Adrenal CT is an x-ray study that allows you to scan the kidneys, adrenal glands, and abdominal organs. The study can be carried out as a comprehensive or only as a tomographic study of the adrenal glands. Before diagnosis, patients are examined by a urologist, gynecologist, oncologist, or therapist. The reason for referral for an examination of the adrenal glands is a hormonal imbalance, which manifests itself in the form of weight gain or sudden weight loss; in women, male-pattern hair appears on the body, problems with kidney function, sexual function is impaired, and infertility may develop.
At the Yusupov Hospital, diagnostic studies are carried out using modern methods using innovative equipment. Computed tomography of the adrenal glands with contrast can detect adrenal cancer, determine the extent of damage to the organ, and the presence of tumor metastases. If an adrenal tumor is highly aggressive, in a short period it leads to the development of severe complications in the vascular system of the kidneys, heart, and brain. Adrenal cancer is preceded by various endocrine disorders. The Yusupov Hospital treats various diseases of the kidneys and adrenal glands, including malignant and benign tumors.
The adrenal glands are endocrine glands that are responsible for the balance and production of hormones in the human body. The adrenal glands influence metabolism, control puberty, influence the body's resistance to infections, anti-allergenic abilities, produce the hormone adrenaline, which provides invaluable assistance during stress, norepinephrine, affect the sexual function of men and women, participate in the production of cortisol, which supports the body during prolonged stress.
CT scan of the adrenal glands with contrast: price in Moscow
You can get a CT scan of the adrenal glands in Moscow in various clinics and medical centers. CT scan of the adrenal glands can be comprehensive, covering the area of the kidneys and other abdominal organs for examination. CT scan of the adrenal glands can be prescribed as an independent study if adrenal gland pathology is suspected. Computed tomography is performed with or without contrast. The patient should be aware that when performing a CT scan of the adrenal glands with contrast, the price is higher than without contrast.
The price of an adrenal CT scan depends on a number of factors: the location and reputation of the medical center, how modern equipment the clinic uses to diagnose diseases, whether contrast is used or not. CT scan of the adrenal glands price in Moscow from 3,000 rubles and above (without contrast), with contrast from 7,000 rubles and above; at a low price, computed tomography can be done as a promotion, at night in some clinics.
CT scan of the adrenal glands with contrast: indications
Indications for diagnosing adrenal pathologies using contrast-enhanced CT are the following disorders:
- Pale or reddened skin.
- A persistent increase in blood pressure that is difficult to treat with hypertension medications.
- Decreased potency, lack of sexual desire.
- Menstrual irregularities.
- Depression, increased aggressiveness.
- Joint pain, numbness of limbs, cramps.
- Gastrointestinal diseases.
- Dramatic weight loss.
- Sudden weight gain.
- Women have male pattern hair.
- Hirsutism.
- General malaise, headache.
- Increased blood sugar.
Contrasting allows you to clearly identify the boundaries of an organ, determine its size, and defects in the tissues of the organ. Using contrast-enhanced CT, the density of adrenal tissue, disruption of the structure of the organ, the presence of tumor formations, changes in the size of the organ, and vascular pathology are determined. CT scans can detect the following adrenal gland diseases:
- Adenoma.
- Carcinoma.
- Hemangioma.
- Fibroma.
- Paraganglioma.
- Pheochromocytoma.
- Mixed tumors of the adrenal medulla and cortex.
- Metastases of malignant tumors.
- Injury.
- Vascular insufficiency.
- Pathology of lymph nodes.
CT scanning of the adrenal glands is performed before surgery, for dynamic monitoring during treatment, as a postoperative examination method.
CT scan of the adrenal glands with contrast: contraindications
Computed tomography with contrast is not performed:
- Patients with impaired renal function.
- For severe heart diseases.
- Liver failure.
- If you are allergic to contrast agents.
- For diabetes mellitus.
- In severe condition of the patient (coma).
- If the patient's body weight is over 200 kg.
- During pregnancy and lactation. During lactation, CT scanning is possible with a temporary cessation of feeding the child.
- Thyroid diseases.
- In childhood, there are a number of restrictions - CT is not performed before 4 years of age, after 4 and up to 14 years of age it is performed if diagnosis using CT is vital.
Equipment
Examinations of the adrenal glands in newborns and young children are carried out using high-frequency broadband sensors (up to 10 MHz) and a scanner equipped with a sensitive color or power Doppler option (diagnosis of neuroblastoma tumors).
In adolescents and adults, adrenal examinations are performed using 2–5 MHz convex broadband probes, which are used in abdominal scans. In thinner patients, higher frequency transducers may be used. Preparation for the examination is the same as for an abdominal scan.
In many cases, DTHI and SCI improve the contrast between the adrenal tumor and adjacent tissues and allow better visualization of tumor margins (Figures 1 and 2).
Harmonic imaging in particular provides better visualization (better contrast) of even normal adrenal glands, allowing them to be measured.
Three-dimensional scanning allows a more thorough assessment of tumor size and improves correlation with computed tomography (Fig. 3). In complex cases, 3D ultrasound allows for easier and more thorough interpretation of complex anatomical relationships. Three-dimensional imaging may be particularly useful for visualizing tumors in the left adrenal gland, as it is more difficult to visualize due to its anatomical conditions.
Figure 1 : Pheochromocytoma of the left adrenal gland (arrow).
A. _ Conventional ultrasound in B- mode B. B-mode with tissue harmonics. Compared to image A, there are fewer artifacts - clearer tumor boundaries.
Figure 2 : Pheochromocytoma of the right adrenal gland (arrow).
A. _ Conventional ultrasound in B- mode B. B-mode with SCI. Compared to image A, less artifacts, smoother image, clearer tumor edges.
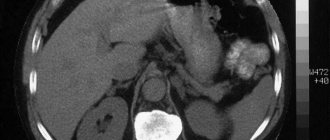
Figure 3 : Small adenoma of the left adrenal gland
– A. P – pancreas, K – upper pole of the kidney, S – spleen. Three-dimensional ultrasound - axial image (A). This small tumor of the left adrenal gland was not detected on real-time 2D imaging. 3D ultrasound allows visualization of the lesion and comparison of its size with CT (B ).
B-mode ultrasound imaging is useful in differentiating between cysts and solid tumors of the adrenal gland. This information is especially important if the diagnosis of adrenal adenoma in computed tomography was made only on the basis of its low density without the administration of iodinated contrast agent.
Regarding ultrasound imaging, if a hypoechoic lesion does not present all the features of a simple cyst on B-mode examination, shear wave elastography can be used. This allows differentiation between solid and cystic lesions.
Fabric elasticity results are presented on an absolute scale in kPa. Fabric elasticity is represented in real time as a color map placed on the B-mode image. Unlike solid tumors, cysts do not present a color elastographic signal because shear waves do not propagate through fluids (Figure 4).
Figure 4 : Recurrent lymphatic cyst of the right adrenal gland, maximum size 10 cm: shear wave elastography - top image, B-mode - bottom image. An artifact-like color signal is visible within the lesion at its periphery, indicating low stiffness values (approximately 4 kPa)
Ultrasound studies with contrast did not reveal any features that would allow a definite differentiation between benign and malignant adrenal tumors.
An assessment of the nature of vascularization in the group of benign adrenal lesions showed that there are differences between nodular hyperplasia and adenomas. With nodular hyperplasia, vascularization begins at the periphery of the lesion. Adenomas, however, usually have a mixed or central vascularization pattern (Figs. 5 and 6).
Figure 5 : Nodular adrenal hyperplasia with two tumors, with a mean diameter of 23 mm and 10 mm. B-mode image (right). Parametric contrast inflow time (SonoVue) image (left) shows vascularization of both tumors starting from the periphery.
Figure 6 : Adrenal cortical adenoma (arrows) with a mean diameter of 16 mm. B-mode image (right). Parametric contrast agent arrival time (SonoVue) image (left) shows tumor vascularization starting from the center and periphery simultaneously.
Computed tomography of the adrenal glands: CT scan
Before undergoing a CT scan of the adrenal glands, patients undergo preparation. Five days before the CT scan, you should follow a diet, exclude gas-forming foods, fatty, spicy, salty foods, coffee, strong tea, and alcohol. The patient is being tested for allergies to a contrast agent. Computed tomography is performed on an empty stomach - you should not eat or drink 7-8 hours before diagnosis. Before diagnosis, you should remove jewelry and do not wear clothes with metal buttons or decorations.
Computed tomography is performed within 5-30 minutes. The patient is placed on the movable table of the tomograph, the table is installed under the scanning ring of the tomograph. The doctor is in the next room, observing the patient and giving commands. After the scan is completed, the patient is given recommendations, and the radiologist interprets the scan results. Computed tomography allows you to obtain layer-by-layer images with high resolution; from the images, the doctor determines the location and relationship of organs in relation to each other, the boundaries of the organ, and the presence of the smallest pathological areas.
Despite the fact that CT is considered a safe diagnostic method, the method has radiation exposure. Before prescribing a study, the doctor calculates the radiation exposure; if the patient has already been diagnosed using CT, MRI, or X-ray within one year, the patient is offered other research methods. At the Yusupov Hospital, patients will be able to undergo examinations of tissues and organs using computed tomography and other diagnostic methods. The hospital performs MSCT - multislice computed tomography, computed tomography, computed tomography with contrast. The hospital consists of several multidisciplinary clinics, a diagnostic center, a laboratory, and a rehabilitation center.
The clinical departments of the hospital receive specialists of the highest category, doctors of science, and you can get advice from a specialist from a partner clinic abroad. A CT scan with contrast is prescribed by a doctor after examining the patient. You can make an appointment with a doctor by phone.
Sonography results for adrenal pathology
Sonography results for adrenal pathology
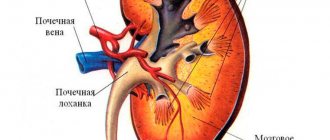
Echography of the adrenal glands is normal
The adrenal glands are thin structures located in the thickness of the retroperitoneal tissue, in the duplicator of the renal fascia, in cross section having the shape of an inverted letter “Y” or “V”. The question of the echographic size and structure of normal adrenal glands is very complex, since the very possibility of echographic visualization of normal adrenal glands in the adult population is currently being questioned, although the literature on this issue is quite contradictory. The results of examinations are undoubtedly influenced by such determining factors as the experience of the doctor and the quality of the ultrasound equipment used. It should immediately be noted that during the examination, the right adrenal gland is visualized better than the left.
The echographic dimensions of normal adrenal glands are: length on the right 1.8-2.8 cm, length on the left 1.6-2.5 cm, thickness 1.1-1.6 cm.
The most common approaches for visualizing the localization zone of the adrenal glands are: on the right - subcostal (in this case, the acoustic 'window' is the right lobe of the liver and the inferior vena cava), on the left - intercostal along the left axillary line. The gas bubble of the stomach interferes with the visualization of the left adrenal gland; there is no good “acoustic window” on this side, and therefore adrenal pathology is often not diagnosed on the left side.
Normal adrenal glands can only be detected through long-term studies using high-resolution equipment. The adrenal glands are easier to visualize when they are enlarged.
Right adrenal gland: scanning in the high lateral transverse or oblique plane identifies the superior pole of the kidney and the inferior vena cava (the adrenal gland should be located between them), a scan in the upper longitudinal plane of the abdominal cavity along the midclavicular line or anterior axillary line allows visualization of the vena cava.
Rice. 1. Visualization of the right adrenal gland in longitudinal section: the slice plane passes through the liver and vena cava (Vc), followed by the adrenal gland (^^). Ard - right renal artery.
Landmarks for determining the location of the right adrenal gland are the upper pole of the right kidney, the right lobe of the liver laterally. right leg of the diaphragm medially, inferior vena cava medially;
Rice. 2. Cross-sectional view of the right adrenal gland showing the origin of the renal vein (Vrd) as well as a small section of the upper pole of the kidney (N). The adrenal gland is well visualized (^);
Visualization of the left adrenal gland is much more difficult. In front, the upper pole of the left kidney is covered by the stomach and intestines.
Rice. 3. Visualization of the left adrenal gland in a lateral longitudinal section: a hypoechoic section of the adrenal gland is visible (^).
Left adrenal gland: identified by scanning in a high lateral plane passing through the lower pole of the spleen and the upper pole of the kidney; the sensor is tilted medially, towards the aorta. As on the right, the gland can be found in the high upper transverse plane of the abdominal cavity, between the upper pole of the kidney and the aorta.
Rice. 4. Left adrenal gland (^) in lateral cross-section. Mi - spleen (additional finding: non-Hodgkin's lymphoma), N - ventricle, A - aorta.
In adults, the adrenal glands are not visible or sometimes faintly visible in the perinephric tissue. Ultrasound examination of the adrenal glands cannot be clearly assessed.
The doctor performing an ultrasound examination of the adrenal glands should pay attention to the following points:
- the general picture of unchanged adrenal glands cannot be unequivocally assessed;
- Hyperplasia and small adenomas of the adrenal glands are quite poorly distinguishable;
- identified hormonally active changes in the adrenal glands must be confirmed by CT, MRI and other specific diagnostic methods;
- The main task of ultrasound examination is to search and detect hormonally inactive asymptomatic tumors.
Ultrasound is not a perfect method for visualizing the adrenal glands.
The main objective of the examination is to detect hormonally inactive asymptomatic tumors.
Adrenal tumors
Signs of adrenal tumors
Based on organ specificity, tumors are distinguished: organ-specific and non-organ-specific. Organ-specific - adrenocortical tumors (tumors from various cells of the adrenal cortex), adrenomedullary tumors (mainly pheochromocytomas and pheochromoblastomas - tumors arising from chromaffin cells of the medulla). Hormone-producing adrenal tumors, such as the adenoma in Conn's syndrome or the hyperplasia in Cushing's syndrome, are usually too small to be detected by sonography. Only clinically significant pheochromocytoma, usually already several centimeters in diameter, can be detected sonographically in 90% of cases.
Fig.5. Adrenal cancer. Large heterogeneous tumor (>^v) above the right kidney. Based on ultrasound data alone, a differential diagnosis of adrenal metastasis cannot be made.
Non-organ-specific tumors: metastatic tumors from other organs, lymphomas. rare tumors (vascular tumors, tumors from adipose tissue, nerve fibers, etc.). Hematogenous spread of metastases is due to strong vascularization of the adrenal glands and can occur in bronchogenic cancer, as well as in breast and kidney cancer. Metastases are usually seen as hypoechoic lesions between the upper pole of the kidney and the spleen or inferior surface of the liver, respectively, and should be differentiated from atypical renal cysts.
Based on the degree of malignancy, benign tumors (adenomas) and malignant tumors (carcinomas) are distinguished.
Based on the presence of hormonal activity, a distinction is made between hormonally active tumors (both benign and malignant) and hormonally inactive adrenal tumors.
In general, clinical manifestations of adrenal tumors are: drowsiness, electrolyte disturbances, hormonal disturbances; pain in the upper abdomen due to the “mass effect” (the effect of squeezing surrounding tissues); swelling as a result of vena cava compression syndrome.
It is not possible to determine the presence and specificity of hormonal activity from the echographic picture of the tumor. Rather, on the contrary, the presence of clinical manifestations of a hormonally active adrenal tumor is an indication for an echographic examination. Hormonally active tumors of the adrenal cortex include androsteromas, aldosteromas, and corticosteromas.
When diagnosing adrenal tumors, the following are used:
· History, clinical picture.
· Laboratory tests (up to 20% of adrenal tumors are non-secreting): electrolyte composition of the blood; if necessary, the daily cortisol level is determined; level of androgens, aldosterone, test with suppression of secretion.
· Ultrasound examination and ultrasound-guided percutaneous aspiration.
· If necessary, CT examination.
Androsteromas and stromas are tumors of the zona reticularis of the adrenal cortex, producing large amounts of androgens and estrogens, as well as cortisol and mineralocorticoids. These tumors manifest themselves clinically as symptoms of virilization, arterial hypertension, and signs of Cushing's syndrome. Similar clinical symptoms occur with tumors of the gonads and with congenital virilizing adrenal hyperplasia. Estrogen-secreting tumors are characterized by high levels of estrogen, as well as decreased concentrations of gonadotropin. The leading signs in the clinic are signs of feminization.
Aldosteromas are tumors of the zona glomerulosa of the adrenal cortex, accompanied by hyperproduction of aldosterone. Clinical symptoms of aldosteronism (Conn syndrome) are associated with electrolyte disturbances in the form of excessive excretion of potassium ions and retention of sodium and chloride ions in the body and are manifested primarily by damage to the cardiovascular system and kidneys. A similar clinical picture occurs with hyperplasia of the zona glomerulosa of the adrenal cortex.
Corticosteromas are tumors of the zona fasciculata of the adrenal cortex that produce excessive amounts of glucocorticoids, resulting in the development of Cushingoid syndrome. Similar clinical symptoms are observed with damage to the hypothalamus or pituitary gland (Cushing's disease) with overproduction of ACTH and bilateral adrenal hyperplasia, as well as with adenocarcinomas of the lungs, pancreas, ovaries and uterus, producing an ACTH-like substance that increases adrenal function.
Fig.6. ad Perirenal formation, a Perinephric fat (F). Arrows: Gerota's fascia surrounding the perirenal fat capsule, K - kidney, b Adenoma of the right adrenal gland (arrow), discovered by chance as a formation with a complex structure. Differential diagnosis: pheochromocytoma, metastases, primary carcinoma. Hormonal tests were negative, with metastasis of bronchial carcinoma to the adrenal gland (cursors), located between the upper pole of the kidney (K) and the vena cava (VC). d Perinephric fluid collection communicating with the kidney at the pericapsular level. Differential diagnosis: abscess, hematoma, urinoma.
Adrenal tumors are characterized by the following ultrasound findings: Hypoechoic formation, defined on the right between the vena cava and the upper pole of the kidney (where it can easily cause vena cava compression syndrome) or on the left, between the aorta and the upper pole of the kidney
A hormonally active tumor of the medullary substance (chromaffin cells) of the adrenal glands is pheochromocytoma or pheochromoblastoma. The leading clinical symptom is hypertension (permanent form with crises or paroxysmal form). Similar crises are observed in various forms of hypertension, kidney disease, and diencephalic syndrome. However, it is possible to achieve relief of a crisis in the presence of pheochromocytoma only by introducing agents that block the action of catecholamines. An increase in the level of catecholamines and catecholamine metabolic products in urine tests done after a crisis is also characteristic.
Fig.7. a-c Adrenal tumor, a Heterogeneous hypoechoic formation (P), presumably in the liver (L), suspicious for a liver tumor, b Hypoechoic formation (cursors) near the upper pole of the right kidney in the same patient, c On the lateral plane it is determined a large hypoechoic adrenal tumor (AT) located medial to the anterior aspect of the upper pole of the left kidney (K). Diagnosis: pheochromocytoma. S - spleen.
Echographically, pheochromocytoma is represented by a formation of increased echogenicity, sometimes with anechoic areas corresponding to areas of decay or hemorrhage. It must also be remembered that pheochromocytoma can also have an extra-adrenal localization (paracaval sympathetic ganglia, sympathetic ganglia of the mediastinum, ganglia in the wall of the bladder).
Rice. 8. Pheochromocytoma on the right (^). A tumor with cystic structures (^^) is adjacent to the right kidney.
Accuracy of ultrasound diagnosis: adrenal carcinomas rarely measure less than 3 cm, the usual size of adenomas is less than 6 cm. An adrenal tumor, the size of which does not exceed 2-3 cm, can easily be detected with a targeted ultrasound examination. Differential diagnosis of benign and malignant neoplasms is carried out by percutaneous biopsy performed under ultrasound control. Before performing a fine-needle biopsy, pheochromocytoma should be excluded to avoid a hypertensive crisis.
Fig.9. TIAB. a In the area of the right adrenal gland, a hypoechoic formation (TU) of elliptical shape is detected. L — liver, b The formation is visualized, the course of the needle is marked, the depth of its insertion is determined (truncated arrow), c The location of the echo signal of the needle tip in the pathological focus is confirmed (arrow
The liquid aspirate is subjected to cytological and bacteriological analysis.
Sample preparation:
Material (mixed with citrate) is removed onto a glass slide
· Larger particles are placed in an Eppendorf tube filled with formaldehyde.
· The material for cytological examination is distributed onto a glass slide and dried in air.
Sonography is more important for identifying metastases in the adrenal glands.
Metastatic tumors of the adrenal glands. The most common sources of metastasis are: lungs, mammary and thyroid glands, colon, pancreas, esophagus. Damage to the adrenal glands is often observed in melanoma and lymphoma. The lesion is usually bilateral. Metastases with clear, even contours and a round shape are more common.
Fig. 10. Metastasis to the adrenal gland.
Despite the malignancy of the process, the contour of the tumor is smooth and clear, the internal echostructure is relatively homogeneous. There are usually no correlations between the echogenicity and echostructure of the primary lesion and adrenal metastasis. The only tumor that gives metastases and has echo-structural changes similar to the primary focus is lymphoma - pseudo-cystic anechoic structures with a capsule and distal pseudo-enhancement are identified in the affected adrenal glands. The differential diagnosis can be facilitated by identifying involvement of the retroperitoneal lymph nodes, which is almost always present at this stage of the disease.
Whether a mass in the adrenal gland is malignant or not cannot be decided based on its echogenicity. Adrenal tumors must be differentiated from: adrenal hyperplasias; inflammatory changes in the adrenal glands (tuberculosis, syphilitic origin, with toxoplasmosis, disseminated histoplasmosis, granulomatosis); adrenal hematomas (often develop during the perinatal period as a result of perinatal hypoxia, and in adulthood as a result of sepsis, anticoagulant therapy, during pregnancy, and with severe traumatic manifestations);
Rice. 11. Cyst of the left adrenal gland (^). Compression of the upper pole of the kidney by a cyst.
adrenal cysts with the presence of an internal structure (a suppurating cyst, a cyst with elements of hemorrhage, a cyst with fluid containing a large amount of protein); necrosis of the adrenal gland, which developed as a result of thrombosis of the adrenal vein during meningococcal, streptococcal, gonococcal infections in children, or as a result of iatrogenic thrombosis of the adrenal vein during adrenal venography.
Thus, despite its accessibility and ease of implementation, the ultrasound method is not the most informative method for diagnosing adrenal pathology. If there are clinical and laboratory manifestations of adrenal disease (primarily tumors), after receiving negative echography results, it is necessary to conduct a CT or MRI, in which a more accurate diagnosis is possible, in particular, determining the nature of the process (benign and malignant). Currently, selective angiography and venography are becoming less important. For topical diagnosis of extra organ tumors, radioisotope scanning with iodine isotopes is successfully used. Fine-needle aspiration biopsy, despite the high sensitivity and specificity of the method, is not performed in the presence of hormonally active formations - due to the risk of developing a crisis.