Diabetic nephropathy (DN) is kidney damage that develops in patients with diabetes mellitus types 1 and 2, manifested by an increase in the excretion of proteins, mainly albumin, in the urine, as well as increased blood pressure and progressive renal failure.
The prevalence of this disease has increased significantly in recent decades, due to an increase in the incidence of diabetes mellitus. In type 1 diabetes mellitus, at least 30% of patients develop DN at the age of 20-25 years. Kidney damage in type 2 diabetes usually develops after 15-20 years of the disease.
Causes of nephropathy
The modern medical theory of the development of this type of pathology is based on the influence of several provoking factors. It is believed that nephropathy appears only in weak people with a susceptible body and is often inherited. Patients whose immediate family members had renal pathologies are at serious risk of developing nephropathy.
Causes of nephropathy:
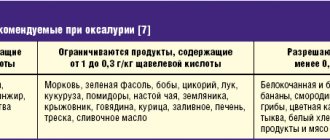
- Problems with metabolism, due to which the circulation of glucose in the blood increases, the level of phosphates, urates, oxalates and other impurities. When passing through the kidneys, these substances cause damage to the glomerular system and destroy it.
- Impact of environmental toxins. Alcohol drinks, tobacco products, other psychotropic drugs, industrial poisons, radiation have a destructive effect on the functioning of the genitourinary system.
- The deterioration of blood supply to the kidneys is provoked by an increase in atherosclerotic plaques, the appearance of deposits on the walls of blood vessels, and a decrease in capillary permeability.
What causes nephropathy? The causes may be congenital or acquired.
Congenital factors:
- Disorders caused by connective tissue defects.
- Difficulty contracting the bladder.
- Return tissue back to the pelvic system.
- Primary immunodeficiencies.
Acquired causes of nephropathy:
- Harmful working conditions.
- Injuries.
- Consequences of sepsis or toxin poisoning.
- Multiple pregnancy.
Overdose of medications often provokes the disease.
Causes
A characteristic feature of ischemic nephropathy is its close association with many other diseases affecting the cardiovascular system, metabolic processes, and endocrine glands. At the same time, some urologists consider true ischemic nephropathy only those forms that are caused by primary damage to the renal vessels, while other causes of arterial occlusion lead to similar, but somewhat different pathological processes. The scientific discussion regarding the causes of the disease continues; today, most nephrologists recognize the presence of the following etiological factors:
- Atherosclerosis of the renal vessels. It is possible to have both isolated damage to the vascular bed of the kidneys (renal atherosclerosis) and systemic formation of atherosclerotic plaques in various arteries of the body, which is often observed in elderly people. Deposits of lipid substances narrow the lumen of the arteries and impede perfusion, which causes ischemic changes in the renal tissue.
- Atherosclerosis of the abdominal aorta. Advanced forms of aortic damage can limit blood flow to the excretory system and provoke ischemia. In addition, cholesterol crystals can break off from plaques and enter the renal vessels, causing rapidly progressive renal failure due to tissue ischemia
- Autoimmune systemic pathologies. Diseases of blood vessels and connective tissues, accompanied by the formation of antiphospholipid antibodies, can affect the walls of small arterioles. This impedes blood flow and oxygen penetration to the kidney tissues, which is manifested by ischemia.
In newborns, ischemic kidney damage occurs due to dehydration, overheating, and hypovolemia. This causes a neurogenic spasm of the renal arteries with a sharp restriction of blood flow through them. In some extreme situations, a similar process can be observed in adults, leading to fulminant forms of ischemic nephropathy.
Symptoms and signs of nephropathy
Symptoms of nephropathy depend on the type of pathology. Some manifestations are considered common to different forms of the disease.
We list the signs of nephropathy:
- Increased fatigue and general weakness of the body.
- Intense thirst.
- Frequent headache.
- Tissue swelling.
- High blood pressure.
- My lower back hurts.
- A large amount of protein is concentrated in the urine.
When the disorder occurs due to diabetes, patients' blood pressure increases to a critical level. Doctors often observe severe swelling of the lower extremities. Nephropathy in pregnant women occurs quickly and provokes swelling of the face. Specific symptoms of nephropathy in men include blood in the urine and a sharp increase in pain. The gouty form of the disorder is not accompanied by any special symptoms. The diagnosis of nephropathy is difficult to make in the development of myeloma, since there are no symptoms of such a disorder.
With the development of nephropathy in women, the ability of the kidneys to filter decreases so much that internal intoxication increases significantly. Based on the results of the examination, nephropathy or a chronic form of renal failure at the first stage is diagnosed.
Signs of nephropathy in children:
- Mild abdominal pain.
- A burning sensation is felt during urination.
- Cloudy urine is produced.
- Blood pressure drops.
Signs become more pronounced in the hereditary form of the disorder in children. The stomach often hurts from an early age, the child feels discomfort in the joints. Urolithiasis develops at the last stage of nephropathy.
Pathological anatomy
The buds are swollen and slightly increased in size. The cortex is anemic, pale yellow, the medulla is dark red. Mostly dystrophic changes are found in the kidneys. The microscopic picture is presented in the form of cloudy swelling and fatty infiltration of the epithelium of straight and convoluted urinary tubules, which can be filled with granular and hyaline masses. The endothelium of glomerular vessels is affected less frequently. Inflammatory changes at night are observed in cases where N. b. develops against the background of glomerulonephritis (see). Hemorrhages into the renal parenchyma and infarctions are rarely detected.
How to treat nephropathy
The disease is diagnosed by laboratory tests.
Diagnostic methods:
- Visual inspection.
- Studying the patient's medical history.
- Palpation.
- Blood analysis.
- Ultrasonography.
If necessary, specialists conduct other tests to obtain specific information regarding the general condition of the patient. Based on the information obtained, a detailed anamnesis is formed and treatment for nephropathy is prescribed. Urine is analyzed to determine the amount of salts, proteins and measure the specific gravity of the liquid.
How to treat nephropathy? All procedures at the initial stages are carried out in a hospital setting.
Set of measures:
- Normalization of kidney condition.
- Elimination of puffiness.
- Blood pressure control.
- Daily urination improves.
- Improves blood supply to diseased organs for the treatment of nephropathy.
- Provides general health.
Concomitant pathologies are also treated, since they often cause nephropathy.
Medicines for the treatment of nephropathy:
- Diuretics.
- Drugs that normalize potassium and magnesium levels.
- Vitamins.
- Medicines that promote blood circulation.
- Means for regulating pressure.
- Anti-inflammatory and antibacterial drugs.
To improve the acid-base balance and regulate the amount of salts, a dropper with saline solution is placed. To prevent the kidneys from being destroyed, hemodialysis is performed in the treatment of nephropathy; the breakdown products of toxic microelements are eliminated from the body. The procedures are performed using special medical equipment.
How to cure nephropathy with folk remedies? Doctors recommend taking medications. Traditional medicine is used to keep the body normal and eliminate unpleasant symptoms.
Recipe:
- St. John's wort, yarrow, nettle and coltsfoot are crushed.
- The ingredients are mixed in equal proportions.
- Fill with hot water and set up in a dark place.
Treatment of nephropathy lasts 25 days.
Treatment
All patients with Nephropathy of Pregnancy are subject to hospitalization. Outpatient treatment is permissible only in mild cases. The regimen is gentle, for severe N. b. and the threat of retinal detachment - bed. Creating emotional peace is achieved by prescribing valerian and tranquilizers. A diet with limited table salt (up to 2-3 g per day) and liquid (taking into account water balance). Patients receive proteins in the form of boiled meat, cottage cheese, fish; Fatty meats and smoked meats are excluded. Fruits, vegetables, juices, vitamins are needed. To combat edema, diuretics are prescribed orally, and in severe cases - intramuscularly or intravenously; potassium supplements are prescribed at the same time. Antihypertensive therapy is carried out. Infusion therapy allows you to fill the deficit of energy resources and plastic substances (glucose solution with insulin, hexose phosphate, plasma, albumin, protein, amino acid complexes). In order to detoxify and improve the rheological properties of the blood, hemodez, polydesis, low molecular weight polyvinyl alcohol, rheopolyglucin, etc. are administered. The normalization of the redox processes of the patient and the intrauterine fetus is facilitated by the introduction of a 5% solution of ascorbic acid, cocarboxylase, as well as oxygen therapy.
If complex treatment within three, maximum four weeks does not lead to improvement, the question of early delivery is raised. Therapy during labor continues. Pain relief for labor (see) is mandatory, while long-term epidural analgesia with trimecaine has undoubted advantages. If blood pressure is high during childbirth, controlled hypotension can be used, which is achieved by drip administration of 0.1% arfonade solution, 5% pentamine solution or other gangliolytic drugs. The introduction of Viadryl with Droperidol also reduces the risk of transition to N. b. in preeclampsia and eclampsia.
Stages and degrees of nephropathy
The disorder develops slowly and symptoms appear gradually. Nephropathy during pregnancy is considered one of the most serious complications. The reasons for the development of this disorder have not been fully studied. The risk group includes young women who abuse alcohol and tobacco products.
Let us list the stages of nephropathy:
- Diabetic.
- Nephropathy that occurs during pregnancy.
- Toxic disease.
- Gouty form of the disorder.
- Myeloma nephropathy.
- IGA nephropathy.
Dysmetabolic nephropathy is quite common. It is divided into the following types:
- Oxalate-Calcium.
- Phosphate-urate.
- Exchange.
In the diabetic form of the disease, the right and left kidneys are affected simultaneously.
Prognosis and Prevention
The prognosis depends on the time of onset of N.'s symptoms. (the prognosis is much worse if nephropathy develops before 30 weeks of pregnancy), the presence of previous somatic pathology, the duration of toxicosis; Timely and adequate treatment in the vast majority of patients allows the pregnancy to end successfully. Late treatment and insufficiently intensive treatment worsens the prognosis: after childbirth, hypertension often persists, vision deteriorates, and chronic kidney disease develops.
Prevention consists of timely identification and treatment of dropsy in pregnancy, preclinical signs of Nephropathy in pregnant women. Such diseases. such as hypertension, nephritis, diabetes mellitus, etc., against the background of which nephropathy in pregnant women usually develops, are subject to intensive treatment before pregnancy. If they are present, a woman who wants to have a child should be examined by various specialists to decide on the possibility of having a child.
See also Toxicoses of pregnant women.
Bibliography:
Becker S. M. Pathology of pregnancy, L., 1975; Bodyazhina V.I. and Shmakin K.N. Obstetrics, M., 1979; Practical obstetrics, ed. Y. P. Solsky, p. 240, Kyiv, 1977; Slepykh A. S., Repina M. A. and Gladun E. V. Hemorrhagic shock in obstetrics, Chisinau, 1979; Toxicoses of pregnant women, ed. Yu. I. Novikova, p. 83, L., 1973; James F. M. Epidural analgesia and anesthesia in obstetrics, NC med. J., v. 32, p. 5, 1971; Willocks J. a. Moir DD Epidemiological analgesia in the management of hypertension in labor, J. Obstet. Gynaec. Brit. Comm., v. 75, p. 225, 1968.
V. P. Baskakov.
Prevention of nephropathy
The main measures to prevent nephropathy are diet. Doctors individually develop a diet for each patient, taking into account his condition. Products with low amounts of protein are used.
The menu includes the following food:
- Berry fruit drinks.
- Fermented milk products.
- Low fat fish fillet.
- Cooked meat.
- Parsley, dill, other greens.
To prevent nephropathy, all products are steamed or boiled, and a minimum amount of salt is used.
Pathogenesis
Often the cause of ischemic nephropathy is atherosclerotic changes in the renal vessels, caused by the deposition of cholesterol and lipids on the walls of arteries and arterioles. In a certain proportion of patients, kidney damage is caused by an inflammatory reaction, sometimes of an autoimmune nature. All this leads to a decrease in the width of the lumen of the vessels and thereby impedes the flow of blood to the kidney tissues.
Insufficient oxygen and nutrients lead to gradual degeneration of nephron cells, especially tubular epithelium, which then undergo autolysis and necrosis. The death of the nephron is accompanied by the growth of connective tissue, which is less demanding on the volume of oxygen supplied to the blood. A decrease in the volume of blood flow through the kidneys leads to a slowdown in filtration and purification of blood from metabolic products. This phenomenon is further aggravated by the death and decrease in the number of active nephrons and affects the functioning of the entire organism.
Hypoperfusion of the juxtaglomerular apparatus leads to increased formation of angiotensin 2 and the development of renovascular hypertension, which accelerates the formation of atherosclerotic plaques. The combination of these pathogenetic processes leads to a complex and varied picture of ischemic kidney disease. At the terminal stages of the disease, due to a sharp decrease in the number of nephrons and the progression of vascular disorders, chronic renal failure occurs, often of a terminal nature.
Treatment of ischemic nephropathy
Therapeutic prescriptions are limited to supportive treatment and elimination of pathologies that contribute to renal hypoperfusion. In the case of acute and rapidly progressive forms, intensive therapy may be required to save the patient's life. In some situations, they resort to surgical treatment methods aimed at eliminating the main element of kidney damage - reduced perfusion. These include stenting of the renal arteries to eliminate stenosis and endarterectomy to remove atherosclerotic plaques. Conservative treatment is carried out using the following groups of drugs:
- Lipid-lowering drugs. High levels of lipids in the blood are a central link in the development of atherosclerosis, so the use of drugs in this group allows you to slow down the growth of lipid plaques. Long-term use of atorvastatin, lovastatin and similar drugs significantly reduces the rate of progression of ischemic nephropathy.
- Antihypertensive drugs. Elevated blood pressure is a consequence of nephropathy, but also accelerates its progression. The use of ACE inhibitors reduces blood pressure levels and the load on the excretory system. The use of strong antihypertensive drugs should be avoided - their use can cause reflex narrowing of the renal arteries and acute renal ischemia.
- Other auxiliary drugs. According to indications, cardioprotectors, infusion therapy to correct the electrolyte balance in the body, and prednisolone to reduce the oxygen demand of kidney tissue may also be prescribed. In the presence of concomitant diseases (diabetes mellitus, obesity), treatment regimens are developed taking into account the reduced function of the excretory system.
An important role in slowing down ischemic processes in the kidneys is played by proper adherence to the water regime, giving up bad habits (especially drinking alcohol), and taking certain medications (nephrotoxic antibiotics, some NSAIDs). You should also limit your salt intake and adhere to a diet with low lipid content in your diet. The duration of conservative therapy and auxiliary measures is quite long, they are often prescribed for life. With a sharp decrease in kidney function, hemodialysis is used.
Symptoms of ischemic nephropathy
A feature of the disease is a long period of asymptomatic progression and extremely slow development. The first complaints and characteristic symptoms of the torpid variant of the pathology arise already with a pronounced decrease in the functional activity of the kidneys. Patients complain of a decrease in the volume of diuresis (oliguria), frequent urges at night (nocturia), swelling of the limbs and facial tissues. Possible deterioration in general condition - weakness, decreased performance, fatigue.
Over time, the listed manifestations increase and turn into chronic renal failure - in addition to edema and impaired urine formation, an unpleasant (ammonia) odor from the mouth and skin irritation occur. Terminal chronic renal failure is also characterized by changes in the psycho-emotional state of the patient - he becomes irritable, mood swings occur, and suicidal tendencies are possible. Disturbances also affect other systems of the body: the gastrointestinal tract includes frequent diarrhea, nausea, and appetite disturbances.
A shift in water-ion balance leads to hyperkalemia, manifested by disorders of the muscular system and abnormal heart rhythms. At the final stages of development of ischemic nephropathy, the kidneys practically lose their function - anuria develops with the formation of less than 50 milliliters of urine per day. Without the use of hemodialysis, a patient at this stage of the torpid form of pathology may die from uremia.
Other forms of the disease are characterized by a much more rapid course. Thus, rapidly progressive ischemic nephropathy is manifested by lower back pain, a sharp decrease in diuresis and the development of anuria with edema and electrolyte disturbances characteristic of acute renal failure. It is often preceded by numerous episodes of renal infarction caused by embolization of their vessels by cholesterol fragments. The acute form is characterized by an even more rapid onset of acute renal failure, as well as a severe condition of the patient, up to coma or shock. In both cases, urgent resuscitation measures are necessary.