Chronic adrenal insufficiency is a disease that occurs when the production of hormones by the adrenal cortex decreases.
Highlight:
- primary adrenal insufficiency (Addison's disease). The disease is caused by damage to the adrenal cortex, which does not produce enough hormones;
- secondary adrenal insufficiency, when hormone production decreases due to a decrease in the amount of ACTH, a hormone produced in the pituitary gland and regulating the activity of the adrenal cortex.
Causes
The cause of primary adrenal insufficiency (Addison's disease) often remains unknown (in 50-60% of cases).
The disease can also occur due to damage to the adrenal glands when:
- tuberculosis;
- autoimmune diseases (the immune system begins to damage healthy cells of its own body);
- hemochromatosis, scleroderma;
- blastomycosis;
- syphilis, brucellosis;
- metastasis of a malignant tumor (cancer of the lungs, mammary glands and other organs);
- adrenalectomy (removal of the adrenal glands) due to tumors, Itsenko-Cushing's disease;
- treatment with cytostatics;
- long-term glucocorticoid therapy. In this case, suppression of the function of the adrenal cortex occurs as a withdrawal syndrome;
- AIDS. Adrenal necrosis may occur.
Secondary adrenal insufficiency develops with diseases of the pituitary gland (most often with hypopituitarism).
What's happening?
As a result of a decrease in the amount of hormones of the adrenal cortex, metabolism and the balance of water and salts in the body are disrupted.
The disease is characterized by:
- progressive general and muscle weakness, increasing fatigue;
- weight loss;
- darkening of the skin, reminiscent of a strong tan. First of all, darkening of the skin appears in open areas of the skin (face, neck, hands), in places of friction of the skin and skin folds (elbows, palmar lines, abdomen, etc.), places of natural pigmentation (nipples of the mammary glands, scrotum, anus) , in places of contact and friction of skin and clothing (at the point of pressure from the elastic band of panties, a belt, a belt), in the area of postoperative scars. Sometimes, against the background of darkening of the skin, there are white spots - vitiligo. Brown spots may also appear on the mucous membrane of the cheeks, lips, gums, and tongue.
- decreased or loss of appetite;
- decreased blood pressure;
- dizziness, fainting;
- disorders of the gastrointestinal tract: nausea, vomiting, alternating diarrhea and constipation;
- stomach ache;
- craving for salty foods;
- apathy, irritability, deterioration of concentration, attention, memory.
With secondary adrenal insufficiency, the skin color of patients does not change.
Adrenal insufficiency (hypocortisolism)
Adrenal insufficiency
(adrenal insufficiency, hypocortisolism) is a clinical syndrome caused by insufficient secretion of hormones from the adrenal cortex as a result of disruption of the functioning of one or more parts of the hypothalamic-pituitary-adrenal system. Adrenal insufficiency is divided into primary, resulting from the destruction of the adrenal cortex itself, and secondary (hypothalamic-pituitary), resulting from insufficient ACTH secretion by the adenohypophysis. In clinical practice, primary chronic adrenal insufficiency is the most common (95% of cases). The disease, caused by a destructive process in the adrenal glands, was first described in 1855 by the English physician Thomas Addison (1793-1860). Primary hypocortisolism of autoimmune and tuberculous etiology is referred to as Addison's disease.
The main causes of primary chronic adrenal insufficiency are:
- Autoimmune destruction of the adrenal cortex (98% of cases). Antibodies to the enzyme 21-hydroxylase (P450c21) are detected in the blood of most patients. In addition, 60-70% of patients develop other autoimmune diseases, most often autoimmune thyroiditis.
- Adrenal tuberculosis (1-2%). Most patients suffer from tuberculosis of the lungs.
- Adrenoleukodystrophy (1-2%) is an X-linked recessive disease in which a defect in the enzyme systems that metabolize long-chain fatty acids is inherited, resulting in their accumulation in the white matter of the central nervous system and the adrenal cortex, leading to dystrophic changes.
- Rare causes (coagulopathies, bilateral hemorrhagic adrenal infarction (Waterhouse-Friderichsen syndrome), tumor metastases, bilateral adrenalectomy, HIV-associated complex. The main causes of secondary hypocortisolism are various tumor and destructive processes in the hypothalamic-pituitary region. Acute adrenal insufficiency
(Addisonian crisis), in the vast majority of cases, has the same causes as the chronic crisis and represents its decompensation.
With primary hypocortisolism, as a result of the destruction of more than 90% of the cortex of both adrenal glands, a deficiency of aldosterone and cortisol is formed. Aldosterone deficiency leads to sodium loss, potassium retention (hyperkalemia) and progressive dehydration. The consequence of water and electrolyte disorders are changes in the cardiovascular and digestive systems. Cortisol deficiency leads to a decrease in the body's adaptive capabilities, a decrease in the processes of gluconeogenesis and glycogen synthesis. In this regard, primary chronic adrenal insufficiency manifests against the background of various physiological stresses (infections, injuries, decompensation of concomitant pathologies). Cortisol deficiency via a negative feedback mechanism leads to increased production of ACTH and its precursor proopiomelanocortin. As a result of proteolysis of proopiomelanocortin, in addition to ACTH, melanocyte-stimulating hormone is also formed. Thus, with primary hypocortisolism, in parallel with excess ACTH, an excess of melanocyte-stimulating hormone is formed, which causes the most striking symptom of primary chronic adrenal insufficiency - hyperpigmentation of the skin and mucous membranes.
Due to the fact that the production of aldosterone by the adrenal cortex occurs almost independently of the effects of ACTH,
with
secondary hypocortisolism,
due to a lack of ACTH, a deficiency of cortisol alone develops, and the production of aldosterone remains. This is what determines the fact that secondary hypocorticism has a relatively milder course compared to primary.
Clinical manifestations
The main clinical symptoms of primary hypocortisolism (Addison's disease) are:
- Hyperpigmentation of the skin and mucous membranes.
The severity of hyperpigmentation corresponds to the severity and duration of the process.
First, the exposed parts of the body that are most exposed to the sun darken - the face, neck, hands, as well as places that are normally more heavily pigmented (nipples, scrotum, external genitalia). Hyperpigmentation of friction sites and visible mucous membranes is of great diagnostic value. Characterized by hyperpigmentation of the palmar lines, which stand out against the relatively light background of the surrounding tissue, darkening of friction points with clothing, collar, and belt. Skin tone can vary from smoky, bronze (bronze disease) , tan, dirty skin, up to severe diffuse hyperpigmentation. Hyperpigmentation of the mucous membranes of the lips, gums, cheeks, soft and hard palate is quite specific, but not always pronounced. The absence of melasma is a fairly serious argument against the diagnosis of primary chronic adrenal insufficiency; however, there are cases of so-called “white Addisonism”,
when hyperpigmentation is almost absent.
Against the background of hyperpigmentation, patients often develop non-pigmented spots (vitiligo).
Their size ranges from small, barely noticeable, to large, with irregular contours, clearly standing out against the general dark background. Vitiligo is characteristic exclusively of primary chronic adrenal insufficiency of autoimmune origin. - Losing weight.
Its severity ranges from moderate (3-6 kg) to significant (15-25 kg), especially with initially excess body weight.
- General weakness, asthenia, depression, decreased libido.
General weakness progresses from mild to complete loss of performance. Patients are depressed, lethargic, unemotional, irritable, and half of them are diagnosed with depressive disorders.
- Arterial hypotension
at first it may only have an orthostatic character; Patients often report fainting conditions that are triggered by various stresses. The discovery of arterial hypertension in a patient is a strong argument against the diagnosis of adrenal insufficiency, although if primary chronic adrenal insufficiency developed against the background of previous hypertension, blood pressure may be normal.
- Dyspeptic disorders.
The most common symptoms are poor appetite and diffuse epigastric pain, alternating diarrhea and constipation. With severe decompensation of the disease, nausea, vomiting, and anorexia appear.
- Addiction to salty foods
associated with progressive sodium loss. In some cases, it goes as far as consuming salt in its pure form.
- Hypoglycemia
It practically does not occur in the form of typical attacks, but can be detected during laboratory testing.
Clinical picture of secondary hypocortisolism
distinguished by the absence of hyperpigmentation and symptoms associated with aldosterone deficiency (arterial hypotension, addiction to salty foods, dyspepsia). What comes to the fore are non-specific symptoms such as general weakness and attacks of hypoglycemia, which are described as episodes of feeling unwell a few hours after eating.
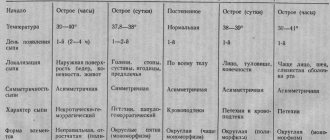
Clinical picture of acute adrenal insufficiency
(Addisonian crisis) is represented by a complex of symptoms, based on the predominance of which three clinical forms can be distinguished:
- Cardiovascular form.
In this variant, the phenomena of acute circulatory failure are dominant: pallor of the face with acrocyanosis, coldness of the extremities, severe arterial hypotension, tachycardia, threadlike pulse, anuria, collapse.
- Gastrointestinal form.
The symptoms may resemble a food toxic infection or even an acute abdominal condition. Spastic abdominal pain, nausea, uncontrollable vomiting, loose stools, and flatulence predominate.
- Neuropsychic form.
Headache, meningeal symptoms, convulsions, focal symptoms, delirium, lethargy, and stupor predominate.
Diagnostics
Primary hypocortisolism
- Laboratory confirmation of hypocortisolism.
Primary chronic adrenal insufficiency is characterized by hyperkalemia, hyponatremia, leukopenia, lymphoitosis, decreased levels of cortisol and aldosterone, high levels of ACTH and renin.
- Etiological diagnosis.
A marker of chronic adrenal insufficiency of autoimmune origin is antibodies to P450c21.
- Specific changes detected by MRI of the brain and spinal cord.
- In chronic adrenal insufficiency of tuberculous origin, changes in the lungs are almost always detected.
Diagnosis and treatment
To identify chronic adrenal insufficiency, the following is prescribed:
- clinical blood test: anemia is detected, an increase in the number of eosinophils in the blood;
- biochemical blood test: increased potassium and creatinine levels, decreased sodium, hypoglycemia (low blood sugar);
- study of the level of adrenal hormones in the blood and urine: a decrease in the amount of corticosteroids (cortisol, aldosterone, etc.) is detected;
- special tests - water load test, Thorne test, glycemic curve, etc.;
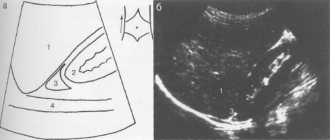
- computed tomography allows you to assess the size of the adrenal glands; diagnose the tubercular process, calcifications, adrenal tumors;
- Ultrasound of the adrenal glands and kidneys;
- various methods for determining adrenal autoantibodies - for the diagnosis of autoimmune Addison's disease.
Treatment is aimed, on the one hand, at eliminating the process that caused damage to the adrenal glands and, on the other, at replacing the lack of hormones.
Recommendations:
- The diet for chronic adrenal insufficiency should contain an increased amount of calories, proteins, vitamins, and table salt (3-10 g/day).
- It is necessary to avoid serious physical and mental stress, not to drink alcohol and sleeping pills.
- If tuberculosis is suspected, courses of anti-tuberculosis drugs are prescribed under the supervision of a phthisiatrician.
- Replacement therapy is mandatory - constant lifelong administration of synthetic hormones of the adrenal cortex (for example, cortisol). If acute infectious diseases or surgery develop, it is necessary to consult an endocrinologist to adjust the dose of hormones taken.
- Independently reducing the dose of hormones or canceling them is unacceptable, since they lead to the development of a severe complication of the disease - acute adrenal insufficiency.
The course of the disease with early diagnosis and proper treatment is favorable. In women suffering from chronic adrenal insufficiency, pregnancy and normal childbirth are possible.
Treatment
Treatment is aimed, on the one hand, at eliminating the process that caused damage to the adrenal glands and, on the other, at replacing the lack of hormones.
The diet for chronic adrenal insufficiency should contain an increased amount of calories, proteins, vitamins, and table salt.
- It is necessary to avoid serious physical and mental stress, not to drink alcohol and sleeping pills.
- If tuberculosis is suspected, courses of anti-tuberculosis drugs are prescribed under the supervision of a phthisiatrician.
- Replacement therapy is mandatory - constant lifelong administration of synthetic hormones of the adrenal cortex (for example, cortisol). If acute infectious diseases or surgery develop, it is necessary to consult an endocrinologist to adjust the dose of hormones taken.
- Independently reducing the dose of hormones or canceling them is unacceptable, since they lead to the development of a severe complication of the disease - acute adrenal insufficiency.
The course of the disease with early diagnosis and proper treatment is favorable. In women suffering from chronic adrenal insufficiency, pregnancy and normal childbirth are possible.
Sources
- Quénéhervé L., Drui D., Blin J., Péré M., Coron E., Barbara G., Barbaro MR., Cariou B., Neunlist M., Masson D., Bach-Ngohou K. Digestive symptoms in daily life of chronic adrenal insufficiency patients are similar to irritable bowel syndrome symptoms. // Sci Rep - 2021 - Vol11 - N1 - p.8077; PMID:33850177
- Ongidi IH., Abdulsalaam FY., Amuti TM., Kaisha WO., Awori KO., Pulei AN. Microscopic features of the rat adrenal gland associated with chronic codeine phosphate administration. // Anat Cell Biol - 2021 - Vol - NNULL - p.; PMID:33850059
- Gitto L., Stoppacher R., Serinelli S. Death Due to Adrenal Crisis: Case Report and a Review of the Forensic Literature. // Am J Forensic Med Pathol - 2021 - Vol - NNULL - p.; PMID:33833192
- Jeican II., Inișca P., Gheban D., Tăbăran F., Aluaș M., Trombitas V., Cristea V., Crivii C., Junie LM., Albu S. COVID-19 and Pneumocystis jirovecii Pulmonary Coinfection-The First Case Confirmed through Autopsy. // Medicina (Kaunas) - 2021 - Vol57 - N4 - p.; PMID:33804963
- Manosroi W., Pipanmekaporn T., Khorana J., Atthakomol P., Phimphilai M. A Predictive Risk Score to Diagnose Adrenal Insufficiency in Outpatients: A 7 Year Retrospective Cohort Study. // Medicines (Basel) - 2021 - Vol8 - N3 - p.; PMID:33801854
- Wang YL., Zhang HL., Du H., Wang W., Gao HF., Yu GH., Ren Y. Retroperitoneal laparoscopic partial resection of the renal pelvis for urothelial carcinoma: A case report. // World J Clin Cases - 2021 - Vol9 - N8 - p.1916-1922; PMID:33748242
- Nishio K., Okada Y., Kurozumi A., Tanaka Y. . // J UOEH - 2021 - Vol43 - N1 - p.97-102; PMID:33678791
- Lee J., Anderson L.J., Migula D., Yuen KCJ., McPeak L., Garcia JM. Experience of a Pituitary Clinic for US Military Veterans With Traumatic Brain Injury. // J Endocr Soc - 2021 - Vol5 - N4 - p.bvab005; PMID:33655093