What are genital warts (AC), what causes them, and how common are they?
OKs are warty growths that most often appear in the genital area or anus of a person. They can be very small or quite voluminous, resembling cauliflower in appearance. OK are by nature a viral disease and, in fact, one of the manifestations of infection with the human papillomavirus (HPV), which causes them.
It is known that up to 75% of young sexually active women are infected with one or more types of HPV and approximately 15% of them have some form of infection. Moreover, from 50 to 75% of those infected were infected with types of the virus with a high oncological risk, and 1% of those infected had OK. Among young men, the prevalence of HPV infection is similar, but lifetime carriage is less common. Currently, about 5 million cases of HPV infection are registered annually in the United States, and the total number of infected people is about 20 million people. Thus, HPV is the second most common predominantly sexually transmitted disease (STD) in the United States, second only to genital herpes infection (45 million infected). We do not have data on the prevalence of HPV in Russia.
Incubation period and routes of infection with condylomas
The papilloma virus enters the body from another person suffering from this infection. Infection can occur in different ways. The path can be sexual or contact-household. But it is obvious that if the formation is localized inside the urethra, there can be no talk of any domestic infection.
In everyday life, we rarely come into contact with another person's urethra. This happens much more often during sex. The incubation period for papillomavirus is usually long. It lasts for at least 3 months. Sometimes it lasts six months or even more. Only after this can condylomas appear. Moreover, not everyone has them. With good immunity, formations often do not appear. The virus is contained by the immune system.
And after a year, for most people it leaves the body. Therefore, the infection goes unnoticed. It can only be detected by chance by examining the patient for HPV.
What is the relationship between HPV and human cancer?
The clearest causal role of HPV has been demonstrated in cervical cancer. Thus, high-risk HPV types (see Table 1) were found in 93 - 99% of women with cervical cancer. Previously, it was found that the most susceptible to cervical cancer are women who began sexual activity early, had an STI, and also had a large number of sexual partners, as well as those who were in contact with men whose partners had cervical cancer. It turned out that high-risk HPVs contain regions with high oncogenic activity (E6 and E7) in their genome. When HPV invades the genome of cells in the cervical mucosa, regions of the genome E6 and E7 stimulate the synthesis of corresponding proteins, which in turn interact with proteins that regulate cell division and cell death. The E6 protein suppresses the activity of the P53 gene (and the corresponding protein), and the E7 protein of the retinoblastoma gene, which stimulates the process of apoptosis (programmed cell death). This leads to the predominance of cell reproduction over cell death, which stimulates the uncontrolled malignant growth of cervical epithelial cells and the development of cervical cancer. Thus, the International Agency for Research on Cancer has concluded that high-risk HPV types are the leading cause of cervical cancer.
However, it is known that most women infected with HPV do not develop cervical cancer and the presence of HPV is “necessary” but not “sufficient” for the development of this disease. The development of cervical cancer in people infected with HPV is facilitated by smoking, long-term use of hormonal contraceptives, and the presence of other STIs, such as chlamydia, namely Chlamydia trachomatis, herpes simplex virus type 2. In addition, vitamin A deficiency, genetic predisposition and immunodeficiency contribute to the development of cervical cancer in the presence of HPV. In addition to cervical cancer, the causative role of HPV has been established in cancer of the anal area (especially in homosexuals), and in cancer of the vulva, vagina and penis. Some cases of cancer of the mouth, larynx and esophagus are also possibly related to HPV.
Every year, up to half a million new cases of cervical cancer occur worldwide. Most of these cases are registered in developing countries, where preventive programs of annual screening examinations for HPV, dysplasia and cervical cancer do not work or work poorly. The introduction of similar preventive programs in developed Western countries has reduced the incidence of cervical cancer by 75%. Although the incidence of other HPV-related cancers is much lower, the incidence of anal cancer among gay men is estimated to be 4 times higher than the incidence of cervical cancer in women (35 cases per 100,000 homosexuals per year, versus 8.3 cases per 100,000 women). population per year).
Types of condylomas: classification
All condylomas that arise in the urethra can have different colors, sizes and structural features. However, experts distinguish 2 main types of these neoplasms:
- flat condylomas. They are rare, but very dangerous. And their main danger is that they do not give any symptoms for a long time, and they can only be identified during examination by a urologist (and even then, not always). But they tend to degenerate into cancer - this is their main danger.
- genital warts. They occur quite often, they look like a neoplasm on a small stalk, which grows into the urethral cavity, and when it reaches a large size, it begins to protrude in the area of the external opening of the urethra. Pointed papillomas (condylomas) are characterized by very rapid growth.
What are the goals of treatment for diseases caused by HPV, and how is it carried out?
Diagnosis, treatment and prevention of genital diseases caused by HPV in men is carried out by urologists, in women - by gynecologists. Unfortunately, there are currently no methods of systemic action on HPV in the human body (antiviral agents) that could be used to completely destroy the virus. The main goal of treatment for OCs is their removal using electro- or laser coagulation, excision, cryodestruction (destruction by cold), as well as using chemicals, cell toxins (podophyllin) or immunomodulators applied topically. Removing OK solves mainly a cosmetic problem; there is no data confirming that removing OK helps to completely remove HPV from the body or reduce the risk of its sexual transmission or infection of the fetus during childbirth. There is no evidence that OC treatment has any effect on the likelihood of developing cancer. However, from a common sense point of view, removal of OCs should reduce the risk of development and recurrence of diseases caused by HPV.
The main goal of treatment of squamous epithelial lesions of the cervix is the prevention of cervical cancer. If a cytological Pap smear shows the presence of a lesion of unknown significance at the risk of malignancy, dynamic observation with Pap smears performed every 4 to 6 months for 2 years is indicated until there are 3 consecutive negative (without any pathological changes) smears. Women with high-risk intraepithelial lesions require immediate colposcopy and possibly biopsy of the detected lesions for more detailed histological evaluation. If CIN 1 is identified as a result of histological examination, dynamic observation is indicated, because the vast majority of such lesions undergo spontaneous regression to normal. For lesions of CIN 2/3, active treatment is required, which consists of cryodestruction, laser evaporation or loop electrosurgical excision (conical excision or conization) of the cervix.
Recent randomized clinical trials have shown that all three methods have similar rates of complications (2 - 8%), persistence (3 - 5%) and recurrence (13 - 19%) of lesions. Risk factors for persistence (lack of treatment effect) were a large affected area, relapse - older age, the presence of oncogenic HPV types 16 and 18, as well as previous treatment.
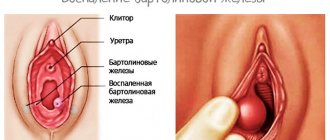
Condylomas near the urethra
If condylomas appear near the urethra, this means that in the near future they may also appear inside the urethra. Therefore, treatment is required to prevent this from happening. After all, if condylomas near the urethra create only an aesthetic defect, then inside they can cause unpleasant symptoms.
Sometimes they provoke complications that require long-term treatment. When infected with the papilloma virus, formations rarely appear in the urethra initially.
Usually, secondary damage to the mucous membrane occurs due to the presence of papillomavirus in nearby areas.
What is the prevention of diseases caused by HPV?
Examination of sexual partners of patients with diseases caused by HPV has no proven value in terms of preventing their occurrence/recurrence. However, theoretically, timely and complete removal of OCs and intraepithelial lesions can reduce the risk of these diseases, including cervical cancer. It has not been proven that condoms can protect against HPV transmission, but their use reduces the risk of developing OCs and cervical cancer. The most promising method of preventing and treating the early stages of diseases caused by HPV are specific polyvalent (for HPV types 6, 11, 16 and 18) vaccines, which are currently in clinical trials. In summarizing the known information about diseases caused by HPV, the US Center for Disease Control (CDC) draws attention to the public's knowledge of the following key points:
- HPV is an extremely common STD
- It is rarely possible to identify the source of infection due to the highly variable incubation period
- The natural progression of diseases caused by HPV is often benign, and treatment sometimes requires several months. Relapses often occur (up to 50% of cases).
- OCs are most often caused by HPV types that do not cause cervical cancer
- Infectiousness of sexual partners decreases over time
- The effectiveness of condoms in protecting against HPV has not been proven. However, the use of condoms by patients with HPV for new sexual contacts is considered mandatory.
- You should tell new sexual partners that you have previously been infected with HPV
Women, especially those of sexually active age, need to know that the basis for the prevention of cervical cancer is mandatory annual preventive examinations by a gynecologist with a cytological examination of the cervical epithelium according to Papanicolaou, as well as, if necessary, HPV typing, colposcopy and cervical biopsy.
Symptoms of condylomas inside the urethra
The formations are located only in the terminal part of the urethra.
It is only theoretically possible to bring them deeper. For example, during medical procedures.
Under natural conditions, the papillomavirus does not penetrate deeply into the urethra. Therefore, in most cases, condylomas are visible to the naked eye. They extend beyond the urethra and are partially outside the urethra. There may be no symptoms.
The reason for the patient’s request in this case is the fact of visual detection of condyloma. Since the appearance of formations inside the urethra is always a cause for concern.
Subjective symptoms of condylomas in the urethra in men and women are also possible:
- itching
- difficulty urinating
- urine splashing
- painful sensations
- discharge of blood from the urethra
- wall adhesion
Objectively, the doctor detects small pink formations. They grow on a small base.
There may be an inflamed mucous membrane nearby. Symptoms get worse when complications occur. Sometimes condylomas in the urethra break off or become infected.
Necrosis may occur if the blood supply is disrupted. In this case, signs of nonspecific urethritis appear. There may be pus in the urine.
A person feels pain in the urethra, feels an unpleasant odor, and complains of pain when urinating.