- Modern methods of treating prostate cancer
- Active Surveillance
- Surgical treatment of prostate cancer
- Radiation therapy for prostate cancer
- Chemotherapy for prostate cancer
- Hormonal therapy for prostate cancer
- Treatment of stage 4 prostate cancer
- Treatment of prostate cancer metastases to bone
- Advantages of prostate cancer treatment at Euroonco
- Patient reviews of prostate cancer treatment at Euroonco
There are different types of treatment for prostate cancer in men; the doctor chooses tactics taking into account a number of factors. First of all, they focus on the stage of the tumor. If it does not extend beyond the prostate gland, surgical treatment is possible. If there are metastases in the lymph nodes, bones and other organs, surgical treatment will not lead to recovery.
It is also necessary to take into account concomitant health problems, and they usually exist, because malignant prostate tumors are more often diagnosed in older men. Such patients often suffer from arterial hypertension and have a history of stroke or heart attack. In such cases, surgery is often contraindicated.
Active Surveillance
For some men, due to age or underlying health problems, treatment can lead to complications and side effects that are more serious than the problems caused by the cancer itself. In such cases, the doctor may adhere to active surveillance. This tactic is possible in the following cases:
- The patient does not experience symptoms.
- The tumor is predicted to grow slowly.
- The tumor is small in size.
- The cancer has not spread beyond the prostate gland.
Find out the exact cost of treatment
Active surveillance tactics involve doctor's examinations and blood tests for prostate-specific antigen every six months. Once a year, your doctor may order a prostate biopsy.
Surgical treatment of prostate cancer
For prostate cancer, a radical prostatectomy is performed, an operation during which the prostate gland and surrounding tissue, including the seminal vesicles, are removed.
Radical prostatectomy can be performed in different ways:
- Retropubic prostatectomy is performed through a longitudinal incision from the umbilicus to the pubis. Usually the patient is discharged from the clinic a few days after the operation, the recovery period lasts several weeks.
- In a perineal prostatectomy, an arcuate incision is made between the scrotum and anus. This operation is faster than retropubic prostatectomy, but it makes it difficult to access the lymph nodes and is more likely to cause erection problems.
- Laparoscopic prostatectomy is performed using special instruments through punctures in the abdominal wall. It is accompanied by less bleeding and less tissue trauma compared to open interventions, and the recovery period is shortened. But the risk of complications is approximately the same.
- Robotic prostatectomy is performed using the da Vinci robot. In essence, this is the same laparoscopic intervention, but the surgeon does not hold the instruments himself, but controls the movements of the robot through a special remote control. Thanks to this, the movements of the instruments are more precise. But there is no evidence that it helps reduce the risk of complications.
Possible complications after radical removal of the prostate: urinary incontinence, erectile dysfunction, slight shortening of the penis, inguinal hernia, infertility, lymphedema (swelling due to removal of lymph nodes).
Rational therapy for prostate cancer
Prostate cancer (PCa) is one of the most pressing medical problems worldwide. This is primarily due to high morbidity. About 15% of all neoplasms registered in developed countries are PCa (Heidenreich A., 2007).
In 2006, in Europe, the incidence of prostate cancer was 24% among all neoplasms in men, ranked 1st in the morbidity structure, and was the cause of death in 11% of men (Farley J., 2007). In Russia, the incidence of prostate cancer is 18 per 100,000 male population, with an increase in incidence from 1994 to 2004. amounted to 131.39% (1st place), the average annual increase was 8.75%. There is also a high mortality rate from prostate cancer (9.5 per 100,000 male population) and an increase in mortality (from 1994 to 2004 by 62.99%).
Considering that the best treatment results for prostate cancer are achieved in the presence of a localized form of cancer, the possibility of early detection of a tumor that does not yet have clinical manifestations - the so-called prostate cancer screening - is of great importance. When screening, three methods of examining the patient are used - monitoring the level of prostate-specific antigen (PSA), digital rectal examination (DRE) and transrectal ultrasound examination of the prostate (TRUS).
PSA is a glycoprotein produced by the secretory epithelium of the prostate. It has been found that with a malignant tumor, the amount of PSA in the blood serum can increase significantly, however, an increase in PSA levels in some cases can also be associated with other prostate diseases - prostatitis and prostate adenoma. To date, the threshold PSA level that may indicate the presence of prostate cancer remains unclear, but the most commonly considered threshold for men under 60 years of age is 2.5–3 ng/ml (Guidelines EUA 2008).
When determining treatment tactics, the tumor stage and degree of differentiation, the patient’s age, the presence of clinical manifestations of the disease, the likelihood of a long relapse-free period, the risk of complications, as well as the patient’s wishes are taken into account.
In patients with severe intercurrent diseases, with a modest life expectancy (less than 10 years), in the absence of clinical manifestations of localized forms of stage 1-2 prostate cancer with high and moderate tumor differentiation, watchful waiting is possible. Active monitoring of such patients with regular monitoring of PSA, DRE, TRUS for the purpose of early detection of possible cancer progression and transition to aggressive treatment tactics shows better patient survival results compared with immediate prescription of hormonal drugs. Therefore, hormonal therapy in patients with stage 1-2 prostate cancer is not recommended by the European Association of Urology.
Radical prostatectomy is recommended for patients who do not have significant concomitant pathology and have a long life expectancy (more than 10 years). With proper selection of patients, radical prostatectomy can achieve excellent 10- and 15-year survival rates - 90 and 82%, respectively. The most important prognostic factors influencing the outcome of surgery are the degree of tumor differentiation (sum of Gleason scores), stage of the disease and preoperative PSA level. The best prognosis is for patients with a Gleason score of less than 7 and stage T1. A high preoperative PSA level is an unfavorable prognostic sign for disease recurrence.
Radiation therapy is indicated for patients with local forms of prostate cancer (T1-T2), who wish to avoid surgical treatment or have a high surgical and anesthetic risk, as well as patients with stage T3N0M0. Candidates for radiation therapy must have a reasonably long life expectancy. In patients with a high risk of lymph node involvement (PSA>10 ng/ml, Gleason score>7), prior laparoscopic pelvic lymphadenectomy is advisable. One of the effective methods of radiation exposure to the prostate gland in the treatment of stage T1-T2 is the use of brachytherapy or interstitial radiation therapy. The essence of brachytherapy is the introduction of radioactive I125 granules into the prostate gland under ultrasound control. In this case, unlike external beam radiation therapy, the surrounding tissues are practically not affected. The procedure for introducing capsules takes about an hour and is carried out on an outpatient basis, which distinguishes it from other types of radiation treatment.
Currently, new methods of treating localized prostate cancer are being introduced, such as cryotherapy, laser therapy, and focused high-intensity ultrasound.
Hormone therapy (androgen deprivation) is the main treatment method for locally advanced and disseminated prostate cancer; it is effective in more than 85% of cases. In patients with stage T3 prostate cancer with the absence of clinical symptoms of the disease, the presence of well- or moderately differentiated tumors, and a life expectancy of less than 10 years, vigilant observation (delayed treatment) can be used.
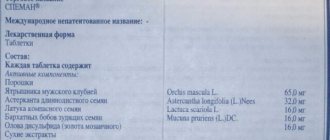
Currently, androgen deprivation is achieved by castration (chemical or surgical), the use of antiandrogens, a combination of the first two methods (maximum androgen blockade) and rarely, as second-line therapy, the use of female sex hormones (estrogens).
The cheapest and fastest method of achieving castration testosterone levels is bilateral orchidectomy. The advantages of surgical castration are low cost, independence from the degree of treatment financing, and reliability. Given the negative psychological effect of surgical castration, methods of medical castration using analogues of luteinizing gonadotropin-releasing hormone (a-LHRH) have become widespread. Three weeks after the start of treatment, a decrease in serum testosterone to post-castration values occurs. The disadvantage of medical castration is the high cost of drugs and the direct dependence on funding for treatment.
With the advent of new modern pharmacological drugs, it has become possible to prescribe antiandrogens as monotherapy. A number of studies have shown the effectiveness and safety of monotherapy with the nonsteroidal antiandrogen bicalutamide (Casodex) at a dose of 150 mg/day in the treatment of patients wishing to preserve libido and potency, although the results of recent studies have shown better castration results compared with antiandrogens. To obtain a castration effect, it is recommended to increase the dose of bicalutamide to 300-600 mg (Tyrrell CJ. BJU international 2006). Increasing the dose of antiandrogens is accompanied by an increase in the number of side effects (diarrhea, hepatotoxicity, cardiotoxicity, myocardial infarction, angina pectoris, thromboembolism, obesity, dyslipidemia, diabetes mellitus, osteoporosis), which sharply reduce the quality of life of patients.
To eliminate androgens of testicular and adrenal origin, maximum androgen blockade (MAB) is used. MAB involves the use of an antiandrogen in combination with LHRH or orchidectomy. The benefits of MAB over LHRH analogue monotherapy in improving overall survival remain controversial. Better survival results for patients with locally advanced prostate cancer are achieved with delayed administration of antiandrogens compared with their immediate use. In case of metastatic disease, immediate administration of antiandrogens is recommended (Isbarn H. et al., 2009).
The diagnosis of hormone-resistant prostate cancer (HRPC) is established in the presence of an increase in PSA levels and/or any other signs of disease progression with adequate androgen blockade with confirmed castration testosterone levels. Initially, most prostate cancers are represented by three cell populations: androgen-dependent cells, which require androgen stimulation for development; androgen-sensitive cells - they do not die in the absence of androgens, but their growth slows down; androgen-independent cells - they do not require androgens for their growth. The progression of the disease during hormone therapy is associated with the death of androgen-dependent cells and the growth of the androgen-independent clone. At the same time, primary hormone resistance of prostate cancer is possible, which accounts for 15-20% of cases.
One of the methods aimed at preventing the development of hormonal resistance in prostate cancer is intermittent androgen blockade (IAB). The concept of IAB consists of temporary androgen blockade, which partially preserves tumor stem cells. Once a certain response is achieved, antiandrogen therapy is stopped to allow the growth of new clones of androgen-sensitive cells. Therapy is resumed if disease symptoms progress and PSA rises. This method allows you to delay the development of a hormonally resistant state of cancer cells. IAB has positive aspects associated with low toxicity and reduced treatment costs.
In 1993, H. Scher and W. Kelly reported that withdrawal of flutamide in patients with maximal androgen blockade resulted in a decrease in PSA, symptomatic response, and objective improvement. Numerous studies have confirmed this effect with other antiandrogens, including bicalutamide, nilutamide, cyproterone, and even progesterone. This phenomenon has been called the "Antiandrogen Removal Effect." Discontinuation of antiandrogens is now the first standard action when disease progression is detected during hormonal therapy in patients with cancer in the United States. The European Association of Urology recommends discontinuing antiandrogens, if they have been prescribed, from the moment disease progression is established. The effect of antiandrogen withdrawal may be observed within 4 to 6 weeks after discontinuation of flutamide or bicalutamide therapy.
In recent years, effective polychemotherapy regimens for hormone-resistant prostate cancer (HRPC) have been developed. Docetaxel at a dose of 75 mg/m2 every 3 weeks showed significant benefits in increasing survival compared with other chemotherapy regimens in patients with metastatic HRPC. In patients with metastatic HRPC with bone symptoms, both docetaxel and mitoxantrone with prednisolone or hydrocortisone are effective chemotherapy regimens. A search is underway for new effective drugs for the treatment of HRPC: blockers of the endothelin A receptor, which plays a key role in the progression of HRPC - ZD4054; targeted drugs - bevasizumab, aflibercept and antitumor vaccines - G-VAX, Provenge.
An important stage in the treatment of patients with prostate cancer with bone metastases was the introduction into practice of drugs from the group of bisphosphonates. After parenteral administration, bisphosphonates are transported by the blood to sites of active bone tissue remodeling, where they firmly bind to the mineral matrix of the bone; bisphosphonates act specifically in areas of osteolytic bone destruction observed in metastatic skeletal lesions. Zoledronic acid (Zometa) is currently the most potent intravenous bisphosphonate and the only effective bisphosphonate in the treatment of patients with prostate cancer. When choosing a bisphosphonate for systemic antiresorptive therapy, it should be taken into account that only zoledronate (Zometa) is active against all types of metastases in prostate cancer, and only Zometa has a registered indication for the prevention of complications of metastases in the bones of solid tumors, including prostate cancer, cancer kidney, bladder cancer. For prostate cancer, it is advisable to prescribe Zometa for a period of 24 months or more. Timely initiation and full treatment can reduce the risk of developing complications of bone metastases in prostate cancer by 30-41%, in hormone-resistant prostate cancer - by 50%, and increase the time to the first complication by 83% - more than 5 months . compared with no antiresorptive therapy, and also increase the time between the first and second complications by 30%. Treatment with zoledronate can increase the life expectancy of patients with advanced prostate cancer; According to studies, patients without fractures in the area of bone metastases live for 39 months. longer than patients with fractures. The good tolerability of zoledronate (Zometa) allows long-term treatment of patients with bone metastases, in the case of advanced prostate cancer – 24 months. and longer. In addition, the ability of zoledronate to inhibit neovascularization in tumors has been described, due to which zoledronate enhances the activity of other antitumor agents and helps improve treatment results.
Thus, the widespread introduction of screening programs will make it possible to diagnose early forms of prostate cancer, for which radical treatment methods show good patient survival results. Vigilant observation (delayed treatment) of asymptomatic elderly and senile patients with severe concomitant pathology is recommended, not only in the early localized stages of prostate cancer, but also in locally advanced ones. Immediate hormonal treatment is indicated only for patients with metastatic disease. The most effective method of androgen deprivation is castration (medical or surgical). The use of antiandrogens should be limited to cases of disease progression due to castration. When the process stabilizes, it is recommended to take a break from hormonal treatment under the control of PSA levels and analysis of symptoms. Treatment should be resumed at the first signs of disease progression. This tactic of patient management makes it possible to delay the onset of hormone resistance, improve the quality of life, and reduce the cost of treatment without compromising survival. It is recommended to discontinue antiandrogens, if they have been prescribed, from the moment the progression of the disease is established. The use of polychemotherapy with the inclusion of taxanes can improve the results of treatment of hormone-resistant prostate cancer. An important treatment method for patients with prostate cancer with bone metastases has been the use of bisphosphonates.
Radiation therapy for prostate cancer
Radiation therapy may be prescribed as an alternative to surgery. It is often as effective as surgery. Other indications:
- In combination with hormonal therapy for cancer that has spread beyond the prostate gland.
- When cancer recurs.
- As palliative treatment in later stages. This helps control tumor growth and increase the patient's life expectancy.
There are two types of radiation therapy used for prostate cancer: external and internal (brachytherapy). External radiation comes in different types:
- Three-dimensional conformal radiation therapy uses computer technology to determine the exact location of the prostate gland and tumor. This helps reduce damage to surrounding healthy tissue.
- Intensity modulated radiation therapy is a more advanced form of 3D conformal radiation therapy. The device not only irradiates the tumor from different angles, but also regulates the intensity of the radiation. This allows an even higher dose to be delivered to the prostate without irradiating healthy tissue.
- Stereotactic therapy uses modern technology to deliver the entire dose of radiation to where the malignant tumor is located. It allows the course of radiation therapy to be shortened, ending up lasting days instead of weeks.
In brachytherapy, a small bead that produces radiation is placed directly into the prostate gland. This treatment is used for men with early stage prostate cancer that is slowly growing. In later stages, brachytherapy is sometimes used in combination with external beam radiation therapy.
Brachytherapy (internal radiation therapy)
Internal radiation therapy uses radioactive beads the size of a grain of rice that are placed directly into the patient's prostate.
Special computer programs calculate the required dose. Imaging techniques such as transrectal ultrasound, CT, or MRI are used to correctly place the radioactive beads.
Typically, brachytherapy is used in the early stages when the tumor is expected to grow slowly. For example, for low-grade cancer.
The use of brachytherapy is limited by various factors. The risk of side effects is high in men who have had TURP of the prostate or have problems urinating.
The large size of the prostate may interfere with the correct installation of the grains. In this case, a short course of hormonal therapy may be prescribed to reduce the size of the organ.
There are 2 types of prostate brachytherapy.
Hormonal therapy for prostate cancer
It is known that male sex hormones - androgens - stimulate the growth of prostate cancer. The goal of hormone therapy is to lower the levels of androgens in the body or prevent them from interacting with cancer cells.
Hormone therapy stops tumor growth for a while. As monotherapy, it is not able to cure. Indications for its use:
- Presence of contraindications to surgical treatment and radiation therapy.
- Advanced prostate cancer when surgery and radiation therapy are ineffective.
- For aggressive tumors, when the risk of relapse is high, hormonal therapy is prescribed along with radiation therapy.
- It may be prescribed before radiation therapy to slow down tumor growth and improve treatment results.
Treatment for prostate cancer is constantly improving. More recently, a large study demonstrated the negative effects of hormonal therapy in patients with a recurrent process and low PSA levels. Euroonco doctors closely monitor such changes and offer their patients only treatment that meets modern standards.
Treatment methods for stage 2 prostate cancer
The choice of therapeutic tactics depends on age, concomitant diseases, and characteristics of the tumor. When a malignant tumor is diagnosed, surgery is not always indicated - stage 2 prostate cancer is successfully treated with:
- conservative methods (drug treatment);
- radiation therapy;
- innovative techniques (HIFU therapy, cryoablation and focal therapy).
If radical surgery is necessary, modern minimally invasive techniques are used.
Treatment of stage 4 prostate cancer
At stage IV, prostate cancer spreads to the bladder, rectum, lymph nodes, and distant metastases appear in the bones and various organs. But even at this stage, depending on the extent of the process, remission can sometimes be achieved. In cases where cancer is incurable, palliative treatment will help curb its growth for a while and prolong the patient's life.
Typically, treatment for stage 4 prostate cancer includes the following:
- Hormonal therapy, in some cases in combination with chemotherapy.
- Surgery. If the cancer has not spread to the lymph nodes and there are no distant metastases, a radical prostatectomy can be performed. In other cases to fight
- with symptoms, they resort to palliative intervention - transurethral resection of the prostate (TURP).
- If the patient is contraindicated for all treatments and is asymptomatic, active surveillance may be considered.
Survival Projections
At the beginning of its development, the disease can be cured. If stage 2 prostate cancer is diagnosed, the prognosis is positive with timely provision of qualified assistance. It is necessary to remember that self-medication is inadmissible, which can lead to a worsening of the clinical picture.
It is important to diagnose stage 2 prostate cancer as early as possible - life expectancy depends on the development of the pathology and the condition of the body. At the clinic named after R.M. Fronshtein is accepted by leading urologists; you can make an appointment by phone or through the website. Timely contact with specialists is the first step on the path to recovery.
Treatment of prostate cancer metastases to bone
If bone metastases are detected, hormonal therapy, radiation therapy, and chemotherapy are prescribed. In addition, in the treatment of bone metastases in prostate cancer, bisphosphonates (drugs that slow down bone destruction), denosumab (the same effect as bisphosphonates, but a different mechanism of action), drugs of adrenal hormones (reduce pain), and painkillers are used.
| More information about treatment at Euroonco: | |
| Urologists-oncologists | 4700 rub. |
| Chemotherapy appointment | 6900 rub. |
| Prostate biopsy | 22500 rub. |
| Palliative care in Moscow | from 40200 per day |
Exposure planning
The goal of modern radiation therapy for prostate cancer is to destroy malignant cells with the most gentle effect on neighboring tissues and organs. The effectiveness of radiotherapy largely depends on the quality of radiation planning.
To prepare patients and accurately determine the position and size of the tumor, such types of high-tech examinations as computed tomography, MRI (magnetic resonance imaging, etc.) are used.
In many clinics, the standard of preparation for radiation therapy is 3D technology and the use of a stereotactic attachment. The three-dimensional model makes it possible to most accurately determine the volume of the tumor and the intensity of radiation, which allows expanding the indications for sparing treatment and gives hope for the recovery of patients who have not previously received radiation therapy according to indications.
Thanks to the use of new techniques and the use of high-tech equipment, it is possible to significantly reduce side effects and quickly return a man to his usual lifestyle.
Advantages of prostate cancer treatment at Euroonco
The main differences of Euroonko:
- We always act in the interests of the patient. When a doctor chooses treatment methods, he strives to achieve maximum effect with minimal risks for the patient.
- At Euroonco, a team of doctors works with the patient: a clinical oncologist, urologist oncologist, chemotherapist, and radiation oncologist.
- Prostatectomy is a serious procedure. We care about the safety of patients, therefore, before surgery, a thorough examination is carried out, the patient is consulted by a therapist, neurologist, cardiologist, and anesthesiologist-resuscitator.
- Here you can get a second opinion from reputable doctors from Europe, Israel, and the USA.
- In Moscow and Krasnodar, we provide treatment for prostate cancer according to international protocols, in accordance with the principles of evidence-based medicine.
Patient reviews of prostate cancer treatment at Euroonco
I had been under observation at a local clinic for many years and was prepared for the fact that sooner or later I would be diagnosed with prostate cancer. My grandfather and father had it. They both did not die from it, but it’s still quite alarming. So, six months ago, tumor markers showed a tumor. I chose the clinic exclusively on the Internet, made a list of five, in my opinion, the best, and then called. In the end, I settled on Euroonco. When I arrived for the appointment, I immediately felt somehow calm. Avetis Agvanovich received me and explained my diagnosis, its prospects and methods of treatment very thoroughly and in detail. It is immediately clear that the specialist knows the question “excellently.” We did some tests and procedures. They haven't started cutting yet. Perhaps you won't have to. Now I am in complete control of the situation, I know exactly what is happening there, and most importantly, I know for sure that there is an excellent doctor who remembers me personally and is ready to respond at any necessary moment. Thank you, Avetis Agvanovich, and until the next inspection! Igor Andreevich Shch.
Book a consultation 24 hours a day
+7+7+78