Introduction
Eye injuries have firmly taken a leading place among the causes of visual disability in Russia, accounting for 22.8% of the number of persons recognized as disabled for the first time. The main task of healthcare is to prevent eye injuries and ensure optimal medical and social rehabilitation of victims. A retrospective analysis of the problem indicates the dependence of visual injuries on the social, domestic, military-political and criminal situation in the country and in the world. Analysis of the political and economic situation in the country allows us to predict the high relevance of scientific research in the field of ophthalmology in this direction (R.A. Gundorova, 1997). Injuries to the organ of vision can be divided into industrial, agricultural, household, and children's. Each type of injury has its own characteristics. Where to begin examining a patient with an eye injury?
First of all, it is very important to correctly and carefully collect an anamnesis of the injury: where, when and under what circumstances it occurred, what was the traumatic agent, and what is the mechanism of injury, the time elapsed from the moment of injury to the patient’s admission, vaccinations that were previously administered to the patient. Then they begin directly to study the ophthalmological status of the patient, which includes: 1. External examination of the eyelids and palpation of the bony edges of the orbit. 2. Inspection of the conjunctiva of the eyelids and transitional folds using the method of focal illumination of the eye and eversion of the eyelids. 3. Inspection and palpation of the lacrimal sac, determining the nature of its contents. 4. Detection of superficial and penetrating wounds of the cornea using fluorescein test and Seidel test. 5. Study of pupillary reactions. 6. Assessment of the color of the pupillary zone in transmitted color. 7. Checking visual acuity (at least approximate). 8. Approximate assessment of intraocular pressure. 9. Examination of the ocular media and fundus (if possible). The variety of injuries is difficult to fit into classification frameworks. There are injuries to the orbit, appendages of the eye and eyeball. It is rational to divide injuries into mechanical, thermal, chemical, radiant energy, vibration, toxic, etc. Mechanical injuries, in turn, are divided into blunt injuries (contusions) and wounds; the latter are penetrating and non-penetrating, and they separately distinguish through injuries. According to the severity of the injury, injuries are divided into mild, moderate and severe, but for the eyeball this classification is to a certain extent arbitrary, since it is difficult to predict the course of the wound process in the eye. With relatively mild injuries, especially penetrating ones, the course of the wound process in the eye can be severe.
Injury to the eyelids and conjunctiva
They look different and are often accompanied by associated injuries, which are not always determined by doctors at the place of residence. The size and appearance of the wound of the eyelid and conjunctiva may not correspond to the severity of the concomitant damage to the deeper parts. A mandatory study of visual acuity, media transparency and examination of the fundus is necessary. It is necessary to pay attention to the presence of subcutaneous emphysema, indicating damage to the paranasal sinuses and nasal bones. First aid is the introduction of PSS (1500-3000 units) according to Bezredka. Cleaning the wound with tweezers, a tupper, washing with peroxide and furacillin, treating the edges of the wound with alcohol (1% brilliant green solution). Applying an aseptic dressing. Then urgent surgical treatment of the wound is indicated, but in principle, sutures can be applied at any time after the injury (if there is no infection). A wound to the conjunctiva requires surgical debridement if there is divergence of the edges of the wound or the sclera is exposed, which indicates damage to Tenon's capsule. Diagnosis of subconjunctival scleral tears
The first symptom of subconjunctival rupture of the sclera, which ophthalmologists paid attention to, was prolapse of the lens under the conjunctiva (Mandelstamm, 1888).
In addition to prolapse of the lens, prolapse of the iris, ciliary body, choroid and vitreous body was often observed (Shereshevskaya, 1959, Zolotareva, 1961, etc.). These symptoms should be considered characteristic of subconjunctival scleral tears. More often, we encounter not the classic picture, but cases without the listed symptoms. When can a subconjunctival scleral rupture be suspected?
- chemosis of the conjunctiva, - extensive or limited subconjunctival hemorrhage, - the appearance of iris coloboma and displacement of the pupil, - sudden massive hemorrhage in the anterior chamber and vitreous body, - folds of Descemet's membrane, - decreased IOP, - transillumination of the choroid under the conjunctiva, - prolapse shells under the con-vu, - the glow of the rupture in the form of a red stripe during diaphanoscopy (Linnik, 1964). Diagnosis of scleral tears in the posterior pole of the eye is especially difficult. Observation of the patient and indirect symptoms help in diagnosis: prolonged hypotony of the eye and the presence of incorrect light projection in the patient, as well as ultrasound examination. There is no doubt that the listed symptoms are unequal in importance, however, it should be recognized that pronounced hypotension caused by injury almost always indicates a subconvalal rupture of the sclera. It should be said about the “pain point symptom”, which occurs when pressing with a glass rod after local anesthesia, in the area of a suspected rupture, causing severe pain. This symptom may indicate not only the presence of a rupture, but also its location. Subsequently, patients are subject to treatment in a specialized hospital.
Non-perforating wounds of the cornea and sclera
Corneal erosion is accompanied by significant pain, photophobia, lacrimation, and blepharospasm. A fluorescein test facilitates 100% diagnosis of this condition. The main task is to relieve pain and prevent infection of the defect. First aid, in addition to instillation of dicaine, consists of instilling drops containing antibiotics or sulfonamides and placing eye ointment behind the eyelids. Urgent surgical procedures are required in 2 cases: 1. A scalped wound of the cornea, when a layer of surface tissue has separated from it or the flap tends to wrap its edges and shift. 2. Foreign body in the layers of the cornea. It is removed with a spear or a needle, followed by scraping out the rust rim, otherwise the healing of the defect will take a long time. After removing foreign bodies, it is necessary to perform a Seidel color test, instill drops with an antibiotic or sulfonamides, apply an ointment and apply a bandage.
Bandage for wounds
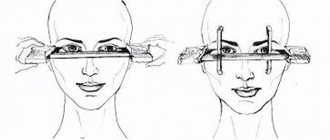
First aid for a penetrating eye injury consists in the obligatory application of a bandage to the injured eye, it does not matter whether it is right or left - the application procedure is the same. In this case, the dressing must be sterile, soft, elastic and hygroscopic (absorb moisture). Clean gauze is best for this.
If possible, it is recommended to additionally iron the material on the outside and back with a hot iron. The gauze needs to be folded in half and cotton wool distributed evenly between the layers. The material should only be touched with hands treated with alcohol. The finished bandage is secured with a simple plaster (to the skin of the forehead). You can also bandage your head with a simple sterile bandage.
Penetrating wounds of the eyeball
Any injury to the eyeball requires emergency care. Anamnesis, examination using focal illumination, examination in transmitted light, ophthalmoscopy, biomicroscopy, and x-ray examination usually make it possible to determine the nature of the damage - penetrating or non-penetrating. All perforated wounds are considered severe injuries and, regardless of their size and location, require hospital treatment. Direct signs of a perforated wound: - a through wound of the cornea or sclera, - a hole in the iris, prolapse of the membranes, - detection of a foreign body in the eye cavity, identified visually or on an x-ray. Indirect signs: - shallow or, conversely, deep anterior chamber, - deformation of the pupil, - traumatic cataract, - hypotony of the eye. Outpatient care:
1. instillation of anesthetic and disinfectant drops, 2. parabulbar administration of dexazone with an antibiotic, etamsylate, 3. administration of antitetanus serum and (or) toxoid, 4. intramuscular solution of a broad-spectrum antibiotic and painkillers, 5. review radiography of the orbit (if possible), 6. application of a binocular aseptic dressing, 7. referral of the patient to a hospital or ophthalmology department.
Treatment of perforated wounds is surgical. Penetrating injuries are often caused by a foreign body. With these wounds, there is always an entrance hole of various sizes and nature (depending on the size of the fragment) in the cornea or sclera. Most often, the entrance gate is the cornea, less often - the sclera - 63.7 and 21.2%, respectively (Gundorova R.A. 1975). The diagnosis of a penetrating wound is made on the basis of the following signs: exophthalmos with limited eye mobility, which is associated with hemorrhage in the retrobulbar tissue, absolute blindness that occurs immediately after the injury, associated with damage to the optic nerve, severe pain when moving the eyeball, the appearance of eyelid edema, conjunctival chemosis especially in the area of the transitional fold, the presence of hemorrhages under the conjunctiva, localized regardless of the location of the inlet, long-term preservation of the deep anterior chamber, indicating possible prolapse of the vitreous through the outlet. When deciding on the removal of foreign bodies from the eye, it is necessary to have data on the time the fragment remains in the eye, its nature, location, size, and associated complications in the tissues of the eye. The surgeon's tactics for new and old injuries vary depending on a number of reasons. In this regard, it is advisable to dwell on the peculiarities of the process during prolonged stay of chemically active foreign bodies in the eye. One of the complications of long-term presence of iron- and copper-containing foreign bodies in the eye is the development of siderosis and chalcosis of the eyeball. Siderosis of the eye.
Cornea - either the phenomena of local siderosis, expressed in brown pigmentation around the fragment, or impregnation of the corneal stroma with iron salts, their deposition on the endothelium of the cornea, which creates a brown opalescence of it.
Anterior chamber - moisture is usually opalescent due to the content of small iron particles in it. The iris has a darker, often brown color. In an advanced stage, mydriasis is observed, and in these cases the pupil does not always respond to convergence and accommodation. Angle of the anterior chamber - pigment deposits or exogenous and endogenous pigmentation of Schlemm's canal. Lens - in the initial stages of the process, deposits look like plaques, in later stages they look like pigment rings formed from many plaques. A brown ring is visible in the center of the pupil, in the cortical layers there is a ring of lighter color, disappearing towards the periphery, where the circle usually spreads and appears as individual dots. Vitreous body - severe destruction or opacities, as well as the formation of moorings. It should be noted that in many patients, changes in the vitreous body precede clinical manifestations of metallosis in the remaining membranes of the eye (Gundorova R.A., 1975). Retina - clinically detectable changes are characteristic of an advanced stage of siderosis. They are manifested clinically by the presence of pigmented foci in the fundus, very reminiscent of the so-called bone bodies in pigmentary retinal degeneration. Analysis of the factors influencing the development of siderosis showed that it is not possible to judge the relationship between the severity of the pathological process and the size of the foreign body; however, clinical experience shows that changes in the anterior section appear earlier after the injury when the fragment is located in the anterior chamber, lens, ciliary body, than when it is localized in the membranes of the posterior part of the eye. Chalcosis of the eyes.
The clinical picture of changes in the membranes and fluids of the eye during prolonged stay of a copper-containing foreign body in the eye in most patients is characterized by the phenomena of chalcosis.
Cornea - deposits in the epithelium and stroma of its smallest grains of blue, golden-blue and greenish color. The posterior surface of the cornea has a dull green color. Iris - different in color from the iris of the other eye, colored greenish or greenish-yellow. Gonioscopic examination of the anterior chamber angle reveals increased pigmentation of the corneoscleral trabeculae. The lens is the shape of a ring (disk) on the anterior capsule of the lens, corresponding to the width of the pupil, with radial strands of opacities extending from it, reminiscent of a sunflower figure - a constant sign of chalcosis. Vitreous body - clinically pronounced changes are in the nature of rough, dark-colored floating opacities associated with the accumulation of protein in them. Retina - Clinically significant retinal chalcosis is rare. The predominant localization of changes is the area of the macula, where the corolla is determined, consisting of individual foci of various sizes and shapes; their color varies from yellowish to copper-red. The lesions have a metallic sheen. Sometimes they are located around the central fossa in several rows. Clinical classification of metallosis of the eyeball (Gundorova R.A., Petropavlovskaya G.A. 1975): 1. Stage (latent period) - there are no clinical changes in the membranes of the eye, characteristic of siderosis and chalcosis, as well as changes in the retina, determined by electrophysiological research methods. 2. Stage - initial metallosis - mild initial changes in one (two) membranes without changes in functions and electrophysiological parameters. 3. Stage - advanced metallosis - pronounced degenerative changes in two (three) membranes of the eyeball, decreased visual acuity to 0.5-0.6, narrowing of the visual field by 10-40o. 4. Stage - advanced metallosis - gross, pronounced degenerative changes in all membranes and environments of the eyeball, visual acuity is reduced to light perception - 0.1; the field of view is narrowed to 10 or more or absent. The proposed classification allows us to correctly approach the development of indications for cataract extraction in patients with siderosis and chalcosis. At stages 1, 2 and 3 of the development of the process, cataract extraction surgery may be indicated. At an advanced stage, removal of the cloudy lens will most likely not give the desired effect, and therefore the operation is not advisable. For penetrating eye injuries, it is necessary to think about the introduction of a foreign body. Diagnosis of a foreign body in the eye consists of the following main stages: 1. Timely detection of a foreign body; 2. Establishing its character (magnetic, amagnetic); 3. Determination of fragment localization. To identify a foreign body, first of all, a thorough clinical examination of the patient is necessary using focal illumination, biomicroscopy, ophthalmoscopy, gonioscopy, cycloscopy, and ultrasound. X-ray techniques are of great importance in the diagnosis and localization of foreign bodies. X-ray diagnostics of foreign bodies in the eye consists of two stages: 1. Establishing the very fact of the presence of a foreign body in the eye or orbit, i.e. defining it; 2. If a foreign body is identified, establishing its exact location in the eye, i.e. its localization. To identify intraocular fragments, it is necessary to take survey photographs of the orbits in two mutually perpendicular projections: the anterior straight (nasomental) and the lateral. In cases where the shadow of a foreign body is visible only in one of the named projections, it is necessary to perform an additional x-ray examination of the orbit in the axial projection (Weinstein E.S., 1989). If a foreign body is detected on survey photographs of the orbit, localization begins using one of the x-ray techniques. If a foreign body is clearly visible on a direct projection image, it is localized using the Komberg-Baltin method. In cases where the foreign body is poorly visible or not visible at all on the image in the direct projection, but is detected in the axial and lateral projections, it should be localized using the Abalikhin-Pivovarov method. When examining each patient, conventional bone radiographs must be supplemented with survey non-skeletal photographs of the anterior segment of the eye, because Small and low-contrast fragments located in the anterior part of the eye can often be visible only on these images. Non-skeletal examinations should be carried out even in cases where the shadow of a foreign body is detected on ordinary photographs, because Besides this, there may be other, less radiopaque fragments in the eye. The most common is the method proposed by Vogt. The essence of the non-skeletal examination of the eye is to obtain an X-ray image of its anterior segment without superimposing bone tissue on it, as a result of which it is possible to obtain shadows of very small and low-contrast fragments. In the presence of multiple foreign bodies, the use of the Weinstein-Urmacher stereoradiogrammetric technique is indicated. In case of extensive wounds of the eye and prolapse of the membranes, its localization is possible without the introduction of a prosthesis - using bismuth gruel, Vodovozov points or a probe. One of the valuable methods for diagnosing foreign bodies in the eye is the ultrasound method. Complications of the wound process:
- Intraocular wound infection; — Traumatic cataract; — Post-traumatic changes in the vitreous body; — Post-traumatic corneal cataract; — Post-traumatic glaucoma; — Traumatic retinal detachment; - Sympathetic ophthalmia. — Traumatic hyphema and hemophthalmos — Post-traumatic subatrophy of the eyeball.
Help for the victim
In case of a penetrating injury to the eye, it is necessary to drip weak antibiotic drops into the eyes and carefully rinse the affected eye with a solution of Furatsioin or Rivanol, but avoid any rubbing.
The following drops can be antibacterial agents: Vigamox, Gentamicin, Albucid or Levomycetin.
If the wound is not too large, then you can additionally drip a solution of Novocaine or Lidocaine into the eye for pain relief. Although some experts recommend not to disturb the deformed organ, but to give an intramuscular injection of analgin or another drug with a similar effect. Afterwards, clean gauze is applied to the affected eye.
Upon arrival at the clinic, the patient undergoes an X-ray of the orbit to identify a foreign body. Emergency care for a penetrating eye injury involves immediate surgery. The procedure involves excision of damaged tissue. The doctor’s main goal in this case is to preserve as much viable tissue as possible.
After identifying the location of the foreign body, it is removed. If it is a metal body, then a magnet is used to remove it. Otherwise, the operation is performed using surgical instruments.
Sympathetic ophthalmia
Dependence of CO on the characteristics of injuries:
— Penetrating wounds, — Repeated operations or operations on the injured eye, — Localization in the anterior section, mainly in the corneoscleral zone, — Prolapse, entrapment of the uveal membranes, — Aseptic autoimmune post-traumatic uveitis, traumatic cataract, — Retinal detachment.
Dependence of SB on the timing of PSO:
- For patients, this is late PSO - from 2 days to 5 weeks;
— Insufficiently qualified wound treatment; — Frequent development of complications (traumatic cataracts, secondary glaucoma, retinal detachment and eye subatrophy with loss of all visual functions). Factors contributing to the development of sympathetic ophthalmia: 1. Violation of the hemato-ophthalmic barrier during penetrating trauma of the eyeball, complicated by prolapse and damage to the uveal membranes, migration of “beyond-barrier” uvearetinal antigens along the lymphatic pathways to the lymphoid organs and the development of autoimmune post-traumatic uveitis. 2. Violation of the immunoregulatory mechanisms of the immune system, the formation of cellular and humoral autoimmune reactions to uvearetinal antigens, retinal S-ag. 3. Various factors of the external and internal environment, including immunogenetic ones, influencing the state of the body’s immunity. When examining patients with OM (L.T. Arkhipova et al., 1976-1997), disorders of the immune status were revealed, characterized by: - A decrease in the number of T-lyphs, mainly against the background of a sluggish or recurrent process, after long-term treatment with steroids; — A decrease in the number of T-helpers and T-suppressors (CD4 and CD8) with an imbalance in the Tx/Tc immunoregulation index; — A decrease in the functional activity of T-lf (in the RBT test for the nonspecific mitogen PHA) more often in a chronic course; — Decrease in the concentration of IgG, A, M and dissymmunoglobulinemia. The immunosuppressive treatment system includes 3 components: 1. Enucleation of the blind sympathetic eye as the primary source of antigenic autosensitization of the body; 2. Immunosuppressive treatment with steroids and cytostatics that suppress the body’s immunopathological reactions; 3. Anti-relapse immunocorrective treatment for chronic forms of sympathetic inflammation. On the issue of enucleation of the sympathetic eye
Most literature sources and analysis of the Helmholtz Institute show that the prognosis of sympathetic ophthalmia improves when enucleation of the blind injured eye is performed in the early stages after the onset of the disease (from 1-2 days to 3-4 weeks). However, after studies conducted at the Helmholtz Institute in patients with a preserved sympathetic eye (with visual acuity in it from objective to 1.0), it turned out that they had a more favorable course and high visual acuity than in the group of patients whose eye was removed. This is believed to be due to the fact that in this group the injured eye had less severe inflammation. Marak GE (1979) showed that the prognosis of the disease is worse if the process in the injured eye spreads to the posterior part of the uvea and the retina. At the Helmholtz Research Institute, L.T. Arkhipova and others developed a treatment regimen for CO with steroids. They are prescribed locally from the first days of the disease (in instillations, under con-vu and parabulbar), given that in more than 80% of patients the inflammatory process spreads to the posterior part of the uvea and the retina. Principle of systemic treatment: 1. Average therapeutic doses - 25-60 mg (in terms of prednisolone) depending on age, clinical form and severity of the process. 2. Gradual reduction in dosage: first by 5 mg (1 tablet) of prednisolone every 5 days, and then starting from 30 mg to 2.5 mg (1/2 tablet), and from 15 mg to 1.25 mg (1/2 tablet). 4 tablets) every 5 days. 3. Steroid withdrawal occurs under the guise of non-steroidal anti-inflammatory drugs such as indomethacin. Those. when prednisolone is reduced to 10 mg, indomethacin 50 mg per day is additionally prescribed (2 tons x 2 times a day). In general, the course of treatment is 4-6 months, of which 1.5-2 months are steroids, and 2.5-3.5 months are indomethacin. In severe forms, treatment begins with intravenous injections of steroids at a rate of 1.0 in 10.0 saline solution No. 3-4, followed by a transition to tablet forms. For posterior forms of sympathetic ophthalmia and exudative chorioretinitis, pulse therapy is performed (IV drip in rheopolyglucin 16 mg every other day No. 3, then 8 mg No. 3 every other day, followed by switching to tablets with 60 mg.). Treatment with steroids is carried out against the background of giving potassium and calcium salts and an antidiabetic diet. The duration of local treatment is on average 8-10 months, total 5-6 months. Treatment is carried out under clinical and immunological control until reactions to uvearetinal tissue antigens are persistently suppressed.
Scleral injuries
The prognosis for an eye injury depends on the severity of the injury itself.
Injuries to the white membrane of the eye rarely occur independently. They are accompanied by loss and damage to the internal structures of the eyeball.
Treatment is exclusively surgical. In case of scleral injuries, all manipulations, starting from the initial examination, are carried out under general anesthesia.
The goals of therapy are inspection and assessment of the wound and wound channel, revision of internal structures and installation of them in a physiological place, removal of foreign bodies, restoration of the integrity of the sclera.
After the initial examination, the doctor decides on the extent of surgical intervention. All manipulations are carried out through the entrance hole in the sclera. For severe injuries, additional incisions may be required.
After restoration of the integrity of the membranes, the administration of general and local antibiotic therapy is indicated in order to prevent the development of purulent processes in the wound.
Frequency and timing of clinical observation
As a rule, they are set individually, depending on the nature of the injury and the severity of the post-traumatic process. The approximate frequency of observations of patients with various consequences of eye injury: - in case of damage to the protective apparatus of the eye appendages - 1-2 times a year for 3 years, with the exception of patients with lagophthalmos, who must be operated on in a timely manner and observed once a month to monitor the condition of the cornea. After 3 years of observation, patients can be removed from the register. - in case of damage to the cornea - repeated examinations are advisable during the first year - 4 times, since progression of the process and relapse are possible, less often in the second year - 2 times a year and in subsequent years - 1 time a year. Patients with cicatricial opacities of the cornea after 3 years of observation can be removed from the register. — if the lens is damaged, the frequency of observations depends on the type of cataract and the position of the lens. - for aphakia - control 4 times a year during the first year after surgery, then 2 times a year. - for pseudophakia - control once a month for 1 year after surgery, all subsequent years - 4 times a year. - for intraocular foreign bodies that are not indicated for removal, observation is carried out 2-4 times a year, and for amagnetic fragments in the transparent lens - once a month during the first year. After 3 years of observation, these patients can be removed from the register, except for patients with foreign bodies in the posterior part of the eye. - if the vitreous body is damaged, it is advisable to carry out examinations 4 times a year during the first 2 years, in the next year - 2 times and subsequently may be removed from the register. — in case of secondary glaucoma, the frequency of examinations depends on the compensation of the process, but even with full compensation, patients should be examined 2-4 times a year.
Specialized care from ophthalmologists
Specialized care from ophthalmologists is provided immediately to the patient at any time of the day or night in an eye trauma center, which is located in any city. The list of specialized ophthalmological care services includes additional diagnostics and X-ray localization, removal of intraocular foreign bodies, and primary surgical treatment of wounds.
After the diagnosis is officially confirmed, the doctor conducts a survey X-ray of the orbits in several projections - lateral and anteroposterior.
To do this, it is important to position the patient correctly. During anteroposterior x-ray of the orbit, the patient lies face down so as to touch the table with the end of the nose and lips. With this positioning of the head, the shadow of the pyramidal bone is removed from the projection of the orbit. In a lateral view, the patient turns his head over so that there is access to the affected eye.
If survey radiographs show a shadow of a foreign body in the orbital area of the diseased eye, then it is important to carry out X-ray localization of the foreign body in order to identify its location. It is on this factor that the doctor’s further actions when providing care to the patient will depend.
If the foreign body is located in the tissue of the orbit and it is not large, then it does not need to be removed. Chemical removal is carried out only for large bodies that lead to the appearance of pain in the orbit.
Intraocular foreign bodies are removed immediately. If a foreign body remains inside the eyeball for too long, this may result in some difficulties in its removal due to overgrowth of connective tissue. In the tissues of the eye, the foreign body quickly oxidizes, and the oxidation products negatively affect the delicate structures of the organ. At the same time, the presence of a foreign object can lead to the spread of a purulent infection, which will require additional treatment.