Beginning of puberty
Normally, puberty begins in girls between the ages of 8 and 13
, and
in boys
a little later -
from 9 to 14 years
.
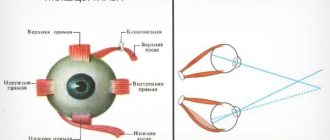
This process is triggered by hormones that are produced in the hypothalamus and pituitary gland: GTRH, LH, FSH. Exactly when a boy or girl begins to grow up is influenced by many factors. Genetics
plays a significant role . If the parents started puberty early, then most likely the child will experience it earlier than other children. And vice versa. Interestingly, this pattern is more often observed among fathers and sons.
— The process of puberty is also influenced by how the pregnancy and childbirth proceeded, whether there were any complications, what medications the mother took during pregnancy and breastfeeding, how the child grew and developed after birth, what illnesses he had, what physical problems he had load, whether he was exposed to stress
.
In general, puberty in modern children occurs a year and a half earlier than in previous generations. The doctor connects this with the harmful factors that our society has encountered, in particular “pseudohormones”
.
— These are chemicals of anthropogenic origin: pesticides, bisphenol A, phthalates, which are contained in food products; used for the production of plastic products, consumer goods, and synthetic detergents. They are “built into” the human body and can lead to various diseases, including disrupting the process of puberty.
The doctor also draws attention to the problem of obesity among modern children. Overweight
negatively affects puberty: it can start too early or, conversely, late. There is another negative point:
- If you are overweight, an imbalance occurs between female and male hormones - estrogens and androgens, and this is fraught with consequences. An excess of male hormones in girls can cause menstrual irregularities.
and excess body hair growth.
Overweight boys may experience a decrease in the amount of male hormones ,
which will slow down the process of puberty.
The opposite situation, when teenagers go on strict diets
.
— Deficiency or sudden weight loss can lead to disruption of puberty. But this affects fertile function, that is, the ability to become parents in the future,” explains the doctor.
Signs of puberty in boys
Due to the active production of testosterone, boys
begin to mature from about 9 years of age. The first sign is an enlargement of the testicles in the scrotum. Then, at the age of about 10-11 years, the child develops pubic and axillary hair growth. At the age of 12-13 years, the male genital organ increases - first in length, and then in thickness.
— Frequently, at a doctor’s appointment, worried parents ask if everything is okay in the boy’s “pants” and whether the genitals are of normal size. You need to understand that it increases in size not at the beginning of puberty, but in the middle of the process. And the main significance for a boy, as a man in the future, is not the size of the penis, but the size of the testicles. It is in them that the “main” male hormone is produced - testosterone. Here's what parents need to pay attention to.
The standard pattern of growing up for boys
like this: first - enlargement of the testicles, then - active hair growth and enlargement of the penis. If the sequence is different, parents need to contact a pediatric endocrinologist. The doctor will find out whether this is normal or pathological.
— It’s worth mentioning separately about the first wet dreams
- involuntary ejaculation, which most often occurs at night at the age of 13-15 years. This is the norm and one of the manifestations of puberty. Parents should not worry about this. But you need to prepare the child for such changes in his body so that he has an idea about it in advance.
At the age of 13-15, boys begin to develop the beginnings of a mustache and beard. These are single small hairs, more like fluff. Only by the age of 16-20 do they become tougher and turn into male stubble.
In addition to active hair growth and changes in the genital organs, adolescents aged 13-15 experience a growth spurt :
boys begin to grow by 8-12 cm per year. After 3-4 years, the growth rate decreases.
Secondary sexual characteristics also appear: changes in the cartilage of the larynx and “breaking” of the voice, an increase in the width of the shoulders. This is influenced by the main male hormone - testosterone, which is produced in boys in the testicles.
Causes of mycopenia syndrome
The formation of external genitalia in boys during the embryonic period requires a significant amount of androgenic hormones. A decrease in testosterone biosynthesis in the embryonic testicle or a defect in the activity of its enzymes (5a-reductase activity) disrupts the masculinization of the external genitalia up to the formation of false male hermaphroditism, and also affects the size of the external genitalia and the formation of a micropenis in the child.
Micropenia is a symptom of many congenital endocrine abnormalities that occur with hyper- or hypogonadotropic hypogonadism - insufficient production of testosterone and/or hormones that activate its production (LH and FSH).
The causes of micropenia syndrome may be:
| View | Cause | Manifestations |
| Isolated micropenis | Incomplete resistance (tissue insensitivity) to sex hormones, especially in the prenatal period, negative effects on the fetus | Possible combination with hypoplasia of the cavernous bodies |
| Micropenis with hypogonadism (impaired production of hormones: testosterone, LH and FSH) | In case of dysfunction of the adenohypophysis, testicular tissue, a combination of primary and secondary hypogonadism | Micropenis + specific disease symptoms |
| Idiopathic micropenis | The cause is unknown in most cases. May be associated with the mother taking medications during pregnancy | Possible combination with hypoplasia of the cavernous bodies |
The most important stage of a child’s sexual development is puberty. During this period, a complex multi-stage restructuring of the hypothalamic-pituitary relationship occurs. As the testicles increase, the size of the penis increases: first the length, and then its diameter.
The lack of growth of the penis and testicles as the child grows older, in boys on average 12-14 years old, is a reason to consult a urologist and pediatric endocrinologist.
But there are also other reasons for the lack of penis growth in boys - functional delay in growth and puberty, severe somatic and infectious diseases. These reasons are associated with reversible changes in the pulsating physiological rhythm of the pituitary gland - hypothalamus - gonads, which are gradually normalized.
An important factor in micropenia and hypogonadism is obesity or malnutrition; they have different mechanisms, but when weight is normalized, the functioning of the hormonal system of the hypothalamic-pituitary relationship and their effect on the gonads is normalized.
False hypogenitalism is also noted - a fold of skin and fat hanging over the pubis and a fold of fat in the groin areas create the impression of underdevelopment of the penis and scrotum.
Signs of puberty in girls
Due to the active production of female sex hormones (estrogens), girls
begin puberty from about 8 years of age. Normally, first there is an enlargement of the mammary glands, then there is active growth of hair in the armpits and pubic area.
— If parents notice that a girl’s mammary glands are not enlarged, but there is pubic and axillary hair, then it is better to consult a doctor. This may be due to increased production of androgens (male hormones).
Girls usually start menstruating between the ages of 11 and 13 .
. As a rule, before this, light, non-bloody discharge appears, and there may also be pain in the lower abdomen.
— The duration of the first menstruation can vary from 3 to 7 days, and they occur after 21-40 days. It is important to understand that the menstrual cycle in girls is not established immediately. Within 2-3 years after the start of the first menstruation, disruptions may occur. This is fine. But if more than 3 months have passed since the first menstruation, and the next one has not arrived, you need to contact a gynecologist or endocrinologist.
The abundance and pain of menstruation depends on various factors: nutrition, disease, heredity. These issues should be discussed individually with your doctor.
At the same time, girls develop secondary sexual characteristics: an increase in the size of the pelvis and redistribution of subcutaneous fat according to the female type (fat deposition on the buttocks and thighs). It is important to tell the girl about this so that she is not afraid of how her figure is changing.
- But it is important to watch your diet ,
because during this period teenagers’ appetite increases, warns the doctor. — If a girl begins to actively eat carbohydrate foods, excessive weight gain may occur, which is fraught with complexes and health problems.
Micropenia Clinic
The diagnosis of micropenis is made based on correctly measured penis length.
If the length of the elongated penis is 2.5 standard deviations less than that of the average patient with normal internal and external male genitalia, a diagnosis of micropenia is made.
Individual variations of puberty are also distinguished, which includes the growth of the penis in length.
But at the same time, in the case of late and/or slow puberty in boys, constant monitoring by a pediatric urologist-andrologist and a pediatric endocrinologist is required.
The scrotum in some cases may be underdeveloped. The testicles are located in the scrotum, but their function may be reduced. Some patients experience difficulty descending the testicles (cryptorchidism).
Testicular volume is often below normal values.
Micropenia is a symptom of many congenital endocrine abnormalities occurring with hyper- or hypogonadotropic hypogonadism.
| Klinefelter syndrome is a pathology of the sex chromosome, manifested by the presence of at least one extra X chromosome (47XXY) or a mosaic karyotype. Before puberty, boys may exhibit cryptorchidism and a small penis. The pubertal period is characterized by gynecomastia, tall stature, and eunuchoid body proportions. The size of the testicles remains pre-pubertal, their consistency is dense. This syndrome is characterized by a 47XXY karyotype, hypergonadotropic hypogonadism (testicular hypoplasia and micropenia), infertility, reduced body hair, gynecomastia, decreased intelligence, bone deformation and high stature. Karyotyping is indicated. |
| XX men - the penis and scrotum are formed according to the male type, however, the penis can be shortened, and hypospadias occurs. The internal genital organs correspond to the male gender. The testicles at puberty remain small and dense, as in patients with Klinefelter syndrome. Adult XX men are capable of sexual activity, but they are infertile. The levels of LH and FSH are increased. |
| Nuan syndrome is associated with mutations in the PTPN11 gene (12q24.1) or mutations in the SOS gene (2p22-p21). It is manifested by cryptorchidism, micropenis and scrotal hypoplasia. In addition, some patients develop a clinical picture of eunuchoidism during puberty. Often with this syndrome, pterygoid folds on the neck, a triangular face, valgus deformation of the elbow joints, short stature, lymphatic edema of the hands and feet, ptosis, sunken chest, defects of the right heart, and mental retardation are detected. Low levels of testosterone in the blood are combined with increased levels of LH and FSH. |
| Anorchism syndrome is an intrauterine, genetically determined lesion of the gonads (INSL gene mutations at 19p). At birth, the external genitalia are formed correctly, but in some cases there is a micropenis and a decrease in the scrotum. Testicles are missing. Extragenital signs of hypogonadism develop after 12–14 years. There is no puberty during puberty. Involution of secondary sexual characteristics, obesity and eunuchoidism are observed. The blood has low levels of testosterone, but high levels of LH and FSH. The test with human chorionic gonadotropin (hCG) is negative. |
| Gonadal dysgenesis is quantitative and structural chromosomal aberrations; a gene mutation cannot be excluded. Irregular structure of the external genitalia is detected at the birth of a child. Clinical symptoms: the patient has a dysgenetic testicle, derivatives of paramesonephric (vagina, uterus, fallopian tubes) ducts and mesonephric (epididymis) ducts. |
| Isolated hypogonadotropic hypogonadism - decreased secretion of LH and FSH separately or both hormones simultaneously. Inherited autosomal recessively. At birth, the boy has underdevelopment of the scrotum, unilateral or bilateral cryptorchidism with inguinal dystopia of hypoplastic testicles, and micropenis. Before puberty, eunuchoidism, lack of puberty, tall stature, obesity, and gynecomastia develop. Levels of LH, FSH and testosterone in the blood are reduced. |
| Kallmann syndrome is a genetically heterogeneous hereditary disease manifested by pituitary hypogonadism in combination with anosmia (impaired sense of smell). Micropenis occurs with a gross defect in the secretion of LH-RH hormones. In some cases, other developmental anomalies may be present and include renal agenesis, cleft lip and/or cleft palate, selective dental agenesis, and bimanual synkinesis. |
| Prader-Willi syndrome is a neurogenetic multisystem disease that develops as a result of damage to the critical region of chromosome 15 (segment q11.2-q13). During the course of the disease, two phases can be distinguished: 1) the first is characteristic of children 12–18 months of age. It is characterized by severe muscle hypotonia, decreased Moro, sucking and swallowing reflexes, which makes feeding the child difficult; 2) the second - occurs later, after several weeks or months. It manifests itself as polyphagia, a constant feeling of hunger, leading to the development of obesity, and fat deposition is observed mainly on the trunk and in the proximal limbs. Muscle hypotension gradually decreases and almost completely disappears by school age. The feet and hands of patients are disproportionately small - acromicria. There are also other anomalies: 1) high, narrow forehead; 2) almond-shaped palpebral fissures with thin, drooping eyelids; 3) skin and hair are lighter than those of all other family members; 4) hypopigmentation of the iris; 5) delayed motor development; 6) microdontia, hypoplasia of auricular cartilage, scoliosis, glaucoma. Hypogonadism (hypoplasia of the penis and scrotum, cryptorchidism) is noted. The height of patients is often reduced. |
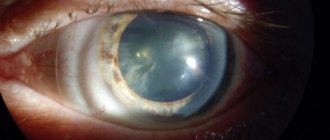
| Bardet-Biedl syndrome is a genetic pathology associated with ciliopathies. The disease is characterized by obesity, microgenitalism and cryptorchidism, oligophrenia, polydactyly, polycystic kidney disease, spastic paraplegia, and pigmentary retinopathy. LH and FSH levels are low. |
| Hyperprolactinemic hypogonadism - the secretion of gonadoliberin is inhibited and the frequency and amplitude of pulse secretion of LH decreases, the level of testosterone in the blood serum decreases. Boys in the prepubertal period develop eunuchoid body proportions: relatively long limbs, high waist, hips relatively wider than the waist of the lower limbs, fat deposits in the nipples, abdomen, and iliac crests, flabby and weak muscles, a high-pitched childish voice. The testicles and penis may be moderately hypoplastic. During puberty, secondary sexual characteristics may be absent. Sexual desire and fertility are reduced. |
| Incomplete form (Reifeinstein syndrome) - the structure of the external genitalia reflects varying degrees of androgen deficiency during fetal development. In children with this form, high-grade hypospadias with a divided scrotum is detected, micropenis, testicles are located in the split scrotum or in the inguinal canal. Histological examination showed an increased number of Leydig cells and impaired spermatogenesis. LH and testosterone levels are increased. |
| Leydig cell hypoplasia and agenesis is an autosomal recessive disease in which Leydig cell differentiation and testosterone synthesis are impaired. At birth, the external genitalia are formed correctly. The testicles are reduced, cryptorchidism is possible. At puberty, a clinical picture of eunuchoidism develops with obesity, underdevelopment of the external genitalia, and lack of sexual hair. The LH level is high, the concentration of testosterone and DHT is reduced, the hCG test is negative. The FSH level is normal in childhood, but decreased in puberty. |
| Defect 17 - reductase - an isolated disorder of testosterone synthesis (androstenedione is not converted into testosterone). Clinical symptoms in male patients include the manifestation of testosterone deficiency in the prenatal period (hypospadias), and later in the pubertal and postpubertal periods, symptoms of hypogonadism. However, androstenedione can be freely converted into estrogens. During puberty, gynecomastia may develop. |
| Congenital dysfunction of the adrenal cortex - various forms cause enzyme deficiency and cause abnormal structure of the external genitalia, which further increases the symptoms of hyperandrogenism, which manifests itself in boys as symptoms of false precocious puberty, and in girls the symptoms of virilization progress. Due to the excess amount of adrenal androgens, bone age accelerates, which causes eventual short stature. |
Micropenis is sometimes a symptom of congenital growth hormone deficiency or congenital hypopituitarism.
In some cases, the cause of micropenia cannot be determined. In such patients, endocrine dysfunction is not detected.
With functional delayed sexual development, when the external genitalia have a pre-pubertal appearance, adolescents, as a rule, do not have other signs of sexual development:
- voice mutation;
- facial hair;
- hypertrophy of the shoulder girdle;
- activity of sweat and sebaceous glands;
- growth retardation is observed.
The basal concentration of gonadotropic and sex hormones corresponds to pre-pubertal values. Functional tests with LR-RG help in diagnosis. In response to the introduction of the latter, the release of LH increases. The bone age of such adolescents lags behind the passport age by 2–3 years.
False micropenia (hidden penis) is spoken of when the penis is of normal size, correctly formed, has well-developed corpora cavernosa and a head, but is hidden by surrounding tissues. This picture is observed in obesity - the penis is hidden in excess subcutaneous fat, but is well removed from it. During puberty, some adolescents experience hormonal dysfunction.