Find out more about other diseases starting with the letter “F”: Phakomatoses; Phantom pain; Fibromyalgia; Focal cortical dysplasia; Focal epilepsy; Funicular myelosis.
Phakomatoses are a group of diseases caused by a genetic predisposition, characterized by a progressive course and having polymorphic symptoms, mainly affecting the nervous system and organs of vision. A distinctive symptom is the formation of tumors of internal organs.
The diagnosis is established after consultations with many specialized specialists, as well as on the basis of a comprehensive examination using MRI, CT, ultrasound, ECG, EEG, and ophthalmoscopy. Treatment of phakomatosis is aimed at eliminating symptoms, using psychotherapy and surgical treatment. The prognosis of the disease depends on its form and severity.
general information
At the end of the 19th century, clinical variants of phakomatoses were described by many doctors. In 1923, the Dutch ophthalmologist Van der Hoove proposed combining diseases with combined lesions of the nervous system, internal organs, and eyes, which are accompanied by skin manifestations in the form of hypo- and hyperpigmentation, neurofibroma, and angioma. Van der Hoeve introduced the definition of "phakomatosis".
In modern medicine, “phakomatosis” is not a nosological entity, but belongs to a certain group of diseases. The most common diseases in this nosological group are Recklinghausen's neurofibromatosis and tuberous sclerosis. This group includes almost 30 neurocutaneous syndromes - Louis-Bar, Hippel-Lindau, Bonnet-Dechaumes-Blanc, Sturge-Weber, Ito hypomelanosis, pigment incontinence syndrome.
Report on the topic “Phakomatoses”
Phakomatoses (phakos-spot) are diseases in which combined damage to the skin, nervous system and internal organs is observed. The following phakomatoses are distinguished: neurofibromatosis of Recklinghausen, tuberous sclerosis of Bourneville, encephalo-trigeminal angiomatosis of Sturge-Weber, ataxia-telangiectasia (Louis-Bar syndrome).
RECKLINGHAUSEN NEUROFIBROMATOSIS:
Recklinghausen's neurofibromatosis has been studied more than other phacomatoses, since it occurs most often. There are peripheral and central neurofibromatosis. In peripheral neurofibromatosis, the process involves peripheral nerves; in central neurofibromatosis, the process involves cranial nerves and the substance of the brain and spinal cord. It is inherited in an autosomal dominant manner, but many sporadic cases occur because the gene that determines this disease often mutates spontaneously. The peripheral form of neurofibromatosis is more common than the central form. It is characterized by a tetrad of symptoms: spots on the body resembling the color of coffee with milk, tumors of the skin and subcutaneous tissue, tumors of the nerve trunks and their endings, physical and mental disability.
Pigment spots are detected already at birth. They are usually found on hidden surfaces of the body. Skin tumors may manifest as local elephantiasis, multiple nodular formations, or massive pigmented skin growths. In the nodular form of neurofibromatosis, there may be from several to several thousand nodes on the body (81). Nerve tumors can be of different localizations; the nerves of the extremities are most often affected. Along the nerve trunks, single or multiple thickenings or diffuse thickenings of the peripheral nerves are noted. These nodes are painful if they come from sensory fibers, and painless if they come from motor fibers.
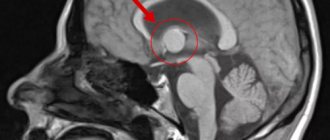
In central neurofibromatosis, tumors originate from cranial nerves, spinal roots, or the substance of the central nervous system. A common form of central neurofibromatosis are bilateral acoustic neuromas, multiple neuromas of the cauda equina roots and other nerves and roots. The central form of neurofibromatosis clinically manifests itself as a tumor of the brain or spinal cord, and only histological examination helps to establish the true nature of the process. Neurofibromatosis is often combined with other tumors - arachnoidendotheliomas, ependymomas, astrocytomas, spongioblastomas, etc. Both their own nerve fibers and connective tissue elements of the endo- and perineurium take part in the development of neurofibromatosis tissues. In central neurofibromatosis, accumulations of nodules of dysplastic giant glial cells are often found in the cerebral cortex, as well as in the white matter. The presence of these atypia brings Recklinghausen's disease closer to Bourneville's tuberous sclerosis.
See also: Report on the topic “Pulpitis”
With neurofibromatosis, a number of malformations of various organs (eyes, ears, nose, dentofacial apparatus) are observed.
Treatment of patients is surgical for a small number of nodes, as well as in cases of compression of vital formations by the tumor.
ENCEPHALOTRIGEMINAL ANGIOMATOSIS OF STURGE-WOBER:
The classic manifestation of the disease is characterized by a triad of symptoms: vascular spots on the skin of the face (angiomas), seizures, increased intraocular pressure (glaucoma).
The pathology is often familial and inherited in an autosomal dominant manner, but autosomal recessive forms also occur.
Order work from 200 rubles
If you need help with your work, we recommend turning to professionals. More than 70,000 experts are ready to help you right now.
Find out the cost
Pathomorphological examination of patients suffering from encephalotrigeminal angiomatosis reveals proliferation of blood vessels in the skin, pia mater, and choroid plexuses of the eyeball. Less commonly, angiomas are located in the occipital region of the cerebral hemispheres, cerebellum, spinal cord and internal organs. They describe the deposition of calcium salts in the vessels of the brain—petrificates. The severity of angiomas can vary significantly.
Angiomas on the skin usually appear already at birth and have the appearance of a “flaming spot” (Fig. 86). In 80% of cases they are located on the face (on one or both sides) in the area of innervation of the branches of the trigeminal nerve. Convulsive seizures appear in the first years of life and are usually focal in nature. In many patients they end in a generalized convulsive seizure. Nonconvulsive attacks in the form of instantaneous blackouts, shuddering, and freezing are possible. Some patients have severe headaches with vomiting (migraine-like attacks).
Increased intraocular pressure (glaucoma) is observed from birth or appears later. The progression of glaucoma leads to decreased vision up to complete blindness.
Among other manifestations of the disease, dementia is very common, which is caused by repeated attacks. Dementia is combined with pronounced changes in the emotional-volitional sphere: rancor, egocentrism, affectivity, vindictiveness. Patients' memory, attention, and ability to assimilate new information deteriorate; these factors significantly
complicate the process of training and education. These mental disorders are also observed in the period between attacks. The severity of intellectual disorders, especially memory, increases as seizures become more frequent. Among the mentally retarded, the incidence of Sturge-Weber disease is 0.1%.
See also: Report on the topic “Cellulite and some methods of body correction”
The diagnosis of encephalotrigeminal angiomatosis is confirmed by examining intraocular pressure, the fundus, radiography of the skull and recording of brain biocurrents.
During the treatment of the disease, anticonvulsants and psychotropic drugs are used, as well as drugs that reduce intracranial and intraocular pressure. X-ray therapy and (if indicated) neurosurgical treatment methods are used.
Order work from 200 rubles
If you need help with your work, we recommend turning to professionals. More than 70,000 experts are ready to help you right now.
Find out the cost
Children with a monosymptomatic form of encephalotrigeminal angiomatosis, having only a cosmetic defect in the form of glowing spots on the face, are educated in a public school. In these cases, the teacher needs to teach other children not to notice the cosmetic defect their sick friend has. Otherwise, psychopathological character traits may arise and develop in a sick child.
When teaching children with encephalotrigeminal angiomatosis, great difficulties may arise due to the increase in psychopathological changes and dementia due to the progression of the main pathological process.
With this rare form of phakomatosis, neurological symptoms, skin manifestations in the form of spider-like proliferation of blood vessels (telangiectasia), and a decrease in the immunological reactivity of the body are observed. The disease is genetically determined; inherited in an autosomal recessive manner.
A pathological examination of patients suffering from ataxia-telangiectasia revealed a decrease in the number of nerve cells and proliferation of blood vessels in the cerebellum.
The first signs of the disease appear between the ages of one and four years. The gait becomes unstable, awkward movements appear, and the fluency of speech (chanted speech) is disrupted. The progression of cerebellar disorders gradually leads to the fact that patients stop walking independently. Involuntary movements of the limbs are often observed, and poor facial expressions are noted. Speech is monotonous and poorly modulated.
Another characteristic sign of the disease is vascular changes in the form of telangiectasia, located on the mucous membrane of the eyes, mouth, soft and hard palate, and skin of the extremities. Telangiectasia usually appears after ataxia, but can also be the first symptom of the disease (Fig. 87).
Children with ataxia-telangiectasia often suffer from colds, inflammation of the paranasal sinuses, and pneumonia. These diseases often recur and take a chronic course. They are caused by a decrease in the protective immunological properties of blood and the absence of specific antibodies.
Order work from 200 rubles
If you need help with your work, we recommend turning to professionals. More than 70,000 experts are ready to help you right now.
Find out the cost
See also: Report on the topic “Visceral syphilis”
As the disease progresses, intellectual impairment increases, attention and memory become impaired, and the ability to abstraction decreases. Children become exhausted quickly. There are sudden changes in mood. Tearfulness and irritability are replaced by euphoria and foolishness. Patients are sometimes aggressive. They lack a critical attitude towards their own defect.
During the treatment of ataxia-telangiectasia, general restoratives and drugs that improve the functionality of the nervous system are used. Attempts are being made to replace the missing immunological blood fractions by transplanting a thymus gland taken from a deceased newborn and introducing an extract of the thymus gland - thymosin.
Therapeutic and pedagogical measures are very limited due to frequent colds and the steady progression of the process, leading to severe intellectual impairment.
HOPPEL-LINDAU DISEASE:
Cerebroretinal angiomatosis is a combination of angioblastoma of the brain (usually the cerebellum) with angiomatosis of the retina. This may be accompanied by pancreatic cysts, kidney cysts or tumors, and polycythemia. If angioblastoma is removed in a timely manner, the prognosis is favorable.
BOURNEVILLE DISEASE:
Tuberous sclerosis is a tumor-like growth of glia found in childhood. The triad is characteristic: progressive dementia, seizures and pigmented adenomas of the sebaceous glands of the face. Tumors of the heart, kidneys, lungs, and periventricular calcifications are common. The prognosis is unfavorable.
Average rating / 5. Number of ratings:
We're sorry you gave it a low rating!
Let us become better!
Tell us how we can improve?
Reasons for the development of phakomatosis
Phakomatosis is a genetic disease during which, starting from the early embryonic period, disorders occur in the processes of cell differentiation and development. Pathologies develop preferentially in the ectodermal germ layer, from which nerve fibers, outer layers of skin, nails, hair, retina, and epithelium of the oral and nasal mucosa develop. What remains are cells that have stopped developing and remain at the stage of permanent embryonication. From these tumors begin to form - hamartomas. Tumors of embryonic origin can be localized in different places and accompany phakomatosis of any nature.
Pediatricians and neurologists often define phakomatosis as neurodermal dysplasia, based on data on the pathology of the formation of ectodermal structures. It should be noted that in phakomatosis, ectodermal dysplasia is often combined with pathologies of differentiation of the mesodermal and ectodermal germ layers.
Mesodermal dysplasia leads to the formation of aneurysm, angioma, rhabdomyoma, and bone tissue pathologies. Clinical signs of ectodermal dysplasia include polyps of the gastrointestinal tract - stomach polyps, rectal polyps, intestinal polyps.
The progress of DNA methods and genetics has made it possible to identify genes in which deviations from the norm explain phakomatosis. Genetic changes lead to a decrease in the synthesis of factors responsible for blocking tumorigenesis. This is the most likely reason for the formation of multiple tumors that characterize phakomatoses. Inheritance occurs according to an autosomal dominant trait with incomplete penetrance, which explains the fact that the disease is not recorded in every generation.
What diseases are classified as phakomatoses?
The most common phakomatoses include diseases such as:
- neurofibromatosis type I (Recklinghausen's disease);
- neurofibromatosis type II (bilateral acoustic neuroma);
- tuberous sclerosis (Bourneville-Pringle disease);
- Sturge-Weber syndrome (encephalotrigeminal angiomatosis);
- Klippel-Trenaunay-Weber syndrome (hypertrophic hemangiectasia);
- ataxia-telangiectasia (Louis-Bar syndrome);
- Hippel-Lindau disease (retinocerebrovisceral angiomatosis);
- Osler-Rendu-Weber disease (hereditary hemorrhagic telangiectasia);
- Ito hypomelanosis;
- pigment incontinence (Bloch-Sulzberger syndrome);
- albinism.
Clinic of phakomatosis
Polymorphic damage to the skin, nervous system, and internal organs is a characteristic sign of phakomatosis. Signs of neurological and dermatological syndromes appear in early childhood, as they are congenital. Much later other signs appear. In some clinical cases, phakomatosis occurs against the background of congenital immunodeficiency, combined with premature aging and the risk of developing cancer.
Lesions of the nervous system are expressed in formations in the medulla and membranes. Most often, cysts, subependymal nodes, neurofibromas, calcifications, and areas of atrophy or demyelination appear. The patient is diagnosed with congenital anomalies of the cerebral vessels - aneurysms, angiomas. Often a convulsive syndrome appears with various forms of attacks.
West syndrome is recorded in early childhood. Older children experience generalized and partial sensorimotor epileptic seizures, and Lennox-Gastaut syndrome manifests itself. Epileptic seizures and disorders of brain structures lead to mental retardation, speech disorders, mental retardation, and abnormal behavior. The degree of mental retardation is related to the frequency and severity of epileptic seizures and can vary from debility to idiocy.
Patients experience disorders in the functioning of the cranial nerves - oculomotor disorders, hearing pathologies, paresis of the facial nerve. There are signs of cerebellar ataxia, sleep disorganization in the form of insomnia or somnambulism. From the extrapyramidal areas - tonic muscle symptoms, hyperkinesia, bradykinesia. The patient's behavior is disrupted until the development of ADHD or autism.
Metamorphoses of the skin with phakomatoses appear in the first months of life. The spots on the skin are asymmetrical, can have different colors, sizes, single or multiple. Patients most often experience age spots, dermatofibromas, areas of reduced pigmentation, papillomas, angiomas, and shagreen plaques.
The phenomena of phakomatosis are accompanied by disorders of the endocrine system in the form of diabetes insipidus, hypothyroidism, and obesity. Children experience delayed or early puberty, and on the part of the autonomic nervous system - trophic disorders in the form of brittle nails, dry skin, and hair loss. Ophthalmologists detect damage to the visual organs of congenital origin or early manifestation. During the examination, angiomatosis, retinal hamartomas, and conjunctival telangiectasia are detected. There is a decrease in the quality of vision.
On the part of the internal organs, the development of neoplasms is noted. Most often, tumors are benign in origin, but they can recur and progress. Children suffering from phakomatosis are more prone to infectious diseases than others, which lead to complications from the underlying disease.
PHACOMATOSES
PHACOMATOSES
(phacomatosis, singular; Greek phakos lentil, birthmark + -oma + -osis) are hereditary, progressive diseases characterized by combined damage to the skin, eyes, nervous system and internal organs.
The term “phakomatoses” was first introduced in 1923 by J. van der Hoeve, who proposed combining into one group congenital and hereditary diseases with skin changes in the form of hyperpigmented and hypopigmented spots, angiomas, neurofibromas, combined with damage to the eyes, nervous system systems and often internal organs.
Phakomatosis with damage to the nervous system currently includes encephalotrigeminal angiomatosis Sturge-Weber-Krabbe-Dimitri (see Encephalotrigeminal angiomatosis), cerebroretinovisceral angiomatosis Hippel-Lindau (see Hippel-Lindau disease), ataxia-telangiectasia Louis-Bar (see Ataxia ), hypertrophic Klippel-Trenaunay hemangiectasia (see Blood vessels), Bourneville-Pringle tuberous sclerosis (see Tuberous sclerosis), Recklinghausen neurofibromatosis (see Neurofibromatosis), retino-optic-mesencephalic angiomatosis - Bonnet-Dechaumes-Blanc syndrome, cortico- meningeal diffuse Van Bogaert-Divry angiomatosis and some other forms that are very rare.
Phakomatoses develop in early childhood and are sometimes detected at birth.
In the development of phakomatosis, genetic factors play a large role; Often there are familial forms of the disease that can be traced through several generations. Phakomatoses are inherited mainly in an autosomal dominant manner, less often in an autosomal recessive manner with incomplete penetrance of the mutant gene (see Gene). Penetrance of the gene (see) in some phakomatoses reaches 75-90%. The twin method (see) of research reveals a high concordance of systemic lesions of the skin of the eyes and nervous system in monozygotic twins.
It is assumed that the diseases that make up the phakomatosis group are based on genetically determined disorders of the development of germ cells, leading to ectomesodermal dysplasia with the formation of angiomas, telangiectasia, neurofibromas on the skin and in various parts of the nervous system - the brain, brain stem, cerebellum, spinal cord brain, peripheral nerves, as well as aneurysmal angiomas of the retina, etc. In some forms of phakomatosis (for example, ataxia-telangiectasia), congenital immunodeficiency is found (see Immunological deficiency) with an increased risk of malignant tumors and premature aging syndrome. These forms are classified as diseases associated with impaired DNA repair.
Morphological changes depend on the form of phakomatosis. Along with the morphological components characteristic of various forms of phakomatosis - angiomas, angioreticulomas, aneurysms, arteriovenous malformations, tuberous formations, neurofibromas, cystic formations, petrificates in the meninges, brain and spinal cord - hydrocephalus (see) with dilatation of the ventricles of the brain is detected, atrophy of various parts of the brain and cerebellum, demyelination, gliosis, often various malformations of the brain and eyes, pathology of internal organs (kidney cysts, pancreas, etc.).
Damage to the nervous system is manifested primarily by epileptic seizures (see Epilepsy). Partial or generalized epileptic seizures (usually mixed types) occur. Generalized grand mal seizures (tonic or clonic-tonic) are usually accompanied by loss of consciousness; partial seizures often occur without loss of consciousness in the form of motor, sensory or combined Jacksonian seizures. Convulsive seizures, which initially occur as partial ones, can later transform into generalized large ones. Periods of status epilepticus are often observed. Early symptoms also include delayed mental development and speech development, and behavioral disorders. The decline in intelligence reaches the level of imbecility and idiocy (see Mental retardation). There is a clear correlation between the degree of mental degradation, the severity and frequency of development of status epilepticus. The examination reveals symptoms of damage to the cranial nerves (usually oculomotor, facial), pyramidal symptoms (hemiparesis, hemiplegia), extrapyramidal disorders (hyperkinesis, athetosis, less often - parkinsonism with hypokinesia, oligokinesia, bradykinesia, changes in muscle tone), cerebellar disorders ( ataxia, intention tremor, nystagmus). Along with this, hypothalamic vegetative-trophic disorders (dry skin, acrocyanosis, brittle nails, hair loss), endocrine metabolic disorders (obesity, premature or, conversely, delayed puberty, hyper- or hypothyroidism, diabetes insipidus, etc.) may occur. .).
Skin lesions are noted at birth or in the first months of life. On the skin of the face, torso, and limbs, angiomas are found (see Angioma), angiofibromas (see), telangiectasia (see), single or multiple, different in color, size, distribution. Along with this, café-au-lait areas of hypopigmentation are observed on the skin. Skin lesions can cover one half of the body or be diffuse, combined with cavernous angiomas on the mucous membranes (see Encephalotrigeminal angiomatosis), with adenomas of the sebaceous glands (see). There is no correlation between the skin manifestations of phakomatosis and damage to the nervous system. There is often a tendency for pathological formations on the skin to progress and become malignant. In patients with phakomatosis, dysembryogenetic changes in the bone and vascular systems are often observed. Characteristic of certain nosological forms included in the phakomatosis group, eye changes can be congenital or develop in the first years of a child’s life. In the fundus, limited or diffuse angiomatosis, ampulla-shaped dilations of blood vessels are detected (see Hippel-Lindau disease), tumor-like tuberous yellow formations along the periphery of the fundus or in the area of the optic nerve head (see Tuberous sclerosis). Along with this, bright red telangiectasias may be observed on the scleral conjunctiva. Progression of pathol. changes in the eyes lead to decreased vision or blindness.
The course of phakomatosis is progressive. The severity of central paresis, epileptic seizures, and mental disorders gradually increases. Neuropsychic and speech disorders progress especially quickly during puberty. Latent, compensated forms of phakomatosis when exposed to unfavorable environmental factors, infectious diseases, injuries can turn into a clinically pronounced and rapidly progressing process.
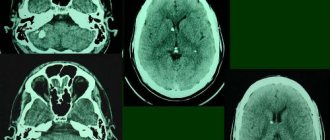
The diagnosis is made on the basis of the clinical picture - a combination of epileptic seizures of a polymorphic nature, mental retardation, delayed development of motor and speech functions with characteristic skin changes (presence of spots with altered pigmentation, angiomas, neurofibromas on the face, limbs, torso), specific changes in the fundus , focal neurological symptoms. X-ray examination of the skull plays an important role in early diagnosis. During craniography (see), petrificates are found in various structures of the brain; using pneumoencephalography (see) detect enlargement of the ventricles of the brain, signs of intracranial hypertension (see Hydrocephalus); computed tomography (see Computer tomography) allows you to diagnose angiomas, neurofibromas, cystic and tumor-like formations, and brain atrophy. An electroencephalographic study reveals focal or diffuse changes in bioelectrical activity of an epileptic nature (see Electroencephalography). Cerebrospinal fluid is usually unchanged.
Differential diagnosis is carried out with malformations of the central nervous system, in contrast to which, with phakomatosis, there is a progression of the process with an increase in neuropsychic disorders.
Treatment is symptomatic. Anticonvulsants, dehydrating drugs, drugs that improve trophic functions and metabolism (amino acids, vitamins), etc. are prescribed. For single superficial angiomas of the meninges, radiation therapy is used (see), surgical treatment is less often performed. For isolated skin angiomas, cryosurgery (see), surgical treatment is used; for retinal angioreticulomas, laser treatment (see), etc.
The prognosis is unfavorable. A negative factor that complicates the course of the disease and often leads to the death of patients are infectious diseases and injuries. Edema and swelling of the brain (see) with status epilepticus can lead to death. In some forms of phakomatosis, the outcome of the disease is associated with the development of a malignant tumor.
Medical genetic counseling is of preventive importance, in which it is recommended to limit childbearing in families with established cases of phakomatoses (see Medical genetic consultation).
Bibliography; Badalyan L. O., T and b o-lin V. A. and Veltishchev Yu. V. Hereditary diseases in children, p. 312, M., 1971; Differential diagnosis of skin diseases, ed. A. A. Studnitsina, p. 450, M., 1983; Kalinina L.V. and Gusev E.I. Hereditary diseases of metabolism and phakomatoses with damage to the nervous system, M., 1981; 6 und 1 a c h R. u. Ster n J.Das multilokulare Hamangioblastom mit zerebellarer und spinaler Beteiligung ais Manifestationsform des inkompletten von Hippel - Lindau - Syndroms, Neurochirurgia (Stuttg.), Bd 25, S. 124, 1982; Kingsley DPECAT in the phakomatoses, in: The first European seminar on computerized axial tomography in clinical practice, ed. by G. H. du Bou-lay a* I, F. Moseley, p. 174, B, aot 1977; Person JR a. R e g u N. O. Recent advances in the phakomatoses, Int. J. Derm., v. 17, p. 1, 1978; R i 1 ey FC a. Campbell RJ Double phakomatosis, Arch. Ophthal., v. 97, p. 518, 1979; Van der Hoeve J. Eine vierte Phakomatose, Ber. ophthalmic Ges., Bd 51, S. 136, 1936. JI. V. Kalinina.
Diagnosis of the disease
The variety of clinical symptoms and their manifestations at different ages make it somewhat difficult to make a correct diagnosis. For a correct conclusion, you should consult a neurologist, pediatrician, ophthalmologist, dermatologist, cardiologist, nephrologist, geneticist, endocrinologist. A biochemical examination of blood and urine, genetic analysis, DNA examination, and examination of the neuropsychological state are prescribed.
Hardware methods include:
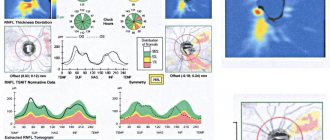
- electroencephalography - reveals the nature of epileptic activity of the brain;
- Echo-EG - detects hydrocephalus;
- MRI, CT - provide information about changes in brain tissue;
- cerebral angiography - abnormalities in the development of cerebral vessels;
- ophthalmoscopy - reveals vision pathologies, even without an obvious clinical picture;
- ECG, ultrasound of the heart - to determine cardiac changes.
If other types of pathology are suspected, ultrasound of the abdominal cavity, radiography of the stomach, examination of the intestines using a contrast agent, ultrasound of the kidneys, and urography are prescribed.
Diagnostics
To diagnose phakomatosis in children, you should first consult a pediatrician; in older people, you should consult your general practitioner. The doctor will refer the patient for consultation to a number of specialized specialists: ophthalmologist, neurologist, dermatologist, nephrologist, cardiologist, gastroenterologist, endocrinologist. Also, due to the hereditary nature of the disease, a geneticist’s opinion will be required. The full list of specialist doctors depends on the manifestations of the disease.
After studying the patient’s complaints, clinical picture, and medical history, the patient can be sent for a number of examinations:
- blood chemistry;
- general blood analysis;
- general urine analysis;
- genetic testing;
- electroencephalography (EEG);
- electrocardiogram (ECG);
- magnetic resonance imaging (MRI);
- CT scan ();
- ophthalmoscopy;
- ultrasound examination (ultrasound) of the brain and internal organs;
- angiography;
- echocardiography.
Diagnosis is complicated by the variety of clinical manifestations in different forms and at different ages. However, the examination data collected together will be able to give doctors the basis for the main conclusion: whether the patient has phakomatosis or not.
Treatment of phakomatosis
Specific therapy for phakomatoses has not been developed. Treatment is aimed at eliminating symptoms. In accordance with the clinical manifestations, anticonvulsants, dehydrating, and neurometabolic drugs are prescribed. Epileptic seizures can be very resistant to anticonvulsants, which requires a change in drug or a combination of two drugs. Stimulating neurometabolites are not prescribed in the presence of epileptic episodes, as they have an exciting effect.
Surgical intervention is performed in the presence of malignant neoplasms. The operation is performed when the tumor is actively growing and there are signs of compression. Neurosurgical operations are performed when intracerebral formations are detected.
Patients are required to undergo psychocorrection aimed at stimulating the child’s mental and mental qualities, his learning and social adaptation. It is advisable to conduct classes with a child psychologist, play therapy, and neuropsychological correction. Psychological counseling of parents is mandatory.
Forecast and prevention of phakomatosis
Phakomatoses in most clinical cases are diseases that have an unfavorable prognosis. The form of the disease, the age of the child at which the diagnosis was first made, and the severity of clinical symptoms have an impact on the final outcome of the disease. An infectious disease or injury can complicate the course of the disease.
Early manifestation of phakomatosis, severe course of epileptic seizures, severe mental retardation, the appearance of malignant tumors - all this significantly aggravates the prognosis of the disease. The patient may die from cerebral edema during an epileptic attack, cachexia in severe cancer, or sepsis.
Preventing the birth of a sick child is the main way to prevent the development of phakomatosis. Parents planning to have a child should undergo genetic counseling.