amount of vitamins and microelements; it is also recommended to take special vitamin complexes for pregnant women;
- neck and head massage (can be performed independently) is one of the ways to quickly relieve spasms without pills and eliminate headache symptoms;
- for prevention - regular measurement of blood pressure, blood tests, examination by a doctor according to schedule.
The Clinical Brain Institute specializes in identifying the causes and treatment of headaches. During pregnancy, these symptoms cause concern for the expectant mother, so it is important to seek medical help promptly. Our center has modern equipment, thanks to which diagnostics have become as accurate as possible. Treatment is selected individually, taking into account the effectiveness of the prescribed regimen.
Clinical Brain Institute Rating: 5/5 — 3 votes
Share article on social networks
Tension headache
With a tension headache, the pain is usually bilateral, constant, of moderate intensity, that is, it does not distract the woman from everyday activities and even becomes easier with physical activity.
The nature of a tension headache is pulling, aching, squeezing the entire head like a “hoop”, with a feeling of pressure on the eyes, and can sometimes be accompanied by mild nausea or fear of sound. It is most often provoked by stress, less often by pain in the cervical spine. With a cluster or cluster headache, the pain is paroxysmal in nature, it is burning, pulsating in nature, and affects one half of the head and face (forehead, temple, orbit). It is so unbearable that it is impossible to sit or stand, and it bothers me more often at night with short but frequent attacks. During an attack, the eye may become red and watery (mainly on the side of pain), the nose may become stuffy, and the forehead may become covered with perspiration.
As you know, pregnancy makes certain changes in the female body, which can increase the risk of some dangerous complications and cause the development of secondary headaches. Cardiovascular complications are especially dangerous, such as stroke, cerebral venous thrombosis, subarachnoid hemorrhage, pituitary tumor, choreocarcinoma, eclampsia, preeclampsia, idiopathic intracranial hypertension, reversible cerebral vasoconstriction, which require timely diagnosis and immediate treatment.
Possible causes of headaches during pregnancy
Headaches occur in more than a third of women during pregnancy; most patients have not previously complained of such symptoms. If discomfort occurs against the background of fatigue and toxicosis, it will pass simultaneously with other clinical signs. Of particular danger are cases in which headaches occur simultaneously with nausea and vomiting, surges in blood pressure, decreased visual acuity, and even fainting. All these factors should be a reason to consult a doctor, as they can affect the normal development of the fetus.
The causes of headaches in pregnant women may vary. Doctors at the Clinical Brain Institute will be able to preliminarily determine them during the initial examination. To do this, you will need information about the conditions under which pain occurs, its duration, nature and location, as well as the conditions for its disappearance. The most common cause is migraine. This term refers to acute, throbbing pain that occurs suddenly and spreads to half or the entire surface of the head. It is accompanied by nausea, dizziness, disorders of the gastrointestinal tract and visual apparatus. Predisposing factors to its occurrence may be:
- sudden changes in temperature and humidity, weather changes;
- nervous tension, stressful situations;
- chronic fatigue, lack of normal sleep and wakefulness;
- prolonged exposure to trigger factors, including bright lights or loud sounds.
Another type is tension headache (TTH) . This is a condition that is characterized by local painful sensations that begin in the occipital or frontal lobes and then spread to the entire surface of the head. They can be of varying intensity, but do not cause nausea - this is their main difference from migraines. They are often caused by emotional tension and stress, as well as excessive physical or mental stress. The pain in most cases occurs after waking up and gradually intensifies during the day. Its duration ranges from 30 minutes to several days, but it is easily relieved with painkillers.
Cluster headaches (CHH) are a separate type. They appear when you feel well, for no apparent reason, and can last from 15-20 minutes to an hour. They are sharp, pulsating, localized at a certain point and do not spread to the entire surface of the head. Their characteristic feature is periodicity. Such pain can occur several times a day or a week, but at regular intervals.
Headaches during pregnancy are also associated with the following conditions:
- hormonal disorders and natural changes;
- diseases associated with surges in blood pressure;
- toxicosis of pregnant women and associated dehydration;
- unhealthy diet with a predominance of fatty or sweet foods, as well as an insufficiently nutritious diet;
- increased air pollution, prolonged stay in a stuffy room.
Headaches can also be symptoms of old chronic diseases that worsen during pregnancy. Hypo- or hypertension, changes in intracranial pressure, vascular pathologies - all these problems can manifest themselves as the body experiences significant stress. It is also worth understanding that old cranial herbs, which have long ceased to bother the patient, can cause headaches during pregnancy.
In the first trimester
Headaches in the first trimester of pregnancy are common. Significant changes occur in a woman’s body, to which she has yet to adapt. Among the reasons that can cause headaches in early pregnancy are:
- an increase in the total volume of blood in the vessels - it creates additional pressure and causes stretching of the vascular walls;
- increased concentrations of hormones (estrogens, progesterone), which can cause fluctuations in vascular tone;
- correction of lifestyle and nutrition, giving up certain foods and bad habits - these changes also require a period of adaptation;
- early toxicosis is a reaction of immune mechanisms to the fetus.
Early toxicosis is considered to occur before 12-13 weeks. During this period, pregnancy often proceeds without clinical manifestations, but some women complain of headache, nausea and general weakness. This reaction is caused by the immune system's response to the formation of the fetus. Normally, some mechanisms are blocked that perceive it as a foreign protein, but this process can also be accompanied by headaches and discomfort.
In the second trimester
The second trimester of pregnancy is a less dangerous period. Some women still complain of toxicosis and other side effects, but, in general, the adaptation mechanisms are already sufficiently formed. If headaches begin to occur during this period, you should pay attention to your well-being - a symptom may signal dangerous disorders. These include:
- glaucoma is a group of diseases in which there is an increase in intraocular pressure;
- sinusitis - inflammatory processes in the paranasal sinuses;
- inflammation of the brain and its membranes;
- osteochondrosis of the cervical spine is a disease that is manifested by a decrease in metabolic processes in hyaline cartilage and its gradual destruction, which leads to compression of nerves and blood vessels;
- diseases of the kidneys and urinary system are the cause of the accumulation of excess fluid in the body.
Not every headache should be a cause for concern. If discomfort continues for 5 days or more, accompanied by decreased visual acuity or stiffness of the neck muscles, you should immediately consult a doctor. In other cases, the symptom may be the result of overwork or physical stress, or lack of daily routine.
In the last trimester
In the last trimester of pregnancy, headaches can develop for several reasons, including physiological ones. An increase in body weight leads to increased curvature of the spinal column. This condition increases the risk of compression of the blood vessels that carry oxygenated blood to the brain. The result of this condition is tissue hypoxia, which is manifested by a deterioration in general health and headache. In addition, a decrease in physical activity also causes poor blood circulation. Even in the third trimester, it is worth paying attention to light physical activity.
In some cases, headaches are caused by nervous tension and stress associated with the upcoming birth. The emotional state of the mother must remain stable, otherwise it may affect the proper development of the fetus. However, such cases of headache are considered the least dangerous - they are not associated with serious internal disorders and are treated with conservative methods.
Late toxicosis (preeclampsia) is a complication of pregnancy. Nausea, swelling, and headaches in the third trimester cannot be considered normal. In addition, this condition can threaten both the health of the mother and the development of the fetus in the final stages. A diagnosis can be made if three characteristic symptoms are present:
- the appearance of edema;
- hypertension;
- the presence of protein in the urine.
Preeclampsia may be associated with insufficiency of the urinary system and kidney disease. Nephropathy can be diagnosed by a significant increase in blood pressure - this symptom may be absent in hydrops of pregnancy.
One of the most dangerous manifestations of late toxicosis is eclampsia. This is a rare form that is manifested by convulsive muscle contractions and loss of consciousness in response to any irritant. It can be a flash of light or a loud sound. Preeclampsia is a less dangerous condition, but it can also harm the health of mother and baby. It occurs without convulsive syndrome, and its main symptoms are acute headache, dizziness, and a feeling of heaviness in the forehead and occipital region. In addition, during an attack, visual impairment is observed: a veil appears before the eyes, different spots, and in some cases, temporary blindness. Additionally, there are complaints of nausea and vomiting, pain in the right hypochondrium. In such cases, pregnancy should proceed in a hospital setting so that doctors can relieve convulsions and intoxication in a timely manner without harm to the health of the mother and fetus.
What should you especially be wary of?
You should be alerted to changes in the course of your usual headache or a headache
, which you have not experienced before and which is unlike anything else. In addition, it is important to know the dangerous symptoms that should alert you and your doctor, the so-called “red flag symptoms.”
These include:
- acute, severe headache;
- first-time headache with the development of persistent focal neurological symptoms;
- severe and continuously worsening headache with visual disturbances lasting more than 60 minutes, with severe vomiting;
- headache that worsens when lying down (this also includes headaches triggered by coughing, sneezing, or physical stress);
- headache in people over 50 years of age, and also accompanied by fever or epileptic seizures.
Diagnosis of headache includes consultation with a neurologist.
It is imperative to consult an ophthalmologist. An MRI of the brain is necessary to exclude or detect brain tumors. In some cases, magnetic resonance arteriography and magnetic resonance venography are needed. The first will determine the presence or absence of aneurysmal dilatation of the arteries, and the second will determine vascular thrombosis. Ultrasound of the vessels of the neck and head will help identify the presence of atherosclerotic plaques and changes in the vertebral arteries. Sometimes headaches are caused by pathologies of the cervical spine, which can be detected by MRI of the cervical spine. The use of radiography during pregnancy is not advisable. In addition, a detailed collection of the patient’s life history and the presence of chronic diseases (hypothyroidism, the presence of autoimmune diseases, arterial hypertension, depression) and recording of medications taken (hormones, anticonvulsants, caffeine-containing and psychotropic drugs) is necessary.
Do I need to endure a headache?
There is no need to endure a headache. Immediate treatment of headaches is necessary, since long-term headaches lead to the development of anxiety and depression, sleep disturbances and decreased appetite, which can negatively affect the body of the mother and fetus. At the same time, it must be remembered that pregnancy and lactation quite seriously limit the possible range of medications due to the high risk of negative effects of these medications on the fetus during the period of intrauterine development of the fetus and after birth through mother’s milk.