There are many structural elements inside the human eye. There are possible diseases in which this integrity is disrupted.
To determine the disorder, the doctor performs an ophthalmoscopy of the fundus.
This is the most common procedure for the visual organs after the use of diagnostic tables. The technique allows not only to identify the condition of the eyes, but also to determine the presence of a systemic disease. It is performed by an ophthalmologist after preliminary preparation of the patient.
Indications
More often, the technique is carried out for a preventive examination of the patient’s visual organs. But with its help it is possible to identify various diseases in the early stages. It is recommended to carry out the procedure for children, since at an early age it is possible to completely eliminate disorders in the early stages.
Additional indications for the procedure:
- suspicion of myopia, when the patient sees poorly in the distance, but well near, the doctor determines the cause of this disorder;
- suspicion of farsightedness, when the patient sees well near, but poorly in the distance, the doctor identifies the true cause of the condition;
- the presence of pathology of the optic nerve (compression, mechanical damage, impaired nutrition through blood vessels);
- pathology of the retina (compression by the internal structures of the eyes, detachment, thinning, mechanical damage, impaired nutrition through blood vessels);
- glaucoma - increased intraocular pressure due to increased secretion of intraocular fluid, the chambers of the eyes gradually grow, squeezing neighboring elements;
- cataract – clouding of the lens due to the accumulation of insoluble protein fractions in its internal structure;
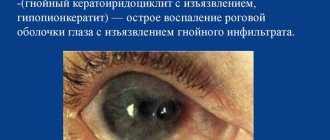
- infectious and inflammatory conditions of the inner part of the eyeball;
- macular degeneration;
- foreign body;
- malignant, benign tumors;
- disruption of blood flow through the vessels, as a result of which the eye tissues cease to receive nutrients and oxygen, necrosis (areas of necrosis) is formed;
- atherosclerosis, in which the microcirculation vessels of the eyes become clogged with cholesterol plaques;
- hypertension, due to which the pressure on the microcirculation vessels increases, their wall can rupture, causing hemorrhage;
- diabetic retinopathy is the formation in the blood of conglomerates consisting of glucose and cholesterol, spreading through the microcirculation vessels, including the eye, causing blockage.
To make a reliable diagnosis, the doctor needs to identify the first causes of the disease. Otherwise, the treatment provided will only be symptomatic and will not completely eliminate the disorder.
When is ophthalmoscopy prescribed?
This research method is the most common in ophthalmology. It is carried out using an ophthalmoscope - a special device that allows you to examine in detail the internal structures of the eye: the retina, vitreous body, optic disc, blood vessels, as well as the peripheral parts of the eyeball. Thanks to ophthalmoscopy, it is possible to identify severe pathologies of the visual organs at the very beginning of development. Among them:
- cataract;
- neoplasms;
- damage to the optic nerve;
- retinal detachment;
- glaucoma;
- macular degeneration;
- melanoma;
- cytomegalovirus retinitis;
- pathology of the blood vessels of the eyes.
Moreover, during an examination with an ophthalmoscope, not only ophthalmological diseases can be detected, but also diseases of a systemic nature, including diabetes mellitus, hypertension, renal failure, and tuberculosis.
Ophthalmoscopy is prescribed for every visual examination. It can be considered a standard procedure that is included in any examination by an ophthalmologist. A referral for an ophthalmoscopy can be given not only by an ophthalmologist, but also by a cardiologist, infectious diseases specialist, gynecologist, and therapist. This diagnostic method is very important for pregnant women. During pregnancy, patients with myopia have an increased risk of retinal detachment. With the help of an ophthalmoscope, this dangerous disease can be detected at a very early stage and laser coagulation can be prescribed.
The following diseases and symptoms may also be indications for ophthalmoscopy:
- color blindness;
- eyeball injuries;
- myopia;
- inflammatory processes in the eye;
- traumatic brain injury;
- headache;
- epilepsy;
- violation of movement coordination.
There are also a number of limitations to the purpose of this research method. It is not performed in case of increased photosensitivity, lacrimation, clouding of the optical media of the eye, miosis and other pathologies of the pupils. Under these conditions, it will be impossible to examine the fundus in detail. In addition, symptoms such as tearing and photophobia may increase. Ophthalmoscopy is not always prescribed for angle-closure glaucoma. There is a risk of increased intraocular pressure. The method is not used in the presence of cardiovascular diseases. Contraindications may include various infectious and inflammatory diseases of the anterior parts of the eye.
Contraindications
Some categories of patients are not recommended to undergo the procedure. To do this, the patient must have the following conditions and diseases:
- increased sensitivity to the action of bright light from a slit lamp, when spasm of the eyelids and increased lacrimation occur, which makes the examination impossible;
- lack of response to drugs that dilate the pupil;
- clouding of the lens, vitreous body, behind which it is impossible to recognize the structures of the fundus.
If there are contraindications, it is recommended to use other diagnostic methods to determine the condition of the patient's eyeballs.
Precautionary measures
It is important to note that the pupil after instillation of a mydriatic agent is not able to adequately respond to changes in light conditions for a certain period of time. In this regard, the patient has difficulties when he gets into a lit room or on the street. To cope with the discomfort that arises, you can use various means, for example, wearing dark glasses. Before the procedure of ophthalmoscopy with preliminary dilation of the pupil, you should ask your doctor about the duration of action of the medicine, as well as about eye protection measures for this period.
Types of ophthalmoscopy
There are different types of techniques. They differ in the equipment used to view the fundus. Each of them has its own advantages and disadvantages. The choice of procedure depends on the equipment of the ophthalmologist’s office and the suspicion of a certain eye pathology.
Straight
A regular ophthalmoscope is used, which the doctor sequentially brings to the patient’s eye until he sees all the insides of the eyeball. The disadvantage of the procedure is the need for patient assistance. He must consistently move his gaze to where the doctor says in order to examine the central and peripheral parts of the fundus of the eye.
Indirect
The ophthalmologist uses special instruments with which you can examine the entire fundus of the eye without the participation of the patient. To do this, he does not need to look in different directions. Using instruments, both central and peripheral areas are determined.
Vodovozov method
The doctor places colored filters on the ophthalmoscope, which are applied to the human eye. If normal lighting is used, it can diagnose early pathologies of the eyeball. When using a color filter, many pathologies of the eyeball will be visible that cannot be identified in daylight. For example, when using a yellow or green filter, slight bruising will be visible.
Fundus ophthalmoscopy - how is the procedure performed?
The first ophthalmoscope was created back in the 19th century. Since then, several methods of examining the fundus have been developed. Today, various types of devices are used: Goldmann lenses, electronic and laser, monocular and binocular. The two main types of ophthalmoscopy are direct and reverse (indirect). The first is carried out as follows. The ophthalmologist sits opposite the patient. The light beam is directed directly into the pupil. The doctor holds an ophthalmoscope in his right hand and brings it closer to the eye of the patient. The retina can be seen in detail from 3-4 cm. The image is magnified approximately 16 times. This procedure lasts no more than 10 minutes. Direct ophthalmoscopy requires instillation of mydriatic drops into the patient's eyes, which dilate the pupil. The technique is very accurate due to the strong magnification of the image. But it is not without its shortcomings. The picture is not very voluminous. It is not possible to study the periphery of the fundus. To do this, you need to resort to another method - reverse ophthalmoscopy. How is this procedure carried out?
The oculist holds an ophthalmoscope in his right hand near his eye. The light source is located behind the patient's back. A little to the left of him. The ophthalmologist holds a lens in his left hand. The distance from the cornea to the optical product is 5 or 7 cm, depending on the dioptres with which the lens is equipped. The doctor directs a beam of light into the patient's eye. It is reflected from the fundus of the eye and hits the lens. The stream of light rays is refracted and forms an image from the side of the ophthalmologist. It seems to hover in the air and represents a several times enlarged picture of the inside of the eye. The magnification here is not as strong as in direct ophthalmoscopy. But it is possible to quickly check the condition of not only the optic nerve head, blood vessels and arteries, but also the peripheral area.
In some cases, both reverse and direct ophthalmoscopy are performed. The first method helps to quickly identify the pathological process, and the second helps to find out details about the disease: the nature of development, stage, causes.
Preparation for ophthalmoscopy
2-3 days before the test, the doctor prescribes eye drops to the patient, with the help of which the pupil dilates. He temporarily loses accommodation when exposed to bright light. Atropine has been used previously, but it has many side effects and contraindications.
Therefore, it was replaced by more modern drugs.
During the use of eye drops, the patient's visual acuity decreases. Increased sensitivity to bright light occurs. Therefore, it is recommended to come to an appointment with an ophthalmologist with family or close friends to make it easier to get back home.
To ensure that there are no side effects or allergic reactions from using the drug, the doctor asks the patient’s medical history. He should tell his ophthalmologist about all the medications he is taking to avoid cross-drug interactions.
If a person develops glaucoma, that is, an increase in intraocular pressure, the doctor will advise not to use drops, but to undergo the procedure in a dark room with a natural reaction of the pupil.
Fundus examination in children
Fundus examination in children requires preparation. In order to be able to conduct ophthalmoscopy in young children, parents need to have a preparatory conversation with them. You will need to tell the child how the procedure will take place, what the doctor will do, explain that the examination will not cause pain to the baby and tell why it is necessary.
Children's eyes are constantly growing, and in order not to miss the disease, children undergo ophthalmoscopy more often than adults.
For newborns, this procedure can also be performed, but most often it is prescribed for suspected congenital pathologies: congenital cataracts, retinal dystrophy and others.
After ophthalmoscopy, newborns are often prescribed an ultrasound of the brain based on the results of the examination.
Features of the examination in children
Fundus examinations for young children and older children are carried out using the same method as for adults: in a dark room using a light source and an ophthalmoscope.
For particularly active young children, the doctor may use a toy (this distracts attention and forces the child to look in the right direction).
The examination of newborns follows the same scheme, with the active participation of the mother.
How is ophthalmoscopy performed?
To carry out the technique, the patient is placed in a dark room. This prevents increased eye tension during the examination. Next, the doctor conducts an analysis in several stages:
- a person sits on a chair, light from a slit lamp is directed into his eyes;
- using a special device according to the chosen method, the doctor examines the fundus of the eye;
- if direct ophthalmoscopy was chosen, the ophthalmologist asks the patient to look in different directions to diagnose the condition of the central and peripheral parts of the eyeball;
- with other methods, patient participation is not required;
- The doctor conducts the examination for 1-2 minutes, after which he writes down the results.
Based on the data obtained, the doctor can make a reliable diagnosis. If the results are incomplete, he will prescribe additional diagnostic tests, based on which he will identify the root cause of the violations.
Ophthalmochromoscopy - what is it and how is this procedure performed?
As noted earlier, the inside of the eye has a reddish tint. The optic disc, vessels, arteries, veins, and macula stand out against its background due to a lighter or darker color. Ophthalmochromoscopy is a direct method of examining the fundus of the eye using color filters that are mounted on an ophthalmoscope. This technique was developed by the Soviet ophthalmologist Vodovozov. It is more informative, as it allows you to see the most minor changes that cannot be detected using white light. During the procedure, the doctor can switch the color. For example, a green filter will show whether there is optic nerve atrophy, and if disc edema is suspected, a red filter is used.
Decoding the results
If a person is completely healthy, the doctor will see the following indicators of the fundus:
- blood vessels are intact and red;
- the structure of the retina is uniform, there are no breaks or thinning;
- a whole, uniform optic nerve disc is visible (its size and shape are determined);
- There should be no signs of inflammation or swelling of tissues.
The following disorders indicate pathology:
- cloudiness of the lens and vitreous body;
- increased amount of secretion in the chambers of the eyes;
- blockage of blood vessels, as a result of which blood does not flow to the tissues;
- hemorrhage (minor or significant);
- mechanical damage to various structures of the eyeball;
- displacement of the intraocular lens, if present;
- presence of a foreign body;
- proliferation of tissue indicating a tumor;
- retinal detachment;
- The optic disc is irregularly shaped and not fully attached to the retina.
By looking at the fundus of the eye, the doctor can assume the presence of cardiovascular diseases that the patient is not aware of. Therefore, using this method, it is possible to detect systemic diseases in a timely manner in order to prevent their complications.
Fundus of the eye - what is it?
This concept refers to the inner part of the eye with the retina, optic nerve head, blood vessels and periphery. Under an ophthalmoscope, a special instrument that is used to examine this area of the eyeball, you can see that the fundus of the eye has a reddish tint. In this case, the optic disc is pale pink, it stands out noticeably against the background of the overall reddish picture. At the very center of the disc are the central retinal vein and artery. They are divided into two branches - lower and upper, after which they diverge into many small branches that spread throughout the entire fundus of the eye. In the very center of the retina is the macula, or macula. Compared to other described structures, the macula has a darker color. Any changes in the color, shape, outline of the disc, macula, or retina may be a consequence of the development of a pathological process. It can be detected at an early stage through a detailed examination of the fundus. The procedure used to examine it is called ophthalmoscopy.
Possible complications during ophthalmoscopy
After the procedure, in rare cases, the patient sees spots, stripes, and lightning before his eyes. This is a temporary phenomenon that resolves within a few hours. After leaving the dark room, the patient is exposed to open rays of light. This causes pain, discomfort, and increased lacrimation. But in this case, sunglasses will help, which you must first take with you to eliminate complications from the procedure.
In rare cases, the following complications are possible:
- thirst, dry mouth due to the use of medicinal drops;
- swelling and redness of the skin around the eyes;
- temporary neurological disorders: nausea, vomiting, dizziness, headache.
Temporary deviations can be completely eliminated if you do not drip the medicine into your eyes.
What is the principle of ophthalmoscopy based on?
A ray of light penetrates the pupil and is refracted by the cornea and lens. It is projected on the retina. This method is used by an ophthalmologist to perform the ophthalmoscopy method. Since the pupil contracts excessively when exposed to bright light, this makes the examination difficult, and the field of the examined area will be insignificant. Therefore, atropine-like drugs are used to dilate the pupil. The ophthalmologist can completely examine the fundus, including the central and peripheral parts.
Indirect ophthalmoscopy
Reverse ophthalmoscopy is performed using a conventional lamp, which is located next to the patient, to the left and slightly behind his back. As a result of this arrangement, the subject finds himself in the shadow. There is no direct contact between the subject and the device. This is a non-contact ophthalmoscopy. The ophthalmologist sits opposite him at arm's length, brings the ophthalmoscope to his eye and directs a beam of light from the lamp, reflected from the mirror of the device, into the patient's eye. At this moment, you can notice that the pupil turns red. Next, the doctor brings a biconvex lens (magnifying glass) to the patient’s eye. He holds it from the patient’s face at a distance of 7-8 cm. The optical product magnifies the image and makes it possible to examine the fundus of the eye.
Indirect ophthalmoscopy can be performed using various lenses and mirrors. The picture turns out to be stereoscopic. The doctor sees the image upside down. The examination is especially effective in diagnosing cataracts in the maturation stage. Indirect binocular ophthalmoscopy has other advantages:
- wide overview, the ability to examine peripheral parts;
- speed of implementation;
- lack of patient contact with the device;
- Possibility of use even in poor lighting.
If we talk about the disadvantages, the following fact should be mentioned: reverse ophthalmoscopy does not make it possible to greatly enlarge the image, as in the direct method. In this case, the doctor can prescribe both types of studies. The reverse one helps to quickly examine the fundus of the eye and identify pathology, and the direct one allows you to study in detail the areas of the fundus affected by the disease.
In addition to direct and indirect ophthalmoscopy, other methods are also used. One of the most famous is biomicroscopy. Let's find out what its features are.
Examination price
If the patient applied to a free medical institution under the policy, the cost of the doctor’s services and the procedure performed will be free. A person will only need to buy medications that dilate the pupil.
If the patient goes to a private clinic, the cost of the procedure is included in the services of an ophthalmologist. The price of the clinic depends on the qualifications of the specialist. Most often, the price varies from 500 to 1500.
The ophthalmoscopy procedure is one of the main examinations in ophthalmology. Using this method, you can look at the fundus of the eye and identify its deviation from the normal parameters of the organ of vision. It is possible to identify systemic diseases of the cardiovascular system that affect microcirculation vessels. In this case, the ophthalmologist is able to promptly refer the patient to specialists and prevent the development of irreparable complications.
What is ophthalmoscopy and why is it performed?
Ophthalmoscopy is a diagnostic test.
Ophthalmoscopy is a diagnostic test that allows an ophthalmologist or other physician to examine the fundus of the eye. Special instruments allow you to determine the condition of the optic nerve, retina and blood vessels of the eye.
This method is useful not only for the early diagnosis of eye diseases, but also for identifying other pathologies.
This short (2-5 minutes) procedure is the cornerstone of the process of diagnosing retinal conditions. Conditions such as retinal detachment, epiretinal membrane, diabetic retinopathy and glaucoma can be safely diagnosed using ophthalmoscopy alone.
Ophthalmoscopy is also performed in patients with systemic diseases affecting the blood vessels of the eye. Usually these are hypertension and diabetes. Often, a competent ophthalmologist, based on the results of a fundus examination, can tell whether a patient has a serious vascular disease.
Now we will try to determine the main indications for ophthalmoscopy.
- Damage to the optic nerve.
- Signs of retinal detachment.
- Glaucoma, manifested by increased intraocular pressure.
- Macular degeneration with loss of vision in the center of the visual field.
- Cytomegalovirus retinitis is an infectious process in the retina.
- Melanoma (skin cancer) that has spread to the eye tissue.
- Hypertension.
- Diabetes.
In addition, ophthalmoscopy is indispensable in the differential diagnosis of visual impairment. Using this method you can diagnose:
- Myopia is a malfunction of the visual analyzer, which makes it difficult to see distant objects.
- Farsightedness is a malfunction of the visual analyzer, in which the eye focuses better on distant objects and perceives nearby objects worse.