Bilateral hemianopsia is a neurological disorder characterized by bilateral blindness in half of the visual fields. Tractus hemianopsia (from the word “path”) is caused by damage to the optical pathways, and central hemianopsia develops when the cortical areas responsible for visual perception are damaged. In other words, hemianopsia is the loss of half of visible vision on the left or right, but always in both eyes.
Damage to the optic tract usually results in death of the optic nerves. With the central origin of the disease, the optic nerves do not atrophy and continue to function.
Loss of visual fields by origin is divided into acquired and congenital. The congenital variant occurs when the development of the central nervous system is impaired during the period of intrauterine maturation of the fetus. It is almost always combined with other defects of the nervous system and rarely occurs as an isolated pathology. The acquired variant develops mainly in people whose average age is from 30 to 50 years. More common in women.
Causes
Hemianopsia occurs when the optic tract, cortex, or subcortical areas are damaged. It follows that it is necessary to look for the nature of damage to the visual system.
- Pathology of cerebral circulation due to arterial blockage due to atherosclerosis or arterial hypertension. They lead to an acute lack of blood in the vessels, as a result of which parts of the brain die from lack of oxygen and nutrients. The type of visual field pathology is determined by the pool and area of the brain in which the blood flow is disrupted. Vision is often impaired when blood supply to the posterior cerebral artery, which supplies the occipital and parietal cortex, is reduced. With a stroke or aneurysm, intracranial pressure increases and hemorrhage into the brain tissue is provoked, and the visual pathways are damaged.
- Inflammation of the meninges and brain parenchyma. Inflammation of the membranes, if localized primarily in subcortical structures, compresses parts of the brain and causes mechanical compression. This impairs the conduction of nerve impulses.
- Volumetric processes in the cranium: tumor, cyst, purulent accumulation.
- Iatrogenic factor. During surgery on the central nervous system, the neurosurgeon may accidentally damage the visual pathways.
- Congenital defects of the central nervous system, accompanied by severe disruption of parts of the brain or hypertension syndrome: dropsy, microcephaly, encephalocele or dysplasia of telencephalon tissue.
A special case of loss of fields, for example, homonymous hemianopia on the left, is determined by the area of brain damage.
Complications of hemianopsia
Hemianopia negatively affects a person's quality of life. People with this diagnosis are unable to independently carry out their usual daily activities – eating, reading, driving. They often get lost in space and have difficulty communicating with other people.
As hemianopsia progresses, there is a risk of complications of the disease, including complete blindness. The outcome of the pathology depends on its type, age category, individual characteristics of the human body and many other factors.
With timely initiation of treatment, the prognosis is favorable. In this case, vision can be restored completely. Otherwise, the person goes blind and becomes disabled. If hemianopia occurs due to a stroke, the disease has a favorable prognosis. As a rule, visual functions are restored within six months.
Varieties
There are several types of neurological disease:
Homonymous hemianopsia (eponymous hemianopsia)
Unilateral hemianopsia is incomplete loss of vision. Characterized by loss of margins on the right or left. Homonymous hemianopsia occurs when the structures of the central nervous system are damaged by infection, stroke, or mechanical trauma.
Features of the pathology. The homonymous variant is reversible. Thus, right- or left-sided blindness can be a sign of aura during migraine. Aura is the preceding stage of a unilateral headache. Hemianopsia may be one of the signs of a stroke. Contralateral hemianopsia occurs when there is unilateral damage to the optic nerve. For example, if the optic nerve on the left is damaged, the right lateral visual fields will fall out and right-sided homonymous hemianopsia (right hemianopsia) will occur. If the right optic nerve is damaged, there will be left-sided homonymous hemianopsia. With complete damage to the lateral geniculate body, complete unilateral hemianopia occurs.
Bitemporal heteronymous hemianopsia
By breaking down each word, you can understand the term. “Bi” means two, “temporal” means the side of the temples of the head. The pathology is manifested by the disappearance of both fields of vision from the temples. Bitemporal hemianopsia occurs when the optic pathway is damaged in the area where the optic nerves intersect.
Heteronymous hemianopsia occurs when the optic nerves are damaged, most often caused by a tumor. Often these are neoplasms in or above the pituitary gland. Temporal hemianopsia is often a symptom of pituitary adenoma.
Binasal hemianopsia
Bi - this is two, that is, on both sides, nasal - meaning the nasal part. The pathology is characterized by bilateral loss of visual fields in the nasal part of the face. Binasal hemianopsia occurs when the optic tract and brain structures are damaged. Also, binasal hemianopsia occurs when the central nervous system is damaged against the background of hydrocele of the brain.
Upper quadrant hemianopsia
Unlike previous types of visual field loss, this quadrant hemianopsia is characterized by loss of the upper half of vision. Superior hemianopsia develops due to damage to the ventral part of the optic tract.
Inferior quadrant hemianopsia
Characterized by loss of lower vision on both sides. Inferoquadrant homonymous hemianopsia occurs when the posterior region of the optic tract or parietal cortex is damaged. Thus, when the parietal cortex is damaged, complete hemianopia occurs.
Mechanisms of visual impairment
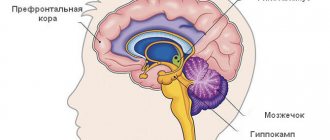
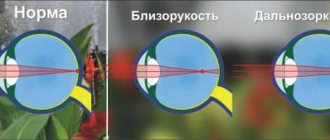
The nerve impulse that, under the influence of light, appears on the retina - the nervous tissue of our eye - is transmitted along a chain of neurons as part of the optic nerve, the visual pathway, to specific areas of the brain to process the received information and transform it into a whole picture.
Since a person has two eyes, we should have two pictures, but thanks to the peculiarities of the anatomy and physiology of the nervous system, the two images merge into one.
Photo: https://pixabay.com/photos/eye-iris-look-focus-green-1132531/
One of the reasons for this transformation is that the nerve fibers from one eye at a certain moment are divided into two groups, one of which continues to transmit information to the brain on its side, and the second goes to the opposite side, connecting with the first group of the other eye. This crossing of fibers is called chiasma.
When the nerve pathway is compressed or its blood circulation is disrupted, the affected area ceases to function, and the transmission of nerve impulses from the eye to the brain is interrupted, and the eye seems to go blind in patches. When examining visual fields, the doctor can make an assumption about where the dysfunctional area is located and can suggest where to look for the pathological process.
In the future, to determine the cause of the development of visual field impairment, an MRI or CT scan of the brain is done, sometimes with contrast.
- If the pathological process is located before the chiasm, blindness or partial loss of vision occurs in only one eye.
- If the chiasm is compressed, then the temporal halves of vision of both eyes fall out - the person perfectly sees what is happening in front of him, but does not notice what is on the side of him until he turns his head in the right direction.
- If the lesion is localized after the chiasm, then loss of the temporal half of vision occurs on one side and the nasal half on the other, or vice versa.
The size of the lost field depends on the force of compression of a particular part of the visual pathway or on the degree of disruption of its blood circulation.
Clinical picture
Patients suffering from pathology often face everyday discomfort. A visual defect prevents a person from seeing objects in the lost field of vision. For patients, ordinary events, such as crossing the road, turn into danger: a person cannot see an approaching car. People are not recommended to drive any vehicle, as there is a risk of accidents.
Lost fields of vision do not even allow you to see the food on the other half of the plate, and difficulties arise when reading, since the other half of the page of the book is not visible. Reading turns into torture for people: people need to make more eye movements.
The neurological illness is accompanied by elementary visual hallucinations. Photopsia is the perception of non-existent ugly phenomena and objects, for example, a suddenly appearing point, flashes, lightning or lights. Often, elementary visual hallucinations with hemianopsia occur after a recent stroke.
Everyday life and basic household things cause psychological discomfort in patients: their actions from the outside seem ridiculous and sloppy. Some patients develop depression and other neurotic disorders. As a result of loss of visual fields and a feeling of incapacity, some patients withdraw from social life, preferring to spend time alone.
For patients with hemianopia, the range of possible specialties is limited. Thus, such patients cannot transport passengers or work in places where external assessment of objects is required, for example, in engineering or construction.
The clinical picture of visual impairment, in addition to photopsia, is supplemented by agnosia. This is a neurological disorder characterized by impaired recognition of objects in the visual channel. Patients often exhibit prosopagnosia—impaired recognition of familiar faces. Some patients experience Anton-Babinsky syndrome: people deny the presence of their pathology.
Congenital hemianopsia is often combined with developmental defects in the subcortical and cortical parts of the brain: the thalamus, brain stem and parietal cortex. Therefore, the clinical picture is supplemented by the following pathologies:
- Paresthesia is a perverted sensation. Thus, patients often suffer from tingling skin and complain of flying spots in front of their eyes.
- Violation of deep sensitivity. Patients have impaired pain and tactile perception.
Diagnosis of hemianopsia
To diagnose hemianopsia, you must consult a doctor promptly.
The specialist performs the following procedures:
- analysis of the visual fields of each eye;
- determination of visual acuity;
- fundus ophthalmoscopy.
The latter procedure may not give the required results. At the initial stages of pathology development, changes in the structure of the fundus may be absent or symptoms may be mild. Subsequently, the manifestations become more noticeable.
Pronounced destructive changes can be seen only after a year of identifying the pathology. The difficulty of diagnosing the disease in the initial stages of its development lies in the fact that it does not cause visual impairment. Such consequences appear only after a few months in the absence of adequate therapy.{banner_gorizontalnyy2}
After a preliminary diagnosis, a more detailed examination is prescribed.
It helps determine the stage and degree of development of the disease. Such diagnostics involve the use of tools. The following procedures apply at this stage:
- tomography;
- angiography;
- radiography;
- ultrasonography;
- application of electromagnetic waves.
To objectively determine the degree of loss of specific areas from the visual field, perimetry is performed.
This procedure helps to project the boundaries onto a spherical plane. If you suspect the presence of a disease, the examination should be carried out in the following order:
- The doctor performs a visual examination of the eyes. This is done one by one. Moreover, one eye is covered with the palm of the hand, and the second is examined from a distance of 1 m.
- During the examination, the ophthalmologist asks the patient to concentrate on his finger. After this, he gradually moves his finger from the areas to the periphery and in the opposite direction. This helps identify the area where the patient is losing vision.
- Provided that the doctor does not have vision pathologies, he and the patient must correctly establish boundaries, beyond which the person cannot see his own finger. This experimental method helps to quickly identify hemianopsia.
Classification
According to the topic of the lesion, it happens:
- Tractus hemianopsia. Develops due to damage to the visual pathways. It is characterized by atrophy of the optic nerves, lack of pupillary response to light and asymmetry of visual field loss.
- Central hemianopsia. Develops when the central parts of the brain are damaged. The pathology is not accompanied by atrophy of the optic nerves; they continue to respond to light stimuli. The central variant is accompanied by a symmetrical loss of visual fields.
Prevention of hemianopsia
There is no specific prevention of hemianopsia in children and adults.
To prevent the development of pathology, you need to adhere to the following recommendations:
- avoid traumatic head injuries;
- avoid increased eye strain;
- monitor the condition of the circulatory system;
- avoid intoxication of the body.
Quite often, hemianopsia develops against the background of other pathologies. This is why it is so important to systematically undergo preventive medical examinations. If any diseases are detected, you need to immediately begin their treatment.
Hemianopsia is a serious pathology that leads to a significant deterioration in the quality of life. To cope with the disorder, you need to consult a doctor in a timely manner and undergo a detailed examination.
How is the disease detected?
Diagnosis of visual impairment is carried out using visual field testing. The purpose of the express method is to identify field pathologies. In neurological practice, a special hand hammer is used. A neurologist sits down opposite a person and asks him to close one eye with his palm. The gaze of the open eye is fixed on the doctor's nose. The physician slowly moves the instrument from behind the patient's head from the periphery to the center from all sides. The patient must be told immediately when he sees the hammer.
Among instrumental methods, perimetry has the greatest diagnostic value. The procedure is carried out using a perimeter. As a result of the procedure, the doctor receives information about the boundaries of the visual fields for both eyes. Other visual defects are also detected. Computer campimetry is also used. It identifies disturbances in color perception in various areas of the retina and helps determine the level of disturbance.
To identify the cause of the disorder, computer and ultrasound diagnostics are used: computer and magnetic resonance imaging, Doppler ultrasound of cerebral vessels. Computer diagnostics helps in choosing treatment tactics, as it allows you to visualize the source of hemorrhage, tumor or abscess.
Treatment and prognosis
Treatment of hemianopsia is carried out in accordance with the nature of the underlying disease that caused it.
Depending on the severity and nature of this disease, as well as the extent of damage to the visual pathway, hemianopia is temporary or remains a permanent symptom of the condition.
In the medical department, everyone can undergo examination using the most modern diagnostic equipment, and based on the results, receive advice from a highly qualified specialist. The clinic provides consultations to children from 4 years old. We are open seven days a week and work daily from 9 a.m. to 9 p.m. Our specialists will help identify the cause of vision loss and provide competent treatment for identified pathologies.
You can find out the cost of a particular procedure or make an appointment at the Moscow Eye Clinic by calling 8 (800) 777-38-81 (daily from 9:00 to 21:00, free for mobile phones and regions of the Russian Federation) or using the form online entries.
Fomenko Natalia Ivanovna
Symptoms
Hemianopsia immediately begins with an acute form and accompanies a traumatic brain injury or stroke. Patients complain that entire areas of the visual image disappear from the field of vision or that large spots appear before the eyes - they prevent clear visualization.
Often the acute form of hemianopsia is accompanied by the following symptoms:
- dizziness;
- nausea, vomiting;
- violation of spatial orientation;
- increased blood pressure;
- violation of facial expressions;
- numbness of the limbs;
- speech disorder.
But sometimes the disease occurs without pronounced symptoms: the patient complains of constant headaches, which are accompanied by partial loss of visual fields; unmotivated weakness and general malaise appear. If such symptoms appear, you should immediately see an ophthalmologist or therapist.
Patients with hemianopsia find it difficult to cope with everyday responsibilities and perform normal work. Walking around the city is dangerous: they do not always see approaching vehicles, do not notice many objects on the road surface, and are poorly oriented in space.
When peripheral vision is lost, it is difficult for a person to navigate space, take care of himself, and perform daily work.
A healthy visual system provides a person with central and peripheral vision. With hemianopia, peripheral vision is absent, which leads to disorientation in space. The field of view is the totality of objects that a person sees simultaneously when fixing his gaze on one thing. When part of the visual field is lost, orientation in space is difficult or impossible.