In some patients, a routine urine test can reveal the presence of specific salt particles - oxalates, which is an alarming sign indicating a malfunction of the urinary system.
Oxalaturia, or the excretion of oxalates in the urine, is a variant of urinary syndrome characterized by the appearance of oxalic acid salts, in particular calcium oxalates, in the urine.
In clinical practice, this syndrome can be found in almost every third patient, and more than half of them do not have any clinical symptoms of the disease. It is important to distinguish between normal and pathological.
The excretion of oxalate salts in the urine, not exceeding 40 mg/day (for adults), is normal. Such patients are subject to annual medical examination.
The excretion of oxalates in the urine in quantities exceeding the norm is called hyperoxaluria. The norm is adjusted for creatinine excreted in the urine, so the daily urinary excretion of oxalates should not exceed 30 mg per gram of creatinine excreted.
Today it is known that the most dangerous for the urinary system are complex organo-mineral salts of calcium and oxalic acid, such as wewellite (calcium oxalate monohydrate) and weddellite (calcium oxalate dihydrate).
It is these compounds that are the most common components of stones in the urinary system; they have the ability to disrupt the functioning of the renal nephron and lead to microtraumas of the urinary tract.
Oxalates as the main factor in stone formation
The study of the chemical composition of kidney stones is an integral part of the examination of patients suffering from urolithiasis, which makes it possible to judge the type of metabolic disorders and the cause of urolithiasis.
Currently, there are 4 most significant groups of urinary stones (phosphate, urate, oxalate, cystine), of which oxalic acid salts account for more than 65%.
Until about the 50s of the 19th century, the excretion of calcium oxalates in the urine was considered a normal physiological phenomenon that did not affect the state of the urinary system and did not lead to its pathology.
The connection between hyperoxaluria and the formation of kidney stones was reliably established only in 1952 and is currently considered as the main trigger of urolithiasis.
It is the increased secretion of oxalates and calcium that is today a generally accepted risk factor for the formation of stones in the urinary system (according to the European urological recommendations for the treatment and prevention of urolithiasis from 2013).
Chemical structure
Oxalates are salts of oxalic acid, which, in turn, belongs to dicarboxylic acids and has the ability to crystallize in aqueous solutions in the form of transparent crystals (dihydrates).
With metals of the alkaline group, oxalic acid forms soluble compounds, while compounds with metals of other groups are completely insoluble or slightly soluble.
As for calcium ions, with them oxalic acid forms a salt that is practically insoluble in a neutral and alkaline environment and is of great biological importance.
The solubility of calcium oxalates increases slightly in the presence of urea, magnesium ions, lactate, sulfate, and with an increase in the concentration of hydrogen ions in the urine (physiological fluctuations in urine pH are small and have a minor effect on the solubility of oxalates).
As a ligand
Oxalate, the conjugate base of oxalic acid, is an excellent ligand for metal ions. It usually binds as a bidentate ligand, forming a 5-membered MO.2C2 ring. An illustrative complex is potassium ferrioxalate, K3[Fe (C2O4)3]. The drug oxaliplatin exhibits improved aqueous solubility compared to older platinum-based drugs, avoiding the dose-limiting side effects of nephrotoxicity. Oxalic acid and oxalates can be oxidized by permanganate in an autocatalytic reaction. One of the main uses of oxalic acid is to remove rust, which occurs because the oxalate forms water-soluble derivatives with the ferric ion.
Oxalate metabolism in the body
The continuous exchange of oxalic acid is carried out due to internal (endogenous) and external (exogenous) sources.
Among exogenous sources, we can highlight ascorbic acid and food products rich in oxalates; among endogenous sources, we can highlight the breakdown of glycine and serine in the body, the final product of which is oxalic acid.
Oxalic acid is found in large quantities in foods such as coffee, tea, chocolate, spinach, parsley, potatoes, grapes, beets, purslane, and is also the end product of the oxidation of ascorbic acid.
With food intake, the average person receives from 100 to 1200 mg of oxalates per day, of which approximately 100-300 mg from drinks (coffee, tea).
Oxalic acid supplied with food makes up approximately 10% of its total amount in the human body, while the rest is formed as a result of the oxidation of ascorbic acid and glycine.
In a healthy person, oxalates contained in foods bind to calcium in the intestinal lumen and are excreted from the body in the feces in the form of insoluble salts.
The final absorption of oxalic acid from food is insignificant and amounts to approximately 2-6% of the total amount. The main part of oxalates excreted in the urine are the end products of the destruction of ascorbic acid, glycine, and hydroxyproline.
Excess oxalic acid produced in the human body is excreted primarily by the kidneys, and saturation of urine with these compounds leads to the precipitation of salts in the form of crystals.
It is known that urine is a solution of salts that are in dynamic equilibrium due to specific substances (inhibitors) that stimulate the dissolution of its constituent parts.
Weakening the activity of urinary inhibitors accelerates the formation of salt crystals, including oxalates.
Crystallization and precipitation of oxalates are also influenced by other substances in the urine. Thus, magnesium prevents crystallization, and its deficiency is a risk factor for urolithiasis.
Structure
X-ray crystallography of simple oxalate salts shows that the oxalate anion can adopt a planar conformation with D2 molecular symmetry, or a conformation in which the O–C–C–O dihedrals approach 90° with approximate D2d symmetry.[20] In particular, the oxalate moiety adopts a planar, D2h conformation in solid-state structures of M2C2O4 (M = Li, Na, K).[21][22] However, in the structure of Cs2C2O4, the dihedral angle O – C – C – O is 81 (1) °.[23][24] Consequently, Cs2C2O4 is more closely approximated by D2d symmetry structure because the two CO2 planes are staggered. Two forms of Rb2C2O4 were structurally characterized by single crystal X-ray diffraction; one contains flat oxalate and the other contains checkerboard oxalate.
Because previous examples show that the conformation adopted by the oxalate dianion depends on the size of the alkali metal to which it is bonded, some have examined the barrier to rotation around the central CC bond. The barrier to rotation around this bond was determined by calculation to be approximately 2–6 kcal/mol for the free dianion, C2O2− 4.[25][26][27] Such results are consistent with the interpretation that the central carbon-carbon bond is best viewed as a single bond with minimal pi interactions between two CO− 2 units.[20] This barrier to rotation around the CC bond (which formally corresponds to the difference in energy between the planar and staggered shapes) can be attributed to electrostatic interactions since the unfavorable OO repulsion is maximized in the planar shape.
It is important to note that oxalate often occurs as a bipronged, chelating ligand, such as in potassium ferrioxalate. When oxalate chelates with a single metal center, it always adopts a planar conformation.
The benefits and harms of oxalic acid salts
Oxalic acid is one of the components of homeostasis in the human body and is part of a large number of biological membranes, tissues and liquids. It is responsible for the stability of cell membranes, and its deficiency can adversely affect human health.
Among the negative properties of oxalic acid, one can note its ability to be deposited in the form of calcium salts in various organs, such as the kidneys, gall bladder, skin, and thyroid gland.
The most common disease associated with excess oxalate is urolithiasis.
The prevalence of this disease in Russia is approximately 34-40%, covering all age groups, including newborns.
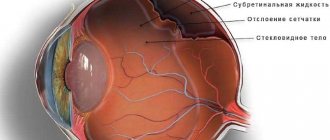
Oxalates can be removed from the body only by urine excretion by the kidneys and nothing else. An excess of these salts inevitably leads to the development first of microcrystalluria, and then to the formation of oxalate stones.
Due to the low solubility of oxalates in water, the renal epithelium is often damaged, which can lead to nephropathy and CKD (metabolic nephropathy).
Relation to oxalic acid
The dissociation of protons from oxalic acid occurs in steps, as for other polyprotic acids. The loss of one proton results in the monovalent hydrogen oxalate anion HC 2O− 4. A salt with this anion is sometimes called acid oxalate
,
monobasic oxalate
, or
hydrogen oxalate
.
The equilibrium constant ( K
a ) for the loss of the first proton is 5.37 × 10−2 (p
K
a = 1.27).
The loss of the second proton, which produces an oxalate ion, has an equilibrium constant of 5.25×10−5 (n K
a = 4.28). These values mean that in neutral solutions, there is no oxalic acid and only trace amounts of hydrogen oxalate exist.[19] In the literature, the distinction between H2C2O4, HC 2O− 4, and C 2O2− 4 is often unclear, and the collection of species is called oxalic acid.
Classification of hyperoxaluria
As described above, oxalates excreted in the urine are either intermediate metabolic products or enter the body along with the food consumed.
Based on this, several main types of oxalauria (hyperoxaluria) can be distinguished, depending on the mechanism of increasing the level of excreted oxalates:
- 1Primary – rare hereditary pathologies with an autosomal recessive type of inheritance of the mutation gene. The mutation consists in the absence of enzymes that metabolize glyoxylic acid, which leads to a sharp increase in the biological synthesis and excretion of oxalates. Ultimately, this mutation leads to progressive urolithiasis and decreased GFR.
- 2Secondary spontaneous hyperoxalaturia. This group of diseases is characterized by a moderate increase in the internal biological synthesis of oxalates, as well as a decrease in the stabilizing properties of urine against the background of a monotonous diet, viral infections and incurrent diseases, for example, connective tissue dysplasia.
- 3Secondary alimentary hyperoxaluria is associated with excess intake of oxalic and ascorbic acid into the body from food. This group also includes transient hyperoxalaturia due to hypovitaminosis A, B1, B6, which are inhibitors of oxalate formation.
- 4Intestinal oxalaturia is caused by increased absorption of oxalic acid in the intestine. They can be observed in chronic inflammatory diseases of the digestive system and food allergies.
- 5 Oxaluria developing in patients with existing independent pathology of the urinary system (pyelonephritis, hydronephrosis, glomerulonephritis, etc.). This group of oxalaturias is caused by the presence of a membranopathological process in the kidneys caused by the underlying disease. Pathology of renal membranes can be triggered by constant oxidative stress, changes in local antioxidant defense, and activation of the phospholipase system. When unstable phospholipid membranes are destroyed, oxalate precursors are formed.
- 6Oxaluria caused by congenital (membrane instability) or secondary pathological process in membranes that arose under the influence of unfavorable environmental factors. Here, the leading role is given to the processes of lipid peroxidation.
Dysmetabolic nephropathy (oxaluria) in children: a modern approach to treatment
Dysmetabolic nephropathies (DN) are a large group of kidney diseases with different etiologies and pathogenesis, which are based on metabolic disorders.
In a narrower sense, some authors understand the term DN as a polygenically inherited (multifactorially developing) nephropathy, which is associated with the pathology of oxalic acid metabolism and manifests itself in conditions of familial instability of cytomembranes [1]. As a result of a disturbance in the metabolism of oxalic acid, the so-called oxaluria and/or calcium oxalate crystalluria develops. In foreign literature, the term DN does not exist; the pathology in question is diagnosed as oxaluria or hyperoxaluria.
Oxaluria is usually divided into primary and secondary. Primary DN (oxaluria) are hereditary diseases that are characterized by a progressive course, early development of urolithiasis and chronic renal failure. This group of diseases is caused by the absence of glyoxylic acid metabolic enzymes, which leads to a significant increase in the synthesis of oxalates in the body. Secondary DN (oxaluria) are polygenically inherited or multifactorial diseases, the implementation of which requires external adverse influences.
The leading pathogenetic link in the occurrence of these nephropathies is the structural and functional destabilization of cell membranes, activation of lipid peroxidation (LPO), and inhibition of the body's antioxidant defense. That is, this nephropathy is a variant of renal membranopathy and manifests itself in conditions of instability of cell membranes [2].
Among the pathogenetic pathways for the development of oxaluria and/or calcium oxalate crystalluria, the following are also distinguished:
- increased intake of certain substances into the body;
- pathology of various organ systems (mainly the digestive tract), leading to disruption of the metabolism of oxalic acid;
- unfavorable environmental factors, drug therapy.
In some cases, DN (oxaluria) is divided into several groups depending on the conditions against which these diseases occur [3]:
- The first group includes DN with calcium oxalate crystalluria (DOCC), which are characterized as polygenically inherited nephropathies associated with oxalic acid pathology and manifesting themselves in conditions of instability of renal cytomembranes.
- The second group is oxaluria or DNOKK in children with diseases of the urinary system (pyelonephritis, glomerulonephritis, etc.), caused by a secondary membranopathological process in the kidneys caused by the underlying kidney disease.
- The third group is nephropathy, which develops under the influence of unfavorable environmental factors.
This approach to understanding the problem can serve as one of the prerequisites for developing an algorithm for the treatment of DN (oxaluria).
A number of foreign researchers believe that one of the main places in the development of DN (oxaluria) belongs to the pathology of the digestive tract. Thus, dysbiotic intestinal disorders (in particular, deficiency of lactobacilli) can lead to impaired degradation of oxalates in the digestive tract, which is accompanied by increased absorption of oxalates in the intestines and the development of oxaluria. This mechanism in the pathogenesis of hyperoxaluria is reflected in a new approach to the treatment of these conditions - the use of probiotics [4]. It is of interest to study the role of the anaerobic microorganism Oxalobacter formigenes. This microorganism produces the enzyme oxalyl-CoA decarboxylase, which leads to the degradation of oxalates, which affects the regulation of oxalate homeostasis, preventing its absorption in the intestine. Results of studies performed by Troxel SA et al. in 2003 in the USA, indicate a connection between the presence of O. formigenes in the intestine and the development of hyperoxaluria. Adults and children over 16 years of age were observed in this study. The main group consisted of patients suffering from urolithiasis with hyperoxaluria, the control group included people without urolithiasis. The study showed that O. formigenes was not detected in 60% of those examined in the main group and only in 26% of the control group [5].
Children with oxaluria, as a rule, do not have specific clinical symptoms of the disease. Quite common may be complaints of abdominal pain, dysuric phenomena (up to attacks of renal colic), and in more severe cases - signs of damage to the musculoskeletal system. DN (oxaluria) can be combined with allergic diseases of the skin and respiratory tract. In the anamnesis of children suffering from oxaluria and/or DNOCC, various diseases associated with metabolic disorders (urolithiasis, cholelithiasis, diabetes mellitus, etc.) are quite common.
The main diagnostic method for these conditions is laboratory diagnostics. Laboratory changes characteristic of DN (oxaluria) are:
- increased oxalate content in biochemical urine analysis;
- the presence of oxalate crystalluria in single urine tests;
- microerythrocyturia from 2 to 20–30 in the field of view;
- microproteinuria from trace to 0.066%;
- absence of pronounced tubular dysfunctions;
- markers of cytomembrane instability (urinary excretion of ethanolamine, lipids, peroxides, increased activity of phospholipids, etc.) and a decrease in the anti-crystal-forming ability of urine [6].
To diagnose DN (oxaluria), a combination of clinical symptoms and the above laboratory changes can be used. In this regard, it should be noted that the term DN (oxaluria) and “crystalluria” are not synonymous. Crystalluria is a variant of urinary syndrome and is most often transient in nature. Often it disappears after an illness (ARVI, ARI).
Treatment
The basic principles of treatment of DN (oxaluria and/or DNOC) are:
- diet therapy - aimed at limiting the intake from food and the formation of “salts” in the body;
- maintaining the stability of cytomembranes and suppressing the processes of lipid peroxidation (LPO) - membrane stabilizing and antioxidant agents;
- increased fluid intake to reduce the concentration of crystalloids in the urine.
The recommended diet is aimed at reducing the functional load on the kidneys. During an exacerbation of oxalate nephropathy, a potato-cabbage diet is recommended. This diet should be recommended for 2-3 weeks. In the future, when the process stabilizes, the therapeutic diet can be expanded. However, it excludes foods containing large amounts of oxalates (
).
The diet also limits the consumption of foods that are sources of ascorbic acid (black currants, Antonov apples, radishes, rose hips, etc.).
Until now, foods that are a source of calcium are excluded or limited from the diet of children suffering from DN (oxaluria and/or DNOC). At the same time, there are studies whose results have not revealed a positive effect of limiting foods that are sources of calcium on the course of oxaluria/hyperoxaluria [8, 9]. It should be noted that these studies were performed in adults, whose calcium requirements are more stable.
Borghi L. and his colleagues in 2002 observed two groups of patients suffering from urolithiasis. The first group received a low-calcium diet, while the patients in the second group used a low-protein, low-salt diet with normal calcium levels. The study showed that the recurrence rate of urolithiasis was much higher in patients in the group receiving a low-calcium diet, especially towards the end of the observation period [8].
Similar results were obtained by Nouvenne A., Meschi T., Guerra A. et al. In this study, of two groups of patients examined with idiopathic oxalate urolithiasis, the level of oxaluria significantly decreased in the group of patients receiving a low-protein, low-salt diet with normal calcium levels. In the group of patients receiving a diet with reduced calcium levels, no reliable results were obtained regarding a decrease in the level of oxaluria (
) [9].
Thus, at the present stage, the issue of limiting foods that are sources of calcium in the diet of children suffering from oxaluria is not assessed unambiguously. Taking into account the results of the above studies, it can be assumed that calcium intake should correspond to the physiological norm of the child’s need for this mineral.
In recent years, studies have appeared on the effectiveness of using probiotics in patients suffering from oxaluria. There are indications in the literature about the effectiveness of using lactic acid bacteria in the treatment of people suffering from oxaluria. In particular, a number of foreign studies have shown that the use of lactic acid bacteria (Lactobacillus casei and Bifidobacterium breve) in complex treatment with diet therapy helps reduce the level of oxaluria, which, according to the authors, is the basis for recommending the use of probiotics in conjunction with diet [4].
An important part of the treatment of oxaluria is the administration of membrane stabilizers and antioxidants. For this purpose, vitamins A and E, a complex of vitamins B1 and B6 are used in the treatment of DN (oxaluria). Vitamin A (1000 IU per year of life per day) is used in combination with vitamin E (1–1.5 mg/kg/day, but not more than 15 mg/day) in courses of 3 weeks quarterly. Vitamin B6 is used at a dose of 1–3 mg/kg/day in the first half of the day, taking into account the biorhythm of its absorption for 1 month. The combined use of vitamin B6 and vitamin B2 is highly effective. The dose of vitamin B2 is 2.5–5 mg/day [10].
Traditionally, the drug Xidifon (2% solution) is still used, which regulates calcium metabolism at the cellular level, prevents its deposition in soft tissues, and also inhibits excessive activity of phospholipases. It is used in a dose of 10–20 mg/kg body weight in 2 doses per day. Duration of treatment ranges from three weeks to 6 months. This drug should be prescribed in combination with vitamins A and E.
The domestic drug Dimephosphone (15% solution), which is prescribed at the rate of 1 ml for every 5 kg of weight (or 30 mg/kg) in three doses, has a membrane-stabilizing effect. This drug has shown its effectiveness in patients with atopy. Thus, the use of this drug seems appropriate in children with oxaluria combined with atopic dermatitis and bronchial asthma.
For DN (oxaluria), it is advisable to prescribe medications containing magnesium. Magnesium preparations can be used: Magne B6, Magnerot, Natural Kalm.
In recent years, the effectiveness of the use of enterosorbents has been proven, especially in environmentally unfavorable regions [3] and, in particular, the enterosorbent Enterosgel [11].
In addition to diet therapy, the use of membrane stabilizers and antioxidants in the treatment of oxaluria, an adequate drinking regime is of sufficient importance. In these conditions, it is recommended to increase fluid intake by 50% of the required amount for a given age, provided that the function of the cardiovascular system and kidneys is satisfactory. Additional fluid intake is recommended in the evening and before bedtime. Preference is given to mineral waters, which are prescribed at the rate of 3 ml per kg of body weight, taken 3 times a day (15–20 minutes before meals). Duration of use is 2–3 weeks. Among mineral waters, “Slavyanovskaya”, “Smirnovskaya”, “Bzhni”, “Naftusya” can be used.
Thus, timely and adequate treatment of DN (oxaluria) is an important factor in the prevention of diseases such as urolithiasis. At the same time, at the present stage, a number of methodological approaches in the treatment of these conditions are the subject of discussion and require further research.
For questions regarding literature, please contact the editor.
E. A. Gordeeva , Candidate of Medical Sciences
RMAPO , Moscow
Table 1.
Table 2.
Causes of primary hyperoxaluria
Oxalosis, or primary oxaluria (primary hyperoxaluria) is a disease from the group of hereditary disorders of glyoxylic acid metabolism.
The pathology is characterized by recurrent oxalate urolithiasis (formation of oxalate kidney stones), a decrease in GFR and the gradual development of renal failure. There are three types of hereditary mutations that lead to oxalosis.
- The first type of oscasia occurs in approximately 80% of cases and is caused by a mutation in the alanine-glyoxylate aminotransferase gene, which leads to increased synthesis of oxalates from glyoxylate. The incidence of primary hyperoxalaturia in European countries is approximately 1 person per 120 thousand newborns.
- Type 2 oxalosis is much less common and is caused by a mutation in the glyoxylate reductase-hydroxylate-pyruvate kinase gene, which ultimately also leads to increased synthesis of oxalates and L-glycerate.
- The third type of mutation is in the DHD PSL gene, which encodes a protein similar in structure to mitochondrial enzymes. Metabolic disorders that occur with this type of oxalaturia have not yet been fully studied.
Bowel diseases and oxalates in urine
Increased absorption of oxalates in the intestine is observed not only with all types of inflammatory processes in the intestinal wall, but also with all types of fat malabsorption (cystic fibrosis, chronic pancreatitis, short bowel syndrome, etc.).
Most types of fatty acids are absorbed in the proximal intestine, and reduced absorption leads to loss of calcium as it binds to fats.
This factor leads to a lack of calcium to bind oxalates in the distal parts of the digestive tract and a sharp increase in oxalate reabsorption.
Other factors leading to hyperoxalaturia include diarrhea, which leads to decreased diuresis and decreased urinary excretion of magnesium ions.
Intestinal dysbiosis plays a major role in the development of the intestinal form of hyperoxalaturia, as a result of which the number of colonies of bacteria that break down intestinal oxalates (Oxalobacter formigenes) decreases.
Figure 1 - Bipyramidal calcium oxalate crystals in urine. Photo source: Renal complications of jejuno‐ileal bypass for obesity. DR Mole CRV Tomson N. Mortensen CG Winearls
Excess
Excessive levels of oxalate in the blood is called hyperoxalemia
, and high levels of oxalate in the urine are called hyperoxaluria.
Acquired
Although uncommon, oxalate consumption (such as grazing animals on oxalate-containing plants such as Bassia hyssopifolia
, or human consumption of sorrel or, especially in excessive quantities, black tea) can lead to kidney disease or even death due to oxalate poisoning.
The New England Journal of Medicine
reported acute oxalate nephropathy "almost certainly due to excessive consumption of iced tea" in a 56-year-old man who drank "sixteen 8-ounce glasses of iced tea per day" (approximately 3.8 liters).
The authors of the article hypothesized that acute oxalate nephropathy is an underdiagnosed cause of renal failure and suggested a careful review of the patient's dietary history in cases of unexplained renal failure without proteinuria (excess protein in the urine) and with large amounts of calcium oxalate in the urine sediment.[40] ] Oxalobacter formigenes
in the intestinal flora may help alleviate this.[41]
Congenital
Main article: Primary hyperoxaluria
Primary hyperoxaluria is a rare hereditary disorder that results in increased oxalate excretion, and oxalate stones are common.
Alimentary form
As stated earlier, the absorption of oxalic acid from food is normally low, so this form of hyperoxaluria is rare in isolation. It is often combined with a hereditary predisposition and impaired absorption in the intestine.
The nutritional form of hyperoxaluria can occur in people who abuse tea, coffee, chocolate, cocoa, sorrel, beans, as well as synthetic vitamins, in particular ascorbic acid.
Nutritional hyperoxaluria can also be caused by a poor and monotonous diet with deficiencies in B vitamins, magnesium and calcium, which are involved in the metabolism of oxalic acid.
Clinical picture
In the vast majority of cases, oxalates in urine are an incidental diagnostic finding. Hyperoxaluria is often completely asymptomatic, especially in the initial stages. The following symptoms may appear:
- 1Decreased volume of urine excreted;
- 2 Acrid and unpleasant odor of urine.
Due to irritation of the genital skin with oxalates, redness and inflammation of the urethra, labia (in women), and glans penis (in men) can develop.
A secondary infection may occur and symptoms such as burning and pain when urinating, pain in the suprapubic area, and increased urge to urinate.
Upon visual inspection, the urine is cloudy and does not have the usual transparency; if you leave it in the container for a while, you can detect sedimentation.
In a general urine test, hypersthenuria is required (increased relative density above 1030). With the long-term existence of crystalluria, microhematuria, proteinuria, and abacterial leukocyturia gradually appear.
If such symptoms are detected, we can talk about the development of dysmetabolic nephropathy.
Diagnostic methods
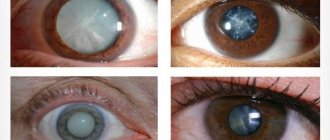
In the OAM with hyperoxaluria, specific colorless oxalate crystals are detected in the urinary sediment, the presence of which in quantities of more than 0.57 mg/kg/day confirms the diagnosis of hyperoxaluria.
In nephrology hospitals, it is possible to conduct tests to study the anti-crystal-forming ability of urine to calcium oxalate and determine the activity of membrane peroxidation.
With calcium oxalate crystalluria in the urine, the presence of specific crystals of calcium oxalates, differing in structure and type, can be detected.
| Type of stone | Development conditions | Peculiarities | Relation to X-rays |
| Wewellite (calcium oxalate monohydrate) | Excess oxalic acid in urine | The crystals look like biconvex ovals, similar in appearance to red blood cells, their core is brown-black in color and high hardness | X-ray positive |
| Weddellite (calcium oxalate dihydrate) | High levels of oxalic acid, calcium and magnesium in urine | The crystals are pyramidal in shape, weakly refract rays, loose, light yellow in color | X-ray positive |
Table 1. Types and structure of calcium oxalate stones
So, the diagnosis of hyperoxaluria (oxaluria) is established on the basis of:
- 1Increased oxalate content in biochemical urine analysis (norms depend on the age and weight of the patient);
- 2Detection of oxalate crystals in a general urine analysis (it is advisable to repeat the analysis at intervals of a week);
- 3The content of red blood cells in the urine according to a general analysis or Nechiporenko’s test is within normal limits and slightly increased;
- 4The amount of protein in the urine is normal or ranges from 0.033-0.066 g/l;
- 5 Positive tests for markers of membrane instability, decreased anti-crystal-forming ability of urine.
24-hour urine salt test
If it is necessary to assess the total amount of salts excreted during the day, the doctor orders urine to be collected in a glass container, after which an analysis is performed. Typically, urine collection occurs at home, and the reliability of the results is influenced by several indicators:
- 3-5 days before the expected date of urine collection, you need to normalize your diet by giving up spicy, salty, sour and smoked foods, alcohol and sweet carbonated drinks.
- Reduce physical activity and consume enough fluid, at least 1.5 liters per day.
- Before each urine collection, it is important to disinfect the genitals by washing with baby soap.
After waking up at 6 am, the first portion of urine is not counted.
Next, the urine is collected in a glass jar with a volume of at least 3 liters. The last portion of urine should be at 6 am the next day.
The jar of urine is stored in a cool, dark place, but not in the refrigerator. The ideal option is a tiled bathroom floor.
After collecting the last portion of urine, close the jar tightly with a lid and shake vigorously. After this, 100 ml is measured into a urine collection container, which is taken to the laboratory. The container is signed, after which laboratory assistants study the quantitative and qualitative composition of the salts.
After the study, results are given on the percentage and quantitative content of salts, on the basis of which the doctor makes a conclusion.
Treatment tactics
Treatment of hyperoxaluria must be prescribed. Therapy is a complex of medicinal and non-medicinal procedures, including therapeutic nutrition, adequate drinking regimen and taking herbal medicines with a uroprotective effect.
The diet for hyperoxaluria in children and adults includes:
- 1Balanced nutrition, taking into account the age-related needs of the body and optimal calorie content;
- 2 Complete exclusion of products high in oxalic acid (chocolate, cocoa, sorrel, spinach, parsley, rhubarb, beans, nuts, beets);
- 3 Limiting foods with moderate oxalate content (currants, sour apples, beans, tomatoes, citrus fruits, buckwheat);
- 4 Limiting foods rich in vitamin C (rose hips, sea buckthorn, cauliflower, etc.);
- 5 Calcium intake from food should be approximately 1300-1400 mg/day;
- 6Fluid intake should be at least 50 ml/kg per day;
- 7It is recommended to take slightly alkaline mineral waters.
To correct metabolic disorders in hyperoxaluria, nutritional therapy should be prescribed for a period of at least 6 months. The decision to extend the diet depends on the severity of urinary syndrome.
Dietary restrictions should be followed daily, or intermittently 1-2 days a week. In addition to normalizing nutrition, it is imperative to correct all existing types of digestive disorders (intestinal diseases, impaired fat absorption, etc.)
Occurrence in nature
Oxalate is found in many plants, where it is synthesized by incomplete oxidation from carbohydrates.
Plants rich in oxalates include: fatty chicken ("lamb"), sorrel, and several Oxalis
variety.
Rhubarb root and/or leaves and buckwheat are high in oxalic acid.[28] Other edible plants that contain significant concentrations of oxalate include, in descending order, carambolas (carambola), black pepper, parsley, poppy seed, amaranth, spinach, chard, beets, cocoa, chocolate, most nuts, most berries, fishtail palms, New Zealand spinach ( Tetragonia tetragonioides
), and beans. [
citation needed
] The leaves of the tea plant (
tea bush
) contain some of the highest measured concentrations of oxalic acid compared to other plants. However, the drink produced by infusion in hot water usually contains low to moderate amounts of oxalic acid due to the small mass of the leaves used for brewing.
| Common foods that are high in oxalates[29] | ||
| Food | Service | Oxalate Content (mg) |
| Beet greens, cooked | 1⁄2 cup (unit) | 916 |
| Purslane, leaves, cooked | 1⁄2 cup | 910 |
| Rhubarb, no sugar | 1⁄2 cup | 860 |
| Spinach, cooked | 1⁄2 cup | 750 |
| Beets, cooked | 1⁄2 cup | 675 |
| Chard, Swiss, leaves, cooked | 1⁄2 cup | 660 |
| Rhubarb, canned food | 1⁄2 cup | 600 |
| Spinach, frozen | 1⁄2 cup | 600 |
| Beet pickled | 1⁄2 cup | 500 |
| Poke greens, cooked | 1⁄2 cup | 476 |
| Endive, raw | 20 long leaves | 273 |
| Cocoa, dry | 1⁄3 cup | 254 |
| Dandelion greens, cooked | 1⁄2 cup | 246 |
| Okra, cooked | 8–9 capsules | 146 |
| Sweet potatoes, cooked | 1⁄2 cup | 141 |
| Cabbage, cooked | 1⁄2 cup | 125 |
| Peanuts, raw | 1⁄3 cup (1 3⁄4 ounce) | 113 |
| Turnip greens, cooked | 1⁄2 cup | 110 |
| Chocolateunsweetened | 1 oz | 91 |
| Parsnips, diced, cooked | 1⁄2 cup | 81 |
| Cabbage greens, cooked | 1⁄2 cup | 74 |
| Pecans, halved, raw | 1⁄3 cup (1 1⁄4 ounce) | 74 |
| Tea, leaves (4-minute infusion) | 1 level teaspoon per 7 fl oz water | 72 |
| Cereal germ, toast | 1⁄4 cup | 67 |
| Gooseberry | 1⁄2 cup | 66 |
| Potatoes, Idaho white, baked | 1 medium | 64 |
| Carrots, cooked | 1⁄2 cup | 45 |
| apple, raw skin | 1 medium | 41 |
| Brussels sprouts, cooked | 6–8 average | 37 |
| Strawberries, raw | 1⁄2 cup | 35 |
| Celery, raw | 2 stems | 34 |
| Milk chocolate bar | 1 bar (1.02 oz) | 34 |
| Raspberry, black, raw | 1⁄2 cup | 33 |
| orange, edible part | 1 medium | 24 |
| green beans, cooked | 1⁄2 cup | 23 |
| Garlic, raw, chopped | 1 tablespoon | 19 |
| Leeks, raw | 1⁄2 average | 15 |
| Blackberries, raw | 1⁄2 cup | 13 |
| Concord grapes | 1⁄2 cup | 13 |
| Blueberries, raw | 1⁄2 cup | 11 |
| Red Ribes | 1⁄2 cup | 11 |
| Apricots, raw | 2 medium | 10 |
| Raspberry, red, raw | 1⁄2 cup | 10 |
| Broccoli, cooked | 1 large stem | 6 |
| Cranberry juice | 1⁄2 cup (4 ounces) | 6 |
Physiological effects
Scanning electron micrograph of the surface of a kidney stone showing tetragonal crystals of veddelite (calcium oxalate dihydrate) emerging from the amorphous central part of the stone;
The horizontal length of the pattern is 0.5 mm from the figured original. In the body, oxalic acid combines with a divalent metal. cations such as calcium (Ca2+) and iron(II) (Fe2+) to form crystals of the corresponding oxalates, which are then excreted in the urine as tiny crystals. These oxalates can form larger kidney stones that can clog the kidney tubules. It is estimated that 80% of kidney stones are formed from calcium oxalate.[30] Those with kidney disorders, gout, rheumatoid arthritis, or some forms of chronic pain in the vulva (vulvodynia) are generally advised to avoid foods high in oxalic acid.[ citation needed
]. Currently, methods for reducing oxalate content in food are relevant.[31]
Magnesium (Mg2+) oxalate is 567 times more soluble than calcium oxalate, so the latter is more likely to precipitate when magnesium levels are low and calcium and oxalate levels are high. Magnesium oxalate is a million times more soluble than Mercury oxalate. The solubility of oxalates in metals decreases in the following order: Mg > Ca > > Zn > {Mn, Ni, Fe, Cu} > {As, Sb, Pb} > Hg.[ doubtful - discuss
]
The highly insoluble iron(II) oxalate appears to play an important role in gout, in the nucleation and growth of the otherwise highly soluble sodium urate. This explains why gout usually appears after age 40. [32] when ferritin level in the blood exceeds 1 μg/L [ citation needed
]. Foods high in oxalates[33] should be avoided by people who have or are at risk of gout.[34]
Cadmium catalyzes the conversion of Vitamin C to oxalic acid. This may be a problem for people exposed to high levels of cadmium in their diet, in the workplace, or through smoking.
In studies in rats, calcium supplements administered along with foods high in oxalic acid can cause precipitation of calcium oxalate in the intestine and reduce the level of oxalate absorbed by the body (in some cases by 97%).[35][36]
Oxalic acid can also be produced from the metabolism of ethylene glycol ("antifreeze"), glyoxylic acid, or ascorbic acid (Vitamin C).[37][ doubtful - discuss
]
Powdered oxalate is used as a pesticide in beekeeping to combat bee mites.
Some mushrooms from the genus Aspergillus
produce oxalic acid.[38]
Some preliminary data indicate that administration of probiotics may have a positive effect on the rate of elimination of oxalic acid.[39]