29.01.2018
Interesting
Bogacheva Sharofat Bairovna
The kidneys, adrenal hormones and the central nervous system play a leading role in maintaining and regulating water-salt balance.
The kidneys regulate the excretion or retention of water and electrolytes. This process depends on the concentration of salts in the body, which is maintained at the required level. This regulation is mainly associated with sodium ions.
Kidneys
The kidneys belong to the urinary system, which also includes the ureters, bladder and urethra.
Urine filtered by the kidneys through the ureters descends into the bladder, where it can remain for some time, and then, as a certain volume is reached, it is discharged out through the urethra. This is the main way for “waste fluid” to exit the body.
Normally, urine does not contain the elements necessary for the body: proteins, amino acids, glucose.
The kidneys are located in the retroperitoneal space on both sides of the spine, approximately around the 12th thoracic and 2nd lumbar vertebrae. As a rule, the right kidney is located slightly lower than the left, as this depends on the liver located nearby.
The kidney capsule is protected and securely fixed by the surrounding adipose tissue. The presence of adipose tissue is vital! In its absence (with severe weight deficiency, body mass index less than 19 - see the article “Obesity Epidemic”), fixation is disrupted and mobility and prolapse of the kidneys become possible.
The buds are bean-shaped, dense, 10–12 cm long and 5–6 cm wide, weighing 120–200 g each. With such small sizes, the kidneys perform a large number of vital functions:
- removal of excess fluid;
- excretion of end products in urine, in particular, toxic products of nitrogen metabolism to the body;
- regulation of total blood volume and, as a consequence, blood pressure
- regulation of ionic composition and osmotic concentration of blood plasma;
- acid-base state of the blood, when violated, multiple changes in functions are formed in other organs;
- regulation of blood cell formation (erythropoiesis) and blood clotting;
- regulation of calcium, protein, lipid and carbohydrate metabolism;
- production of biologically active substances.
What structures provide all these functions?
The main structural and functional unit of the kidney is the nephron. There are up to 1.3 million of them in each kidney. And if for any reason the nephrons stop working, all kidney functions are disrupted. A nephron is a network of vascular capillaries through which blood flows. An arterial vessel enters each nephron, splits into many small vessels, forming a glomerulus (glomerulus), which again connects into one exiting vessel.
In this system, primary urine is first formed from the blood, which, passing further through the complex canalicular apparatus of the nephron, is transformed in its composition into the final version of the “waste liquid”. The kidneys are able to do their job even if they retain only 30% of their functional capacity (people can live normally with one kidney).
There is no other organ that is so dependent on blood supply. If it is damaged, the kidney ceases to fully perform its functions. With the same mass of the kidneys and heart, 25% of the minute blood volume is supplied to the kidney, while other organs supply up to 7–8%.
Causes of kidney cysts
Kidney cysts can be congenital or acquired:
- congenital cysts occur during intrauterine development of the fetus;
- acquired cysts occur after the birth of a person during his life.
The cause of kidney cysts is not entirely clear. One hypothesis explains their appearance by poisoning of the kidney tissue with salts of heavy metals, protein, bacteria, various poisons and, as a result, clogging of the tubules of the kidney tissue with protein masses. The glomeruli of the renal parenchyma, continuing to produce primary urine, expand and give rise to the appearance of a cyst. As a rule, once a cyst appears, it reaches its size and stops growing. There are about 97% of such cysts. But there are cysts that continue to slowly grow. Therefore, patients are recommended to undergo regular follow-up examinations.
The appearance of cysts can also result from:
- hereditary predisposition;
- tuberculosis;
- infectious diseases and other factors.
Malignant kidney cysts occur in 1.5-3% of cases. They are called "dermoid" cysts. These cysts are always congenital and require surgical treatment. Hair and primary teeth are found inside these cysts. Hence the name of these cysts - because of the tissues of the dermos (skin).
Urine formation
Urine is formed from blood. What causes the liquid part of the blood to pass through the walls of blood vessels into the kidney capsule? Filtration of fluid is ensured by the difference in blood pressure in the vessel entering and leaving the nephron (due to the different diameters of the vessels).
Capillaries are the smallest and thinnest vessels. Usually the pressure in them is insignificant - about 15 mmHg, but in the capillaries of the kidneys it reaches values of 70 mmHg, more typical for the middle artery.
As a result of this difference in pressure, filtration occurs, which occurs spontaneously, without control from hormones and the central nervous system. Abundant blood supply and adequate blood pressure are important factors, changes in which in diseases (for example, kidney disease, hypertension) can lead to disruption of urine formation and water-electrolyte balance in general.
What is filtered from the blood into the urine?
First, primary urine is formed in the kidneys (about 200 liters per day with a filtration rate of 125 ml/min), which is essentially blood plasma. Plasma differs from whole blood in the absence of formed elements (erythrocytes, leukocytes, platelets).
Normally, primary urine still contains low molecular weight components and glucose necessary for the body. But already at this stage, blood cells and proteins should not enter the urine.
What happens next?
At the second stage of urine formation, the amino acids, glucose and other substances needed by the body remaining in the primary urine are returned back to the blood. Reabsorption (reabsorption) of salt (and here we mean only sodium) and water also occurs. And out of 200 liters, 60 liters remain - a third of the filtered volume.
Further, as a result of a cascade of sodium and water reabsorption processes, the volume of fluid in the kidneys gradually decreases and, accordingly, the concentration of urine increases.
Normal kidney function allows you to retain water in the body.
How does this happen? Why does water return to the bloodstream, and not be removed outside, and a person’s diuresis is not 20–30 liters per day, but only 1.5–2 liters?
After the urine has traveled a long way, it enters the terminal nephron, in which the reabsorption of sodium from the renal tubule into the blood is carried out under the control of the adrenal hormone aldosterone.
We already know that sodium is an osmotically active substance. The salt passes back into the bloodstream and water, as a solvent, follows the sodium. As a result, the output urine has the highest concentration.
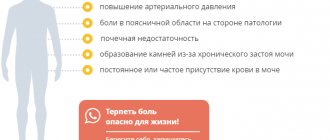
Symptoms of a kidney cyst
Symptoms of kidney cysts depend on the size and location of the cysts in the kidney tissue
Cysts up to 15 mm
If the cysts are small, up to 15 mm in diameter, single and located far from the renal vessels (vascular bundle), they may not cause symptoms at all.
Most often, such cysts are detected accidentally during ultrasound (ultrasound) or X-ray examination of the kidneys (excretory urography, computed tomography or magnetic resonance imaging).
Cysts from 20 mm
If the cysts are medium and large in size (from 20 mm to 90-110 mm in diameter) and are localized near the renal pelvis and vascular bundle, then these cysts can significantly interfere with the functioning of the kidney. They can impede the outflow of urine from the renal pelvis, compress the vessels of the kidney and disrupt its trophism. Such cysts can cause dull aching pain in the lumbar region, a feeling of rapid fatigue, changes in the biochemical blood test and in the general urine test. In a biochemical blood test, indicators of body poisoning with nitrogenous wastes (creatinine and urea) may increase. A general urine test may reveal bacteriuria and erythrocyturia. An increase in diastolic blood pressure is also possible.
How does kidney function depend on blood pressure?
The kidneys are the first organ to respond to changes in blood pressure.
When blood pressure drops, blood flow in the kidneys decreases, which leads to their hypoxia (oxygen starvation). In response to this, the kidneys release renin into the blood (translated from the Latin “ren” means “kidney”), which triggers a complex chain of reactions in the body leading to vasoconstriction and an increase in overall blood pressure. As a result, blood flow to the kidneys increases and their functions are restored. So, normally (when a person is healthy, attentive to himself, and all his physiological regulatory mechanisms are preserved), the compensatory renin-angiotensin-aldosterone mechanism for regulating blood pressure and blood volume in the body is triggered.
Why do these mechanisms fail?
At first we do not feel a decrease in blood pressure. Feeling some weakness or just for pleasure, we “cheer up” with a cup of coffee or tea in the morning and throughout the day. The effect of caffeine on blood vessels, the lack of a normal drinking regime, and taking medications lead to a failure of a well-functioning system, which already becomes the cause of the formation of arterial hypertension.
Due to what? And why do they say that the liver is “to blame” for high blood pressure?
The fact is that the liver produces the protein angiotensinogen - an inactive form of angiotensin. It constantly circulates in the blood and does not bring us any harm. But when renin is released into the blood, a chain of conversion of angiotensinogen is started (under the influence of a substance produced by lung cells - angiotensin-converting enzyme - ACE) into the active substance angiotensin, which already has a powerful vasoconstrictor effect. This is one of the mechanisms for increasing blood pressure. Blood pressure-lowering drugs often contain an ACE-blocking agent, which interferes with the production of active angiotensin.
In addition to its vasoconstrictor and hypertensive effects, angiotensin also activates the release of the adrenal hormone aldosterone into the blood, which increases sodium reabsorption. Following this, the return of water into the blood increases, which leads to an increase in its volume. And any increase in the volume of circulating blood again contributes to an increase in blood pressure.
It turns out to be a vicious circle!
Why did I describe this in such detail? To understand how complex and interconnected everything is, how one thing pulls the “tail” of another... Any violations always have causes, and their consequences become the causes of subsequent changes leading to diseases, which at first glance may be very far from the root causes.
Now we know how kidney function, circulating fluid volume and blood pressure are related.
There is another hormone produced in the central nervous system (in the hypothalamus) that is involved in the regulation of normal fluid levels in the body - vasopressin. Its other name is antidiuretic hormone, i.e., it reduces fluid secretion. It retains sodium, and therefore water.
This is important to prevent dehydration (as a result of polyuria) and maintain the amount of fluid the body needs.
Insufficient release of antidiuretic hormone leads to a disease such as diabetes insipidus, one of the clinical signs of which is polyuria - increased urination. Diuresis can increase up to 20 liters per day; accordingly, such patients constantly drink fluid to replenish its loss.
So, normally a person has the following indicators: urine volume is 1.5–2 liters with a high osmotic concentration, there is no glucose, proteins, blood cells, microorganisms. If any of the above is detected in the urine, then it is now not difficult to understand at what stage of urine formation the disorder occurred.
What do diuretics (diuretics) do?
They enhance the process of urination by inhibiting the reabsorption (reabsorption) of sodium. Sodium pulls water with it, which leads to an increase in urine output. Typically, diuretics are prescribed for hypertension, edema, and kidney disease. And, as a rule, it is recommended to limit the amount of liquid and salt (up to a salt-free diet). Is it correct?
On the scale of the body, this is a violation of water-salt metabolism.
“Spot-on” medications can be used to reduce blood pressure or swelling here and now. These are emergency actions. How can you take them for years, and sometimes decades, while constantly increasing the amount of other medications designed to neutralize the side effects of diuretics?
Methods for diagnosing kidney cysts
Most often, kidney cysts do not require active treatment; dynamic observation is sufficient (up to 2-3 times a year).
Examination if a cyst is detected
The examination of patients with identified kidney cysts should include:
- tests: general urine; urine culture for microflora, degree of bacteriuria and sensitivity to antibiotics; blood clinical; blood biochemical;
- Ultrasound of the kidneys;
- or MRI of the kidneys (once every 2-3 years);
- excretory urography;
- dynamic renal scintigraphy (showing the functional capacity of the kidneys);
- consultation with a urologist.
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Children's features
In early childhood, the kidneys are insensitive to antidiuretic hormone.
Infants need to be given water to drink. Not juices, not “soothing” sweet tea, but just water, since it is the lack of water in the tissues that can cause anxiety.
If children do not receive enough water (not milk, since milk is nutrition), this can lead to tissue dehydration, intoxication, fever, and disturbances in bowel movements and sleep.
Remember, newborns and infants do not have a developed sense of thirst!
If you violate the feeding regime and give children (according to your habits) highly salty foods, this can cause swelling in the tissues, since increased osmolarity contributes to fluid retention in the body. Therefore, it is necessary to treat both the feeding regime of children and the water regime with great care and caution.
Why am I talking about this in too much detail? Definitely not so that you understand the complex mechanisms that many doctors don’t remember about. But so that you understand how many organs and systems are involved in a seemingly “simple” decrease or increase in blood pressure, a decrease in urine output, the formation of edema, etc. So that you do not rest on the medications chosen for you “for the rest of your life,” which “stabilize” your blood pressure, urine output, etc., but set the goal of improving the functioning of your organs through lifestyle control. (The lack of control of which has already led or will certainly lead to illness). To avoid taking medications as much as possible, which are always toxic and foreign to the human body, and lead to secondary changes in other organs.
I urge you not to rest on “slightly elevated” test results, “small doses” of medications taken, and not to rely on “maybe it will somehow resolve itself.”
Be aware of your condition. Map out the path you will take to become healthy.