Indications for tonometry
Often changes in IOP go unnoticed. The clinical picture, characterized by cephalalgia, asthenopia and redness of the mucous membrane of the eyes, is attributed to overwork. Most patients do not even suspect there is a problem.
Tonometry is prescribed and performed by an ophthalmologist. Indications for the procedure:
- neurological disorders;
- age over 40 years;
- complications after operations;
- spasm of accommodation;
- stress;
- fluid retention in the body;
- problems with the functioning of the endocrine system;
- presence of glaucoma in close relatives;
- glaucoma in the study patient.
There are also contraindications to the procedure. Measuring intraocular pressure using the Maklakov method is not carried out in cases of allergies to anesthesia, viral and bacterial infections, or a pathological condition in the structure of the cornea.
The examination is prohibited for patients under alcohol or drug intoxication, as well as for psychological disorders with increased aggression.
Rules for the procedure
Maklakov's tonometer was invented more than 100 years ago. Until today, the device is considered one of the most effective, allowing the most accurate detection of changes in intraocular pressure. In appearance, the device resembles a hollow metal cylinder, inside of which there is a lead rod, and frosted glass is installed at the ends.
Measuring eye pressure using the Maklakov apparatus occurs according to the following algorithm:
- An anesthetic is instilled into the patient's eye. The drops begin to act in 10-15 minutes, during which time the ophthalmologist has time to prepare the tonometer itself;
- the glass of the device is treated with a disinfecting solution and covered with a layer of special glycerin paint;
- the subject lies down on the couch (no need to place any pillows or bolsters under the person’s head) and opens his eyes;
- After this, a weight is placed on the open eye. The device is placed in the center of the eyeball. Only in this case a reliable result is obtained.
To reduce the risk of undesirable consequences, the instructions must be strictly followed.
Important! The higher the intraocular pressure, the denser the consistency of the eye, which means that the area of contact of the tonometer with the mucous membrane will be minimal. In this case, after transferring the device to paper, the diameter of the white spot remaining on it will be small. The lower the intraocular pressure, the larger the white spot remaining on the paper will be.
In addition to the above, it is worth noting that the device used must be in perfect condition: scratches, chips and dents make the device unsuitable for further use. Failure to observe this precaution will aggravate eye problems, since the measured data is likely to be unreliable.
IOP measurement methods
There are several ways to measure intraocular pressure:
- palpation - by touch;
- contact - Shiotz, Maklakov tonometer;
- non-contact - pneumometry, electronography.
The latter method is the most modern in ophthalmology. The contact method for determining intraocular pressure is most often used. With its help, IOP measurement is carried out by flattening the cornea. The Maklov method is the most common. Its advantage is low cost, simplicity and high accuracy of IOP determination.
Interpretation of ophthalmotonometry results according to Maklakov
The diameter of the light circle on the impression is proportional to the degree of flattening of the cornea during the study. Accordingly, the higher the pressure, the less ink will be removed and, accordingly, the smaller the light area of the print.
A transparent ruler measures the diameter of the light area. The researcher should place it with the scale down to avoid distortion. The result is assessed through a binocular loupe. The scale applied to the ruler allows you to immediately convert the result into millimeters of mercury.
When measuring with a regular ruler (up to 0.1 mm), the pressure indicator is calculated as the ratio to the weight of the tonometer: the square of the indentation radius by the number “Pi” and by the specific gravity of mercury (13.6).
The normal eye pressure according to Maklakov is the range of 18-26 mm Hg. Art.
Method for measuring intraocular pressure according to Maklakov
This is a method of contact measurement of IOP, which means contact of the weight with the cornea of the eye. Maklakov's tonometer is a mechanical device. These are 2 weights weighing 10 grams each.
To obtain an accurate result, it is necessary to strictly follow the measurement procedure.
Algorithm for tonometry to measure IOP according to Maklakov:
- The areas of the weights are wiped with a swab dipped in an alcohol solution. Then wipe dry with a sterile swab. Disinfection is carried out 2 times. Repeated use of alcohol after 15 minutes.
- The plates or weights are treated with a thin layer of special paint, which is not harmful to the eyes and is not toxic. The dye used is Collargol (contains 70% colloidal silver and 30% albumin protein) or Bismarck (a basic brown aniline dye used for staining histological and bacterial samples). Collargol (2 g) must be crushed in a mortar, then mixed with distilled water and glycerin. Bismarck brown is mixed in the same way, but in a volume of 1 gram.
- The tonometer is inserted into the socket of the support handle.
- The plate is touched to the stamp pad, which is pre-impregnated with paint. Then remove excess dye with a sterile swab.
- A solution of Dicaine or Lidocaine is instilled into the eyes. 2 drops into each organ of vision 2 times with an interval of 2-3 minutes.
- The patient is asked to lie down on the couch. The doctor is located at the head of the patient. The patient is asked to raise his hand and look up at the index finger.
- The ophthalmologist opens the eyelids with the thumb and index finger. The doctor widens the palpebral fissure. If there is excess tear fluid, remove it with a cotton swab or ball before applying the measuring device. With the second hand, the tonometer is installed on the central part of the cornea using a supporting handle. This should be done carefully, without pushing.
- Then the weight is lowered onto the cornea and under its weight it flattens. Contact of paint with the cornea is 1 second. The doctor immediately removes the measuring devices by lifting the holding handle. At the moment the device comes into contact with the cornea, the paint is washed off from the plate due to the circulation of tear fluid.
- Next, the doctor makes prints of the device’s platform on paper, which is pre-moistened with alcohol and ether or simply an alcohol solution. A colorless circle remains at the point where the device came into contact with the cornea.
- The ophthalmologist measures it using a ruler, the divisions on which represent millimeters of mercury. Measures the diameter of a colorless circle.
First, the study is carried out on the right eye, the doctor writes down the results on a piece of paper, which indicates the patient’s name, time and date of the procedure.
Measurements are then taken in the same way for the left eye. The action of Lidocaine is long-lasting. The ophthalmologist will have time to measure intraocular pressure for both organs of vision.
Tonometry according to Maklakov
Tonometry according to Maklakov
Ocular tonometry is carried out in several ways - according to Maklakov, palpation and non-contact. Maklakov Alexey Nikolaevich is a famous ophthalmologist, professor at the Imperial Moscow Institute, author of numerous works on vision medicine, creator of the first eye tonometer.
The design of the tonometer developed by Professor Maklakov is extremely simple. The device consists of a cylindrical weight, which is fixed in the desired position using a holder. The tonometer package includes 10 g weights, one holder, three rulers and a storage case.
The mass of the device does not exceed 100 g. The error in the mass of each weight should not be more than 20 mg. The design of the holder must allow the weights to move under the influence of their own gravity.
The presence of mechanical damage on the surface of the weights (scratches, dents, chips, cracks) is not allowed. Their presence indicates that the device is unsuitable for use.
Measuring intraocular pressure with a Maklakov device is carried out after instillation of an anesthetic into the eyes of the patient under study. Then a weight from the kit, previously soaked in paint, is placed on the open eye. The weight is held by a holder.
After this, an imprint is left on a paper sheet with the weight used in the study and the amount of paint that has come off from its base in contact with the surface of the eye is determined. Measurements are taken using the included rulers.
Tonometry according to Maklakov is based on the inversely proportional relationship between the value of intraocular pressure and the size of the imprint left by the weight. The higher the intraocular pressure, the denser the cornea and the smaller the area of contact with it by the base of the weight.
At the same time, the size of the print left on the paper is quite large. With low intraocular pressure, the opposite picture is observed.
Normally, the pressure in the ocular structures when measured according to Maklakov is 15-25 mmHg. In male and female patients, intraocular pressure is slightly different - in women it is higher.
Also, ophthalmotonus depends on many other factors:
- elasticity of the sclera;
- tone of blood vessels piercing the eye;
- degree of blood filling of the eye vessels;
- proportions of formation and removal of intraocular fluid;
- state of the nervous system.
Using a Maklakov tonometer to measure eye pressure, you can obtain highly accurate results. However, a significant disadvantage of this method is the use of anesthetics, to which the patient may experience allergic reactions.
If sanitation rules are not followed, an infection may occur in the eye through contact with the tonometer weight.
The following video will introduce you to the principle of operation of the Maklakov tonometer:
Evaluation of results
The smaller the colorless disc after contact of the plate with paper soaked in alcohol, the higher the patient's intraocular pressure. If the diameter is large, then the pressure is low.
To measure IOP, a Polyak ruler is used. It gives results in mmHg. It is applied so that the light circle fits between the diverging lines of the scale and its edges exactly touch these lines.
Normally, the result should be 10–20 mmHg. This figure may change throughout the day. For example, in the morning, intraocular pressure is higher. Therefore, to obtain accurate results, ophthalmologists recommend performing the procedure 2-3 times a day at different times.
The boundaries of the circle may be unclear. This indicates poor quality paper used to make the print. The print will be clearer if you let the alcohol dry slightly, so the edges will not blur.
What is intraocular pressure
Intraocular pressure (IOP) is the pressure exerted by the internal contents of the eyeball on the ocular membrane. The indicator characterizes the normal functioning of the eyes. Tone depends on:
- hydrodynamics of the internal environment of the eyeball;
- filling level of orbital vessels;
- parameters of the vitreous body and lens;
- the level of elasticity of the ocular fibrous capsule (outer layer).
The latter value is not constant and fluctuates even throughout the day. This depends on the circulation of intraocular fluid, its inflow and outflow. The influx or addition occurs due to the production of moisture by the ciliary body.
The decrease or outflow occurs due to the drainage system in the form of the trabecular apparatus. Due to this constant microcirculation of fluid, metabolism occurs in the tissues of the eye. The unit of IOP measurement is mmHg. The norm is 22-23 mm. Hg Art.
Intraocular pressure may fluctuate up and down or be normal. Due to normal indicators, the eye retains its spherical shape and provides itself with nutrition. In a healthy adult, the range of fluctuations varies from 18 to 30 mm. Hg Art.
The process of determining IOP by a specialist is called eye tonometry. If the outflow is impaired, fluid accumulates in the eye and IOP increases. This can also happen normally: with eye fatigue, an attack of hypertension, or stress. But such phenomena are short-lived and go away on their own.
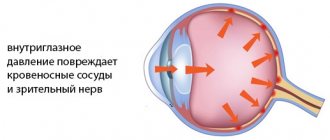
Important! An increase in ophthalmotonus leads to damage to the optic nerve, impaired nutrition of the eye and the development of glaucoma.
Reduced IOP occurs when:
- eye injury;
- hypotension;
- inflammatory eye pathologies (iridocyclitis, uveitis);
- dehydration, etc.
A decrease in ophthalmotonus leads to mucosal atrophy and dry keratoconjunctivitis develops; there may be clouding of the cornea and other pathologies against the background of decreased nutrition of the eye.
Useful video
Contact tonometry:
Indications for determining IOP
Indications for measuring IOP are:
- Glaucoma diseases - IOP determination is performed quarterly.
- Glaucoma among loved ones - the procedure is preventive in nature. Performed once every 2 years.
- Ages over 40 – once a year.
- Suspicion of cataract.
- The presence of pathologies of the heart, blood vessels and the development of heart failure.
- Endocrine pathologies (obesity and diabetes, Graves' disease, menopause).
- Some neurological diseases (skull trauma, intracranial hypertension, brain tumors, etc.)
- Congenital eye abnormalities.
- Foreign body in the eye.
- Kidney and liver pathologies.
- Chronic headache.
- Dry eye syndrome.
- Retinal detachment.
- Dilated or deformed pupil.
- Enophthalmos (retraction of the eyeball).
- Dehydration, hypotension, shock, penetrating eye injuries.
TONOMETERS in ophthalmology
TONOMETERS in ophthalmology
(Greek tonos voltage + metreo measure, measure) - devices for measuring intraocular pressure. The principle of the study is to measure the deformation of the eyeball under the influence of pressure of a certain weight (mass).
Depending on the form of deformation of the eyeball, applanation and impression tonometers are distinguished. When using anplanation tonometers, intraocular pressure is determined by the amount of flattening (aplanation) of the cornea, while impression tonometers are determined by the degree of its depression by the plunger (rod) of the device (see Tonometry).
The first T. were proposed in the 19th century. A. Graefe (1863), Dor (H. Dor, 1865), Weber (A. Weber, 1867), etc. All of them were impressionistic. Measurements of intraocular pressure were made on the sclera, were unreliable and were almost never used in wedge practice. In 1884, A. N. Maklakov proposed measuring intraocular pressure on the cornea using applanation T. of his own design. This method has found wide application.
Maklakov's tonometer is a hollow metal cylinder 4 cm high, weighing 10 g; its bases are expanded and have platforms made of milky white or frosted glass, diameter. 10 mm, loop-shaped handle allows you to hold the T. body in a vertical position during examination (see Fig. 3 to article Tonometry). The imprinted circle of corneal flattening is transferred to paper and measured with a special ruler indicating intraocular pressure in millimeters of mercury.
In addition to the Maklakov tonometer, honey. industry, also produces a set of Maklakov tonometers weighing 5; 7.5; 10 and 15 g for elastotonometry using the Filatov-Kalfa method. The elastotonometry method consists of sequentially measuring intraocular pressure with four tonometers; Based on the results of the study, a curve is drawn, the nature of the cut reflects the condition of the membranes of the eye.
Rice. 1. Goldmann tonometer mounted on a slit lamp: 1 - tonometer body; 2 — Gruby lens for direct ophthalmoscopy; 3 - system of levers for changing the position of the tonometer prism; 4 — part of the tonometer in contact with the eye (prism); 5 — slit lamp illuminator; 6 - binocular microscope.
T., designed by Goldmann (H. Goldmann, 1954), is an improved microcontact applanation tonometer (Fig. 1), mounted on a slit lamp (see). Corneal applanation is performed at very low pressure values, and the corneal flattening circle is measured under a microscope. The area of eye deformation when using microcontact tonometers is extremely small (the volume of intraocular fluid displaced during tonometry is approximately 0.5 μl). Thanks to this, the measurement results are as close as possible to the true intraocular pressure. Manual versions of T. such as the Goldmann tonometer have been proposed, allowing for research in both horizontal and vertical positions of the patient.
Applanation pneumoelectric machines are known, equipped with sensors pneumatically connected to an electronic pressure transducer, recorders, and a digital reading system for results.
Rice. 2. Schötz tonometer: 1 - tonometer scale; 2 - part of the tonometer rod (plunger) in contact with the eye; 3 - additional weight to increase the created load; 4 — tonometer body.
The main impression device for measuring intraocular pressure is T., proposed by H. Schiotz (1905), or its technically improved versions (Fig. 2). The working part of the T. is made in the form of a cylindrical body, the lower end of which has a slightly concave platform (the part of the T. in contact with the eye). According to the center of the platform along the cylinder axis, a plunger weighing 5.5 g and dia. moves freely in the channel. 3 mm; There are also additional weights that, if necessary, are placed on the plunger in order to increase its weight to 7.5; 10 and 15 g. During the study, under the influence of a load, the plunger is pressed into the cornea to a certain depth, the edges are marked by the arrow of the device. The result is read on a scale and recalculated using calibration tables.
See also Tonometry.
Bibliography:
Maklakov A. N. Ophthalmotonometry, Med. review, vol. 22, no. 24, p. 1092, 1884; Go! dmann H. Un nouveau tonomMre & applanation, Bull. Soc. frang. Ophthal., t. 67, p. 474, 1954; S with li i 6 tz H. Ein neuer Tonometer, Arch. Augenheilk., Bd 52, S. 401, 1905.
See also bibliogr. to Art. Tonometry.
V. M. Budnik, B. I. Vagin, A. A. Stetsin.
Device design and quality characteristics
Intraocular pressure is measured according to Maklakov using a special tonometer. The device is equipped with tools for a full session for one patient, it includes:
- Two weights, cylindrical in shape with flat ends.
Weights with different weights
Set of Maklakov tonometer with three rulers
The weights have a lead weight inside. They need to be held with special holders; there is no need to create excess pressure on the cornea.
It should be noted that Maklakov tonometers are still used everywhere today, because they measure with almost 100% accuracy. The disadvantage of this device is the risk of infecting the patient during the examination and the likelihood of an allergic reaction to the anesthetic. The measurement accuracy of this device greatly depends on the qualifications and skills of the specialist who takes the measurements. Movements during measurement must be practiced until they become automatic, then accuracy will be guaranteed.
For what symptoms is it advisable to consult a doctor for tonometry?
Typically, the onset of the disease is indicated by symptoms such as:
- blurred and blurred vision,
- loss of visual fields on one or both sides,
- headache, often temporal localization,
- flashing of flies or black dots before the eyes,
- pathologically rapid eye fatigue when reading or working at a computer,
- constant lacrimation,
- retraction of the eyeball, reduction in its size (with very low intraocular pressure).
Most often, tonometry is prescribed for suspected glaucoma , so patients over 40 years of age should be aware of the symptoms of this disease.
The main signs of the onset of the disease are “fog before the eyes,” narrowing of the visual field and the flashing of bright rainbow circles in bright light. These symptoms are observed during the interictal period. An acute attack of glaucoma is accompanied by intense unilateral pain in the eyeball, photophobia, nausea, and dizziness. If such symptoms appear, an examination by an ophthalmologist is mandatory, and if they are prescribed tonometry, the examination should be performed immediately!
Carrying out tonometry
On the day of the study, the patient comes to the assigned office. He needs to take off his glasses because the doctor will instill eye drops with an anesthetic to suppress the corneal reflex. The patient is asked to lie down or sit down, depending on the type of technique. Next, tonometry is performed directly.
In the case of a non-contact examination, the procedure takes a matter of seconds and will not cause any inconvenience to the patient.
non-contact tonometry
If classical tonometry according to Maklakov is prescribed, the procedure will be a little more complicated.
A nurse or doctor thoroughly wipes the plates of metal cylinders used as weights with an alcohol-containing disinfectant solution. Usually this is done twice.
After disinfection, the cylinder plates are dipped in a pad soaked in a dye. Typically, paint for tonometry is made from a mixture of distilled water with glycerin, with an admixture of a coloring pigment - collargol.
contact tonometry according to Maklakov
Then the doctor sits at the head of the patient lying on his back and instills a few drops of lidocaine into both eyes. After a couple of minutes, he asks the patient to raise his hand up and fix his gaze on the index finger. Gently holding the eyelids, the doctor carefully lowers the cylinder, the paint from the plates of which partially remains on the wet cornea. This blurry circle in the center of the cylinder is the indicator that needs to be measured. After applying the cylinders to the corneas of both eyes, the plates are printed on paper soaked in alcohol. The result is a circle-shaped print with a blurry circle in the center. Next, the diameter of the circles is measured with a ruler, and the doctor makes his conclusion about the value of intraocular pressure.
After the examination, there is no discomfort left, so the patient can go home if the examination was carried out on an outpatient basis in a clinic.
Instructions for using the tonometer
Before you begin the procedure, you need to check the functionality and condition of the tonometer. The glass plates must be intact, otherwise the patient may damage the cornea. The holder secures the cylinder well, which at the same time moves freely inside it.
The records are also wiped with alcohol. Usually this is enough, but if a patient is suspected of having conjunctivitis, the tonometer is boiled in a two percent soda solution for half an hour.
During the boiling process, water may leak into an unsealed tonometer, so after such emergency disinfection, Maklakov’s device should be dried on a sterile surface, placed on gauze.