What is conjunctivitis? Characteristics of the disease
Experts call conjunctivitis a disease that is characterized by an inflammatory process of the mucous membrane of the eye (conjunctiva). Most often, conjunctivitis occurs due to neglect of basic personal hygiene rules. But sometimes the reason
There may be another pathogen. In this regard, conjunctivitis occurs:
- infectious, caused by bacteria, infections, viruses, chlamydia and even fungi;
- non-infectious, provoked by an allergic reaction.
Moreover, such a reaction can be caused by anything: chemicals or external irritants, which also contribute to inflammation of the mucous membranes.
Types of complications after cataract removal
To reduce the risk of complications in the postoperative period, patients who have undergone lens replacement are advised to lead a healthy lifestyle, give up bad habits during the period of preparation for surgery, establish a routine for work, sleep and rest, and balance the diet, enriching it with foods that are beneficial for eye health. The stronger the immunity of a patient with cataracts, the more protective resources the body will have, which will be able to resist possible infections and complications.
Postoperative complications after cataract removal:
- Conjunctivitis is an inflammatory process in the mucous membrane of the eye; can be viral and bacterial, develops against the background of a weakening of the body’s protective functions.
- Uveitis is inflammation of the uvea of the eye; Conservative therapy is used for treatment; in most cases, the inflammatory process is stopped by the tenth day of treatment.
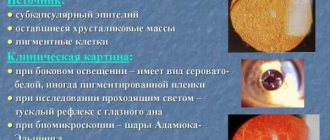
- Secondary cataract is a late complication, associated with opacification of the posterior capsule of the lens; As a preventive measure, capsule polishing techniques during cataract removal are effective, as well as the use of new types of lenses with a special architecture of supporting elements.
One of the most common complications after lens replacement is conjunctivitis. Viral and bacterial infectious agents often interact with the mucous membrane of the eyes, but a healthy, strong body copes with them, preventing spread. Due to dry eyes, which often occurs after cataract removal, the body's defenses are weakened, so the mucous membrane of the eyes becomes inflamed.
What are the symptoms of conjunctivitis?
How to navigate and understand whether you have conjunctivitis or not? Looking ahead, we note that under no circumstances should you begin the treatment process on your own. If, based on the symptoms listed below, it becomes clear that you are dealing with this particular disease, immediately contact a specialist. Do not delay, otherwise conjunctivitis may become chronic.
So, ophthalmologists talk about the following clinical picture of conjunctivitis:
- rapid eye fatigue, especially when reading or watching TV, when working at the computer;
- there is swelling of the eyelids;
- there is severe redness of the eyes;
- specific mucous or purulent discharge from the eyes;
- sensation of a foreign body in the eye, photophobia, blepharospasm.
In some cases, patients also complain of severe weakness, migraines, enlarged lymph nodes and increased body temperature.
Eye conjunctivitis: types and causes
The mucous membrane or membrane is called conjunctiva , it acts as a shield and has a protective function, protecting the eyes from infections, dust and fine particles, and is also involved in the process of tear production. This membrane is filled with small glands that produce water, fats and mucus, which are the main components of tears, designed to provide daily moisture and protect the eye.
There are also a large number of vessels in the conjunctiva, so when an infection occurs, redness of the eye is observed.
There are quite a few causes of the disease; depending on the etiology, there are several forms of conjunctivitis:
- Adenoviral conjunctivitis is a conjunctivitis that occurs due to an airborne virus entering the body; children who attend school or kindergarten often suffer from this type of conjunctivitis.
With this type of conjunctivitis, at the initial stage, not only the respiratory tract is affected, but also the lymph nodes, body temperature rises, a slight spasm of the eyelids is noticeable, and in children a film or follicle may appear.
Viral conjunctivitis can be determined by significant tear production, itching, sore throat and infection of the upper respiratory tract.
- Allergic – manifests itself directly upon contact with an allergen. Accompanied by itching, redness and swelling, as well as profuse lacrimation.
- Koch-Wicks conjunctivitis or acute epidemic conjunctivitis - enters the body with unwashed hands and objects on which germs are already located, most often occurs in children; the peak possibility of getting sick occurs in the hot summer time. It manifests itself as small blood effusions in the conjunctiva (protective membrane) on which swelling appears.
- Toxic – occurs as a result of contact with all kinds of toxic and dangerous substances. Accompanied by irritating pain when moving the eyes.
- Blenorrheal - this type of conjunctivitis affects newborns, the causative agent is gonococci. Infection occurs during childbirth from an infected mother. With this disease, serous-bloody discharges are released, which become purulent within a few days.
- to the stage of a chronic disease with prolonged irritation of the eye mucosa by contaminated air with chemical elements, smoke and dust. This disease also appears in people suffering from vitamin deficiency and metabolic disorders.
- Acute conjunctivitis occurs due to bacteria that are most easily picked up through dirty hands (staphylococci, streptococci, gonococci and pneumococci). Conjunctivitis is also provoked by overheating or hypothermia, processes that deplete the body as a whole, as well as resulting microtrauma to the conjunctiva.
With this form of the disease, the patient feels a cutting pain in the eyes, purulent yellow or gray mucus is released, which is also provoked by opportunistic or pathogenic bacteria. Because of this, the eyelids stick together. If there is no discharge, there may be a sensation of something extra in the eye. There is dryness near and inside the eye. First one eye is affected, then the second one becomes infected.
Diagnosis and treatment of the disease
After visiting a doctor, a specialist examines the patient. Then the doctor needs to take a smear or scraping of the discharge from the eye and send it to the laboratory. This will allow you to understand what type of conjunctivitis the ophthalmologist is dealing with. After research, the picture becomes clear, and treatment for conjunctivitis is prescribed.
Most often, to eliminate it, drops, ointments (for laying), as well as taking antibacterial medications are prescribed. Remember that the treatment of a disease such as conjunctivitis requires exceptional hygiene, so during treatment, use only disposable devices and wash your hands thoroughly.
Can you get viral and bacterial conjunctivitis during cataract surgery?
In clinics where eye surgery is performed, strict sanitary standards apply, so the risk of contracting conjunctivitis during cataract surgery is minimal. But it can still happen that when the lens is replaced, bacteria penetrate into the eye, and then the disease develops within a few hours. The patient is prescribed injections into the eye, intravenous infusions or eye drops. This type of infection is dangerous due to the development of endophthalmitis, an inflammatory process characterized by the accumulation of pus. Suppuration can extend beyond the eyeball and provoke sepsis and meningitis. Typically, this disease occurs as a result of injury or damage to the eyes, but it also happens during surgery, when the infection gets inside through a surgical incision.
Most cases of complications in the form of conjunctivitis after cataract removal are associated with the vulnerability of the body after surgery. Therefore, the therapeutic complex of measures prescribed to a patient who has undergone replacement of a clouded lens includes antibiotics and other drugs with an anti-inflammatory effect. Antibiotics reduce the risk of developing an infection. The doctor describes the regimen for using the drops. In the first days after replacing the lens, you need to apply eye drops frequently, up to 5 times a day; in the second week you can do this 2-3 times. But, even if you follow all the doctor’s recommendations, viral or bacterial conjunctivitis may develop. Its symptoms are recognized at an early stage.
Is it possible to work at a computer with conjunctivitis?
The question “is it possible to work at a computer” is perhaps one of the most common among patients who have experienced inflammation of the eye mucosa. At the moment, it is difficult to imagine a person who would not work behind a monitor, or whose activities were not associated with the active use of various gadgets. Experts recommend limiting the load on the visual organs during treatment, for at least one to two weeks. If it is not possible to completely exclude the computer during illness, the following rules should be followed:
- the computer should be at least 40 centimeters from the eyes, preferably on the left;
- you should take half-hour breaks every hour while working;
- In the morning and before going to bed, do not forget about lotions made from herbal decoctions (they are also prescribed by the doctor as a treatment);
- If you cannot limit yourself to watching TV or constantly interact with gadgets, then be sure to use additional lighting. This will allow your eyes to strain less;
- if your work involves numbers or letters, then in the computer settings you should increase the scale of all font groups;
- Every two hours you should perform gymnastics for the muscles of the visual organs.
Cataract surgery - features
It is impossible to get rid of lens opacities associated with age-related changes in the body without cataract surgery.
As soon as opacities affect the optical zone, and the quality of life of a patient diagnosed with cataracts deteriorates significantly, he is recommended to undergo lens replacement surgery. There is no longer any need to wait until the cataract is fully mature, because new cataract removal techniques allow this to be done at any stage. Due to the fact that fragments of the lens are removed from the eye in the form of an emulsion, and modern types of intraocular lenses are thin and inserted in a folded state, a specialist makes a small incision that does not require sutures. This means that a huge number of complications that were previously associated with prolonged healing are now practically absent, but there are some that still arise in the postoperative period.
Gymnastics for the eyes as one of the ways to relieve pain during conjunctivitis
Gymnastic exercises can also relieve pain, especially if you work at a computer during conjunctivitis. Ophthalmologists advise making circles with your eyes in one direction and then the other, blinking quickly (to improve blood circulation), moving your eyes to the right and left, moving your eyes to the bridge of your nose several times, drawing an infinity sign with your eyes in the air. Also, do not forget about the role vitamin complexes play in the fight against conjunctivitis. Thus, a lack of retinol affects visual acuity - it decreases, in turn, vitamin C works to strengthen blood vessels, and tocopherol is responsible for the tissue membrane that protects from UV rays and bright light. When it comes to natural products, beets and blueberries are considered the key players. They contain a lot of useful substances for vision and immunity of the visual organs.
Treatment of conjunctivitis after lens replacement
How is conjunctivitis treated if it appears after surgery? Depending on the cause of conjunctivitis, the doctor prescribes drugs whose action is aimed at eliminating the pathogen: bacteria or virus. The pathogen can be determined in the laboratory. To do this, the patient is asked to do a scraping and smear from the eyes, as well as donate blood for sensitivity to antibiotics. In case of bacterial conjunctivitis, the causative agent can be staphylococci, streptococci, chlamydia, and in case of a viral disease, the disease is provoked by herpetic viruses, adenoviruses and viral infections (mumps, chickenpox, rubella).
Complex therapy for the treatment of conjunctivitis:
- the use of eye drops with an anesthetic effect - this is necessary to relieve pain and for ointment therapy;
- antibacterial ointments that are placed under the lower eyelid;
- anti-inflammatory drugs that eliminate swelling and redness of the eyes;
- antibiotics - prescribed by a specialist, taking into account tests to determine the causative agent (bacteria) and sensitivity to drugs;
- antiviral drugs if the causative agent is viruses;
- antipyretics, painkillers and drinking plenty of fluids at high temperatures;
- washing the eyes with furatsilin solution.
It is better to wash your eyes with prescription medications to avoid allergic reactions to herbal preparations.
Rehabilitation after cataract surgery: regimen, diet, exercises
vitamins. If vitamin deficiency, depletion, weakened immunity are associated with a meager, unbalanced diet, it must be enriched with vegetables, herbs, fatty sea fish, dietary meats, and foods in which vitamins A, D, E, B6 and B12 predominate. It is also necessary to take vitamin complexes prescribed by your doctor. They should be prescribed during the treatment of conjunctivitis, then the course should be continued to consolidate the result. Unfortunately, with conjunctivitis, relapses are common if the body’s protective functions cannot be restored, so diet and fortification are extremely necessary.
Recovery after cataract removal and complications that arise:
- taking vitamin complexes;
- using moisturizing eye drops with vitamins - additional hydration of the eyes increases protective functions, prevents the passage of infection, and vitamins improve metabolism and improve blood flow to the organs of vision;
- gentle gymnastics for the eyes;
- adherence to the regime, diet, walks in the fresh air.
In the first month after cataract surgery, it is recommended to limit physical activity, but you should not completely give up visual stress. During this period, the human brain gets used to new optical conditions, it needs time to adapt, so you should perform various exercises: train to read books with large and small print, look at objects at different distances, etc. This way, vision recovery will be faster. To prevent recurrence of complications after cataract surgery, it is important to establish a work and rest schedule. An organism accustomed to a clear routine will be able to promptly respond to external threats and resist viral and bacterial infections.