The renal unit is called the nephron. It is responsible for filtering blood and forming primary urine. The functional unit of the kidney removes toxins and metabolic products from the body. Nephrons work around the clock, filtering up to 1.7 thousand liters of blood plasma. In this case, a little more than a liter of excreted urine is formed. In this case, about 170 liters of primary urine are formed per day. Subsequently, this volume is condensed to the daily urine norm. There are about 2 million nephrons in our kidneys. If we calculate the total surface area of the nephrons performing the excretory function, it will be approximately 8 m². This is three times the area of skin.
Nephron structure
The nephron is the structural and functional unit of the kidney, which has an impressive margin of safety.
The nephron is the structural and functional unit of the kidney, which has an impressive margin of safety. Such a reserve is possible only due to the fact that only 1/3 of the nephrons are functioning at the same time. Therefore, a person can continue to live even after one of the kidneys is removed.
The kidney unit purifies arterial blood, which enters the organ through the afferent artery. The purified blood is removed through the efferent artery. Since the afferent artery is larger in cross-section than the efferent artery, a pressure difference is formed in the kidneys.
We figured out what the structural unit of the kidneys is called. It remains to understand the structure of the nephron. It consists of the following departments:
- The nephron begins in the renal cortex from Bowman's capsule. It is located above the capillary node of the arteriole.
- Bowman's capsule communicates with the nearest tubule. This tubule penetrates the medulla. This is the answer to the question - name in which part of the organ the capsules of the renal nephrons are localized.
- This tubule then transforms into the loop of Henle. It consists of two segments - proximal and distal, the first of which is considered the initial one.
- The end of the renal nephron is where the collecting duct forms. It receives secondary urine from functioning nephrons.
If you only list the constituent parts of the nephron but do not understand how they function, your understanding of the functional unit of the kidney will be incomplete. Thus, taking into account the composition of the nephron, it is possible to describe in detail the functions of each section of this functional unit.
Capsule
Podocyte cells are collected around the capillary glomerulus. They surround the ball like a cap. This formation is commonly called the renal corpuscle. Physiological fluid penetrates the pores of the renal corpuscle and ends up in Bowman's capsule. In this place, an infiltrate is formed, that is, a product of blood plasma filtration.
Proximal tubule
The proximal tubule is the part of the nephron that is covered on the outside by the basement membrane.
The proximal tubule is the part of the nephron that is covered on the outside by the basement membrane. In this case, microvilli are located on the inner side of the epithelial layer. They, like a brush, line the inner surface of the tubule along its entire length.
The basement membrane on the outside of the tubule forms multiple folds. When this part of the organ is filled, the folds are smoothed out. At this moment, the tubule itself becomes rounded in cross section, and its epithelium thickens significantly. If there is no fluid in the tubule, then its diameter narrows and the cells have a prismatic shape.
Among the main functions of the tubules are the reabsorption of the following substances:
Is disability given after kidney removal and what are the conditions?
- water;
- magnesium, potassium, calcium and chlorine ions;
- sodium – 85%;
- salts of sulfates, phosphates and bicarbonates;
- compounds of vitamins, proteins, glucose and creatinine.
Further from the tubules, substances and compounds penetrate into the blood vessels that densely intertwine it. In this area, the functional unit of the kidney absorbs into the lumen of the tubule:
- bile acids;
- uric, oxalic and para-aminohippuric acid;
- adrenalin;
- histamine;
- thiamine;
- acetylcholine.
Important: medicinal compounds are transported through the cavity of the renal tubule, namely furosemide, penicillin, atropine, etc. Also in this place, hormones (gastrin, insulin, prolactin, etc.) are broken down, as a result of which their concentration in the blood plasma decreases.
Loop of Henle
In terms of its internal structure, the loop at the initial stage does not differ much from the structure of the proximal tubule.
The structural and functional unit of the kidney is the nephron. In the next section, it consists of the initial section of the loop of Henle. The renal tubule is transformed into a descending portion of the loop that descends into the medulla. And the ascending segment of this loop rises into the cortex, approaching Bowman’s capsule.
In terms of its internal structure, the loop at the initial stage does not differ much from the structure of the proximal tubule. Gradually the lumen of this loop narrows. In this lumen, Na is filtered, entering the interstitial fluid, which is now considered hypertonic. This is important for the functioning of the collecting ducts - due to the high salt content in the washing physiological fluid, water is absorbed into the ducts. Then the ascending portion of the loop begins to expand, which transforms into a distal tubule.
Distal tubule
The distal tubules are shorter sections consisting of low epithelial cells. The inner surface of the canal is no longer lined with villi. On the outside, the folded basement membrane is still present. In this part, the nephron, as a structural unit of the kidney, functions on the principle of reabsorption of water, sodium, and also releases ammonia and hydrogen ions into the lumen.
Histology.RU
Material taken from the site www.hystology.ru
Kidney development. During the period of embryonic development, three excretory organs are sequentially formed: the prebud, the primary kidney (Wolffian body) and the final kidney.
The anterior kidney is formed from the segmental legs of 8-10 cranial segments of the mesoderm, which, while maintaining a connection with the coelomic cavity, but separating from the somites, are sequentially connected to each other and form the mesonephric (Wolffian) duct (Fig. 295-7).
The primary kidney is formed by the segmental legs of subsequent trunk segments. Their dorsal ends also empty into the mesonephric duct. A characteristic feature of the primary kidney is the close functional connection of its tubules with the arterial capillary network. By growing over a glomerulus of capillaries, the wall of the urinary tubule forms a two-layer capsule that receives blood plasma filtration products into its cavity. The glomerulus of capillaries and the capsule together form the renal corpuscle. The primary kidney functions as an excretory organ during the embryonic period of animal development (II).
The final bud is formed later and begins to function in the second half of embryonic development (III): It is formed from the nephrogenic segmented portion of the mesoderm of the caudal part of the body of the embryo. During the development of the final kidney, a system of tubules grows into it from the Wolffian duct, forming the ureter, renal pelvis, renal calyces, papillary ducts and collecting ducts. Unsegmented nephrogenic tissue accordingly forms the system of urinary tubules of the final kidney, including the epithelium of the capsule of the renal corpuscles (Fig. 296).
Rice. 295. Scheme of development of excretory organs:
I - preference; II - primary kidney (Wolffian body); III - final bud; 1 - duct of the primary kidney (Wolffian duct); 2nd canaliculus of the kidney; 3 - glomerulus of capillaries; 4 - aorta; 5 - afferent arteries; 6 - renal corpuscle; 7 - tubule of the primary kidney; 8 - renal corpuscle and tubule of the final kidney; 9 - renal artery; 10, 11 - developing tubules; 12 - ureter.
Kidney structure . The surface of the kidney is covered with a connective tissue capsule. The parenchyma of the organ consists of a peripheral cortex and an inner medulla. The anatomical structure and shape of the kidneys are different in different animal species. Most mammals have lobed kidneys. They can consist of a number of independent lobes (whale) or represent a single complex formed by many merging lobes to varying degrees (cow, horse, sheep, etc.). The shares are, to one degree or another, isolated from one another. In the parenchyma of the lobes, the cortex and medulla are distinguished.
The characteristic structures of the cortex are the renal corpuscles, consisting of a glomerulus of capillaries and a glomerular capsule, and convoluted tubules. The medulla contains straight tubules. The border between the cortex and medulla is uneven. The cortex, descending between the medullary pyramids, forms the renal columns (columns). Straight tubules extending into the cortex form the medullary rays.
Nephron is a structural and functional unit of the kidney parenchyma. The number of nephrons in the kidneys is estimated at 1-2 million. Along their length, nephrons are represented by various segments that differ from each other in structure, position in the organ and participation in the formation of urine. The length of the nephron is from 18-20 to 50 mm. (For example, the total length of all nephrons in the human kidney is about 100 km.)
The blind proximal end of each nephron is expanded and immersed in its own cavity, resulting in the formation of a spherical, two-layer capsule covering the glomerulus of the capillary. The capillaries with the surrounding capsule make up the renal corpuscle. It has two poles: 1) the vascular pole, where the arteriole enters the renal corpuscle, bringing blood into the capillary network of the glomerulus, and the arteriole exits, carrying it out; and 2) the urinary pole, which turns into a convoluted proximal one
Rice. 296. Development of the final bud:
1 - branching of the growing collecting duct; 2 - nephrogenic tissue; 3 - urinary tubule formed from nephrogenic tissue; 4 - urinary tubule before joining the collecting duct; 5 - urinary tubules connected to the collecting duct; 6 - urinary tubule in a later stage of development; 7 - forming capsule of the renal corpuscle; 8 - artery forming the vascular glomerulus; 9- capsule of the renal corpuscle; 10 - afferent arteries of the glomerulus; 11 - collecting duct; 12 - connective tissue.
Rice. 297. Scheme of the structure of the renal corpuscle and juxtaglomerular complex:
1 - proximal nephron; 2 - cells of the outer leaf of the capsule; 3 - podocytes; 4 - endothelial cells; 5 - blood capillary; 6 - red blood cells; 7 - afferent arteriole; 8 - efferent arteriole; 9 - smooth muscle cells; 10 - endothelium; 11 - juxtaglomerular cells; 12 - distal nephron; 13-dense spot.
nephron tubule (Fig. 297). The latter wriggles in the renal cortex near its renal corpuscle. It becomes a straight proximal tubule, which plunges into the renal medulla, where it becomes a thin tubule of the nephron loop.
The thin section—80% of the nephrons (cortical nephrons)—is short and lies entirely within the cortex. 20% of nephrons are nephrons located near the medulla (juxtamedullary nephrons). They have a long, thin tubule that descends into the medulla. The thin tubule is followed by a distal straight tubule; it ascends into the cortex to its renal corpuscle, passes into the region of its vascular pole and passes into the convoluted distal tubule, connected by an arcuate collecting duct to a straight collecting duct. The collecting ducts are located in the medullary rays of the cortex and in the medulla. Based on the origin of the collecting ducts from the outgrowth of the mesonephric duct, they are classified as urinary tracts, although functionally they are connected to the nephron. Several collecting ducts open into
Rice. 298. Scheme of the structure of the nephron:
1 - glomerular capsule; 2 - convoluted part of the proximal section; 3 - straight part of the proximal section; 4 - thin section; 5 - straight part of the distal section; 6- curled part of the distal section; 7 - collecting tube.
Rice. 299. Scheme of the submicroscopic structure of the internal layer of the capsule and capillaries of the vascular glomerulus:
1 - podocytes; 2 - cytotrabeculae; 3 - cytopodia of podocytes; 4 — endothelial cell cytoplasm; 5 - basement membrane; 6 - endothelial cell pores; 7 - endothelial cell nucleus; 8 - mesangial cell; 9 - lumen of the capillary.
papillary Canadian. From the papillary tubules, urine enters the renal cups, pelvis and ureter (Fig. 298).
Fine structure and histophiaiology of the kidney. In the renal corpuscle, primary urine is formed due to the filtration of blood plasma components from the lumen of the glomerular capillaries into the cavity of the glomerular capsule.
The endothelium of the capillaries is very thin. Its flat cells have a large number of pores with a diameter of 70-90 nm, in most cases without burrow diaphragms. The nuclear part of the cells is thickened and often contacts the mesangial cells of the glomerulus. The latter are stellate in shape and apparently correspond to the pericytes of the capillaries of other organs.
The inner (visceral) layer of the glomerular capsule is formed by one layer of cells - podocytes, located on the basement membrane lying between them and the endothelium of the capillaries {Fig. 299, 300, 301).
Podocytes are flat cells, with several primary processes extending from their basal surface - cytotrabeculae, giving off numerous secondary processes - cytopodia. The total length of podocyte processes is 1-2 µm. The cytopodia of cells interdigitate (intertwine) with the processes of neighboring cells, as a result of which a complex system of intercellular gaps is formed, ensuring the process of filtration of primary urine. Podocyte nuclei are irregularly shaped. In their cytoplasm, the Golgi complex, granular endoplasmic reticulum, and a large number of free ribosomes, filaments and microtubules are well developed.
The only continuous layer between the blood circulating in the capillary network of the glomerulus and the cavity of the capsule collecting primary urine is the basement membrane. Its thickness is up to 0.15 microns, it consists of a network of fibrils and a glycoprotein matrix. Three layers can be distinguished in the membrane - the outer and inner are light, and the middle one, containing microfibrils, is darker. The basement membrane is a barrier that controls the process of filtration of blood plasma into the cavity of the renal corpuscle, retaining large protein molecules, as a result of which only a small amount of albumin enters the capsule cavity.
The outer (parietal) layer of the glomerular capsule is formed; one layer of flat cells located on the basement membrane. It directly passes into the epithelium of the proximal tubule.
Fig 300 Scanning electron micrograph of a glomerulus
1 - capillaries; 2 - podocytes (according to Bloom Faucet).
Rice. 301.Blood capillary of the glomerulus (electronic
1- endothelium; 2 - basement membrane; 3 - cytopodia; 4 - erythrocyte.
Rice. 302. Renal corpuscle. Proximal and distal convoluted tubules:
1 - renal corpuscle; 2 - outer leaf of the capsule; 3 — capsule lumen; 4 - glomerulus of capillaries; 5 - proximal convoluted tubule; 6 - distal convoluted tubule.
The proximal tubule is divided into convoluted and straight parts. The convoluted part - the proximal convoluted tubule, forming loops in the cortex in the region of the renal corpuscle, goes to the periphery of the organ, returns and passes into the straight part - the proximal straight tubule. It is this that is directed to the medulla and represents the thick part of the descending part of the loop. The diameter of the proximal tubule is about 60 µm. Its cavity varies from a narrow slit to a wide rounded lumen. The epithelium of the proximal tubule consists of a single layer of cubic cells. Their apical surface contains numerous microvilli, which together form a brush border on the surface of the cells. The latter is characterized by high alkaline phosphatase activity, which
Rice. 303. Electron microscopic structure of the proximal tubule of Vephron:
a - microvilli; b - mitochondria; c — Golgi complex; d - inclusion of secretion; d - basement membrane; e - core; g — folds of the basal plasmalemma.
indicates its participation in the processes of reabsorption of glucose from primary urine (Fig. 302, 303). At the base of the microvilli of the brush border, the cell membrane, plunging into the cytoplasm, forms the thinnest tubules. In the cytoplasm of the apical pole of the cells, vacuoles are formed, which are characterized by a positive reaction to acid phosphatase, which allows them to be interpreted as secondary lysosomes, structures involved in the digestion of protein molecules absorbed from primary urine.
Mitochondria are concentrated in the basal part of the cells of the proximal tubule of the nephron. They are located in chains delimited by deep folds of the plasmalemma of the basal pole of the cells.
Rice. 304. Kidney medulla:
1 - thin tubule; 2 - straight part of the distal section; 3 - collecting tube; 4 - blood capillary.
The regular arrangement of mitochondria and plasma membrane folds, which determines the basal striation characteristic of proximal tubule cells under light microscopy, indicates the activity of substance transport during the formation of definitive urine. In the proximal section, 85% of water and electrolytes, glucose, amino acids, and vitamins are reabsorbed.
Thin descending limb of the nephron loop. The proximal straight tubule, sharply narrowing (to 13-15 µm) passes into a thin tubule. The cuboidal epithelium of the proximal tubule is replaced by flat epithelium (0.5-2 µm in height). Areas of cells containing nuclei protrude into the lumen of the tubule. There are single microvilli on the apical surface of the cells. The cytoplasm of cells is poor in organelles. They contain single mitochondria, individual free ribosomes, and a centrosome located near the nucleus. The cell membrane in its basal part forms single folds (Fig. 304).
The thin tubules of the nephrons, the glomeruli of which are localized in the peripheral zone of the organ’s cortex, are short. They are limited only to the descending segment of the urinary tubule loop. In the longer nephron loops, originating from the renal corpuscles located in the deep zone of the cortex, the thin tubules are longer. They pass into the deep zone of the medulla, there they form a loop, return again to its peripheral zone, and only here they pass into the next thick section of the ascending part of the loop (see Fig. 298). The junction is considered the boundary of the outer and inner zones of the medulla. The inner zone contains only thin tubules and collecting ducts. In the thin section of the loop (the dense tubule of the nephron), the absorption of water from the lumen of the tubule into the blood capillaries intertwining the latter continues.
The distal tubule is shorter and somewhat thinner than the proximal one (20-50 µm). It consists of a straight part (distal straight tubule) and a convoluted part (distal convoluted tubule)* The straight part makes up the thick ascending segment of the loop. The distal straight tubule has a diameter of 35 µm. The brush border and apical tubule are absent, but in the basal part of the epithelial cells, chains of mitochondria located between the folds of the basal plasma membrane form a basal striation (Fig. 305). The Golgi complex is poorly developed. It is located
Rice. 305. Basal pole of the distal tubule cell:
1 - mitochondria; 2 — folds of the basal plasmalemma; 3- basement membrane (arrows - capillary pores).
above the core. The cells contain a few granular cisterns: the endoplasmic reticulum and free ribosomes. In the distal rectum, reabsorption of electrolytes continues, but its wall is poorly permeable to water. Water cannot passively follow the electrolytes and remains in the lumen of the tubule. Therefore, urine in the lumen becomes hypoosmotic, and osmotic pressure increases in the surrounding connective tissue.
At the point where the distal straight tubule is adjacent to the vascular pole of the glomerulus, the side of the tubule in contact with the afferent and efferent arterioles forms a disc of tall, narrow cells. The cell nuclei in the disc lie close to each other, so the disc is called the macula dense, which is part of the juxtaglomerular complex (see below).
The distal convoluted tubule has a length of 4.6-5.2 mm and a diameter of 20-50 µm. Its structure does not differ from the structure of the straight distal tubule.
Sodium pumping continues in the distal convoluted section, but here Na+* ions are partially replaced by other cations (K+- and H+) and acidification of the urine occurs.
The collecting ducts are lined with cubic or low prismatic epithelium. Most of their cells are light-colored and poor in organelles. Hypotonic urine enters the collecting ducts, and there is high osmotic pressure in the environment due to the accumulation of electrolytes actively pumped out of the lumen of the distal straight tubules. As a result of the difference in osmotic pressure, water leaves the collecting ducts into the peritubular space and enters the blood of the vasa recta. Thus, the collecting ducts not only drain urine from the kidney parenchyma into the urinary tract system, but also participate in its formation.
The initial sections of the collecting ducts, localized in the medullary rays of the kidney parenchyma, are lined with single-layer cuboidal epithelium. It has light, structureless cytoplasm and clearly defined cell boundaries. As the collecting ducts merge in the deep zone of the medulla, the epithelium becomes higher, so in the papillary ducts it is already represented by a typical prismatic epithelium.
The juxtaglomerular complex is a complex of structures in the region of the vascular pole of the renal glomerulus, producing the hormone renin, which participates in the chain of reactions of the formation of the vasoconstrictor angiotensin in the blood plasma, regulating blood pressure and the reabsorption of sodium and water in the renal tubules.
The complex includes: 1) the dense spot of the dietary tubule, 2) epithelioid, or juxtaglomerular, cells of the wall of the afferent arteriole, 3) cell islands of Gurmagtig, located between the afferent and efferent arterioles of the renal corpuscle. Morphologically, the latter are characterized by small oblong nuclei.
In the area of contact between the afferent arteriole of the renal corpuscle and the distal tubule of the nephron, there is no internal elastic membrane in the arterial wall. Under the endothelium of this segment of the afferent arteriole lie epithelioid cells, their cytoplasm is weakly basophilic, contains a granular cytoplasmic reticulum and coarse granularity, giving a positive PAS reaction that is not stained with hematoxylin-eosin - juxtaglomerular cells. They are closely adjacent to the base of the cells of the macula densa of the urinary tubule, which in this area does not have a basement membrane. The Golgi complex of cells is shifted to their basal pole.
Gurmagtig cells lie between the afferent and efferent arterioles and the macula densa (see Fig. 297). They have long* shoots. The stroma of the renal medulla contains process cells in contact with the tubules of the nephron loops and blood capillaries. It is assumed that these cells participate in the processes of reabsorption of electrolytes into the blood.
Renal vascularization. The renal artery, entering the portal of the kidney, forms interlobar arteries passing between the pyramids of the organ. At the border of the cortical and medulla parenchyma of the organ, they pass into the arcuate arteries, from which interlobular, or radial, arteries extend into the parenchyma of the cortical substance, leading to the surface of the organ. The latter give off numerous afferent arterioles that enter the renal corpuscles and form capillary glomeruli in them. The efferent arterioles of the glomeruli of the cortical nephrons secondarily disintegrate into the cortical peritubular capillary network, which drains blood through the venous system into the vessels of the kidney. The latter originates under the capsule of the organ from the stellate veins, which form interlobular veins, running parallel to the interlobular arteries and flowing into the arcuate veins. The arcuate veins merge to form interlobar veins that flow into the renal vein.
The efferent arterioles of the juxtamedullary nephrons partly break up into the medullary peritubular capillary network, and partly into the straight vessels of the vascular bundle. These are thin-walled vessels of larger diameter than capillaries. They form loops in the medulla. The arterial and venous parts of the loop are in close contact, which ensures rapid exchange of electrolytes in this countercurrent system. The vascular bundle plays an important role in the final concentration of urine, carrying away water coming from the collecting ducts and thus maintaining the concentration difference between the contents of the collecting ducts and the surrounding hypertonic environment.
Innervation of the kidney . The nerve trunks entering the kidney through the code of blood vessels contain myelinated and non-myelinated fibers. Myelin fibers originate predominantly from the posterior thoracic and anterior lumbar ganglia and end with receptor endings localized in various parts of the kidney parenchyma. Unmyelinated nerve fibers of a sympathetic and parasympathetic nature were identified in all parts of the nephron, including in the area of the juxtaglomerular complex. In the area of the renal pelvis and in the parenchyma of the organ, individual ganglion cells have been described.
Reviews (0)
Add a review
Types of nephrons
There are several types of nephrons, differing in their functional purpose and structural features.
You now know that the structural and functional unit of the kidney is the nephron. But it turns out that there are several types of nephrons, differing in functional purpose and structural features:
- Juxtamedullary.
- Cortical, namely intracortical and superficial.
Cortical
There are two types of nephrons located in the renal cortex. Of these, superofficials account for only 1%. Their differences are a low filtration volume, a shortened loop of Henle, and superficial localization of the glomeruli in the cortex.
The share of intracortical nephrons accounts for 80%. They are localized in the middle part of the cortex. These nephrons perform the main functions of filtering urine. At the same time, the blood in such nephrons flows under high pressure. This is due to the expansion of the adductor artery.
Juxtamedullary
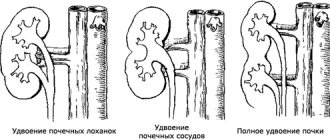
This is a small group of nephrons, accounting for only 20%. Most of the nephron is located in the medulla, and the capsule is located at the border of the medulla and the cortex. In such nephrons, the loop of Henle descends almost to the renal pelvis.
What is kidney dystopia: symptoms and diagnosis
These nephrons are important for the concentrating function of the kidneys, that is, the organ's ability to concentrate urine. This type of nephron has the longest loop of Henle, and the efferent and afferent arteries have the same diameter.
Functions of renal nephrons
The main task of these renal nephrons is the formation of urine and the reabsorption of important and useful substances and compounds
. Since the nephron is the functional unit of an organ, the main tasks of this organ are as follows:
- regulation of vascular tone;
- concentration of urine;
- blood pressure control.
The process of urine formation consists of several stages:
- The glomeruli filter the blood plasma that enters the organ through the arteries. As a result, primary urine is formed.
- Beneficial substances are reabsorbed from the resulting filtrate.
- Urine concentration occurs.
Functions of cortical nephrons
The main task of these renal nephrons is the formation of urine and the reabsorption of important and useful substances and compounds - amino acids, proteins, glucose, minerals, hormones. These nephrons are involved in the process of urine filtration and reabsorption, since they have some features of the blood supply. All reabsorbed beneficial substances and compounds immediately enter the blood through the capillary network of the efferent artery, which is located nearby.
Functions of juxtamedullary nephrons
The main task of these kidney elements is to concentrate urine. This is achieved due to certain features of blood transportation through the efferent artery. The artery does not pass through the capillary node, but immediately flows into venules, which transform into veins.
Important: this type of nephron is involved in the formation of substances that regulate blood pressure. The complex of these nephrons produces renin, which is needed for the formation of a special vasoconstrictor substance - angiotensin 2.
Functional disorders in the activity of nephrons
If malfunctions occur in the functioning of the nephrons, this affects the activity of all organs and systems. Among the disorders that arise due to nephron dysfunction, the following disorders can be mentioned:
- water and salt balance;
- acidity;
- metabolism.
All diseases that develop against the background of impaired transport activity of nephrons are usually called tubulopathies. Among them the following varieties are distinguished:
- Primary tubulopathy occurs against the background of congenital nephron dysfunction.
- Secondary forms of the disease arise due to acquired disorders of the transporting activity of the organ.
Common causes of secondary tubulopathy are damage to the nephron due to toxic damage to the body, malignant neoplasms or heavy metal poisoning. According to the location, all tubulopathies are divided into distal and proximal, depending on which tubules are affected (distal or proximal).
The number of nephrons is limited
For normal life, approximately a third of the nephrons present in the kidneys are sufficient. The rest are reserve, in case of death of those functioning (as a result of injury or illness). The structural and functional unit of the kidney cannot recover, therefore, as a result of any damage, their number in the kidneys decreases. Over time, if such processes progress, renal failure may develop, negatively affecting the functioning of all organs and systems.
With the invention of means that help restore the filtering structures of the kidney, a lot of problems arising as a result of diseases affecting this organ will be solved. In the meantime, experts say, the only measure to prolong the functional viability of the kidneys is the prevention of diseases of the urinary system and timely comprehensive treatment of acute diseases, which does not allow them to become chronic.