Magnetic resonance imaging allows you to assess the condition of internal structures, including elements of the central (CNS) and peripheral (PNS) nervous systems, in a painless and safe way for the patient. MRI of the brain for vasoneural conflict makes it possible to diagnose disorders and identify the causes of pathological changes.
The method is based on the phenomenon of magnetic resonance, the essence of which is the vibration of hydrogen nuclei in response to the influence of an induction field. Under the influence of a directed high-frequency pulse, water molecules contained in the cells provide a response. Sensitive sensors installed on the tomograph read information received on the computer monitor in the form of monochrome photographs of thin sections of the scanned area.
MRI images of the brain for suspected vasoneural conflict (axial section)
The study is more informative regarding fluid-saturated loose structures. MRI of the brain and nerve trunks visualizes the condition of the area being studied and the structure of the surrounding anatomical formations.
Why does vasorenal conflict occur?
Vasorenal conflict refers to the presence of an additional renal artery or an abnormal passage of its branch. This leads to compression of the ureter and difficulty in the outflow of urine, which provokes expansion of the pelvis. Vasorenal conflict can be congenital or acquired. In the first case, the causes of pathology are:
- fibromuscular dysplasia;
- aneurysm of arteries in the kidneys;
- renal artery hypoplasia;
- vascular fistulas;
- extravasal compression of the renal arteries.
Vasorenal conflict can occur against the background of thrombosis and embolism of the renal artery, neoplasms in the kidneys, and vascular sclerosis. Of the acquired diseases, the causes of pathology are:
- dissecting aortic aneurysm;
- nephroptosis;
- glomerulonephritis;
- pyelonephritis;
- systemic vasculitis;
- Takayasu's disease;
- malignant neoplasms;
- atherosclerosis;
- urolithiasis disease;
- traumatic aneurysm of the renal artery;
- kidney infarction.
How does vasoneural conflict occur?
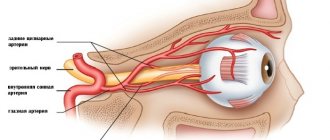
There are frequent cases when a vasoneural conflict occurs when the cerebellar artery pulsates, which passes to the trigeminal nerve. When the heart contracts, blood begins to move through the vessels. Blood flow creates a pulsation in their walls. As a result, there is compression of the nearby nerve.
The result of constant compression of pulse oscillations on the nerve area next to which the vessel passes is its demyelination. The nerve loses its myelin sheath (which is normally present). Due to the sheath, information is transmitted along the nerve processes (also a pain signal), when it is destroyed, the person suffers from trigeminal neuralgia. It is for this reason that with vasoneural conflict the appearance of this syndrome is observed.
Symptoms of the disease
Please note that 25% of patients with renovascular hypertension are asymptomatic. Due to the nonspecificity of symptoms, doctors face a number of difficulties when making a diagnosis. The main symptoms of renovascular hypertension:
- pain in the eyeballs;
- heaviness in the head;
- headache;
- noise in ears;
- muscle weakness;
- memory impairment;
- heartbeat disturbance;
- pain in the heart area;
- pain and heaviness in the lumbar region;
- heaviness in the chest.
Main feature
The main and often the only symptom of the disease is arterial hypertension syndrome. Its course may be no different from essential hypertension. Renal hypertension causes a persistent increase in systolic and especially diastolic blood pressure. The difference between the two indicators will always be small.
An increase in blood pressure in childhood, adolescence and young adulthood – up to 30 years – should alert you. There is a high risk of developing fibromuscular dysplasia. Patients over 45 years of age are characterized by atherosclerotic damage to the renal arteries. You should pay attention to the following symptoms of arterial hypertension:
- resistance to prescribed treatment;
- increased diastolic pressure;
- rapid damage to internal organs.
Trigeminal neuralgia
What are the symptoms?
- pain appears in the innervation area (the place where the processes of the trigeminal nerve pass through the tissues and receive signals from the branches of the trigeminal nerve). Usually this is one of the two halves of the face,
- the pain syndrome comes on suddenly,
- in 80 out of 100 cases, the pain disappears in unexpected attacks and does not bother you for some period of time, in 20 cases it becomes constant;
- an attack of pain can last a few seconds or last for minutes;
- the part of the face affected by the pathology may involuntarily twitch during pain symptoms due to muscle contractions, the skin is sometimes redder, tears flow from the eyes, and salivation increases;
- the patient places his hand on the painful area and tries to breathe less slowly;
- as soon as the attack passes, painful points are felt in the place where the nerve enters the facial surface.
Factors contributing to the occurrence of pain attacks:
- Prolonged exposure to the cold, leading to hypothermia;
- Migraine attacks;
- Nervous tension;
- Chewing;
- Some foods can cause an attack (alcoholic drinks);
- Talk;
- Sanitation of the oral cavity with a brush.
Other causes of neuralgia:
- The nerve is destroyed (occurs with multiple sclerosis);
- Compression of the nerve process by a neoplasm from the outside;
- Neuroma (type of tumor);
- Bruises and fractures of the skull bones;
- Diseases of an infectious nature.
How are inflammation of the trigeminal nerve and trigeminal neuralgia related?
Neuritis (the process of inflammation) is a pathology that results from the spread of an inflammatory reaction from nearby organs (during caries, sinusitis) or the penetration of infection through the blood. Infectious damage to the nerve process ends with the myelin sheath becoming thinner, and symptoms of trigeminal neuralgia appear.
The exit site of the trigeminal nerve is circled; the MRI image shows a large vessel causing compression of the nerve.
Trigeminal nerve inflammation on MRI
MRI images will show both demyelination of the fibers and inflammatory diseases that led to the development of neuritis: the presence of exudate in the sinuses, an edematous process in the middle and inner part of the ear.
Treatment methods
- if surgical treatment is not possible;
- as an addition to surgery if it does not lead to a decrease in pressure;
- with a persistent increase in blood pressure.
Even if medications have been able to reduce blood pressure, if renal artery stenosis persists, the blood supply is disrupted even more. As a result, the patient may experience shrinkage of the kidney, which completely loses its function.
Maintenance therapy
Since conservative methods are ineffective as an independent method of treating renovascular hypertension, they are used as maintenance therapy. Its scheme includes the following activities:
- Normalization of body weight. Obesity provokes kidney and vascular diseases, as well as increased blood pressure.
- Rejection of bad habits. It is necessary to exclude smoking and alcohol.
- Active lifestyle. The patient is advised to exercise moderately.
- Proper nutrition. Fried and fatty foods, foods with stabilizers, salt, dyes, high levels of sugar, and flavor enhancers are excluded from the diet.
At the preoperative stage or in persons who cannot undergo surgery, drug treatment is carried out. The main groups of drugs used:
Angiotensin-converting enzyme inhibitors
Calcium channel antagonists
Surgical intervention
Stenosis of the renal arteries, which provoked an increase in blood pressure, can only be eliminated surgically. The main types of operations performed for renovascular hypertension:
What does MRI show in neurovascular conflict?
Magnetic resonance imaging visualizes the location and condition of intracranial structures, allowing the identification of pathological lesions of small diameter. Scanning is carried out in three mutually perpendicular projections. Layer-by-layer images show alternating light and dark areas, the contours of which correspond to the boundaries of the anatomical formations.
Using the obtained images, a 3D model of the studied area is reconstructed. The three-dimensional projection visualizes the brain stem, nerve roots, blood vessels and formations located nearby.
MRI is the most effective type of diagnostics of neurovascular conflict. Axonal fibers have an average signal intensity on T1- and T2-weighted images; to confirm the disease, scanning in a special mode with fat suppression is often used.
Tomograms reflect changes in the topography of cranial nerves, vascular pathologies and neoplasms. MRI shows signs of root compression; the images show areas of demyelination of fibers in places of compression.
Facial nerve compression on MRI
In the study protocol, the doctor indicates:
- condition of the bone canal;
- the presence of pathologically altered areas of the roots of the cranial nerves in the area of the branch from the trunk of the brain;
- condition of surrounding tissues;
- the presence of inflammatory, degenerative, neoplastic processes in the area under consideration;
- type, location, condition of adjacent veins and arteries.
MRI shows the extent of damage to the nervous tissue, reveals the etiology of the disease and helps to choose an effective treatment method.
MRI diagnostics
The reference method for making a diagnosis in modern medicine is considered to be magnetic resonance imaging (MRI) of vasoneural conflict.
The essence of this method is based on the principle of nuclear magnetic resonance. The magnetic field that is created inside the tomograph picks up impulses from hydrogen ions, which are found in all tissues of the body. These impulses are read by the device, and a highly accurate image of the internal organs becomes visible on the computer.
In the case of neurovascular conflict, MRI will help determine the exact cause of nerve compression. This is also necessary before surgery to adequately assess its effectiveness.
Whatever artery causes nerve compression, early MRI diagnosis makes it possible to prescribe effective treatment in a timely manner.
Facial nerve damage
The symptoms of vasoneural conflict of the facial nerve are fundamentally different from those of the trigeminal nerve. This is due to the fact that the facial nerve performs a motor function, unlike the sensory trigeminal nerve. Therefore, the disorders will be primarily motor.
The main clinical manifestation is involuntary movements of the facial muscles. It is characteristic that involuntary contractions of the orbicularis oculi muscle begin first, which eventually spread to the entire half of the face. The other side remains unaffected. If left untreated, contractions become so frequent that the patient cannot see on the affected side.
There are also atypical forms of the disease. In such cases, involuntary contractions begin from the muscles of the cheek, and then rise upward.
In severe cases, attacks occur even during sleep. They become more frequent after overwork, stress, and anxiety.
Neurovascular conflict of the facial nerve can develop due to the following vessels:
- superior and inferior cerebellar arteries;
- vertebral artery;
- main artery;
- multiple exposure to several vessels at once.
Hemispasm should be distinguished from other conditions that are similar in their manifestations:
- tic - a spasm of the facial muscles of a psychological nature;
- facial myokymia - contractions of individual bundles of muscle fibers;
- Facial nerve paresis - disruption of its function due to injury, inflammation;
- tardive dyskinesia is a condition that occurs after taking antipsychotic medications.
What nerves can be affected?
In everyday life, you most often hear about vasoneural conflict of the trigeminal or facial nerve. The latter condition is also called hemifacial spasm, which literally means “spasm of half the face.” But this pathology can spread to other nerves, including:
- auditory or vestibulocochlear nerve;
- glossopharyngeal nerve;
- oculomotor nerve.