home
Diseases
Cancer
Upper and lower eyelid cancer
Cancer can affect absolutely any part of the human body. You can avoid unpleasant consequences. But it is extremely important to diagnose the disease in time and prescribe the most optimal treatment method.
The human eye, like other organs, also suffers from cancer, and most often this disease is localized in the upper or lower eyelid. Cancers of this type grow very intensively on the eyelids themselves, but they do not tend to metastasize.
Description
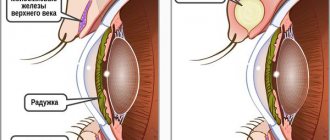
The location of cancer can be any part of the eye structure: tissues and glands, nerve endings, the bony part of the orbit and skin. The location of the tumor depends on where the cell mutation process began. The growth of a tumor can be noticed visually if it is located on the conjunctiva, lower or upper eyelid, the part of the eye closest to the bridge of the nose, under the eyelid, in the inner corner of the eye, with cancer of the meibomian (sebaceous) gland and with damage to the iris. The cancerous process can develop inside the eye and in the eye socket, and the manifestations of such a neoplasm become noticeable only when it is large.
Cancers in adults are usually secondary, having spread to the eye through blood vessels or the lymphatic system from other organs (lymph nodes, lungs, kidneys). The primary cancers of the eye are retinoblastoma and melanoma.
Cancers usually affect one eye, but retinoblastoma most cases affect both eyes. Malignant neoplasms that arise in the eye can metastasize beyond the eye: to the optic nerve, to the brain and other parts of the body. Cancer of the eyelid is the most common - in 50-90% of cases of the total number of patients. Women get sick much more often than men – about 80% of cases.
Features of squamous cell eye cancer
Squamous cell cancer of the eye: symptoms and manifestations
It is worth noting that squamous cell tumors of the eyelids are much more common than basal cell tumors. Squamous cell cancer of the eyelids of any type is a very rare disease of the protective apparatus of the eye.
Based on previous descriptions, it is worth noting that changes in lymph nodes with a squamous cell tumor are most often inflammatory in nature, which reassures the patient, since it is less dangerous for his life. The tumor in most cases appears on the border area of the epidermis and the mucous membrane of the lower eyelid, or the inner corner of the eye. First, a small compaction (nodular and ulcerative form) is observed on the skin of the eyelid, which subsequently increases, moving into the central part of the crust, and when attempting to remove it, bleeding begins.
In some sources, due to the possible spread of squamous cell cancer of the eyelids, therapy involves lymphadenectomy of the border lymph nodes, as in the case of malignant tumors of the oral mucosa, cancer of the lips or tongue. What is wrong, we can say the following. Guided by many years of observations and the principles of humanity, all this causes unnecessary trauma to patients.
Leading clinics in Israel
Assuta
Israel, Tel Aviv
Ikhilov
Israel, Tel Aviv
Hadassah
Israel, Jerusalem
Bottom line
Meibomitis of the eyelids is a common disease that affects patients from infancy to old age. It is a disease of dirty hands, poor personal hygiene, as well as a weak immune system and poor nutrition.
The disease is especially dangerous for young children who do not yet understand the importance of personal hygiene. At the first symptoms of eye disease, you should immediately go to an ophthalmologist
Only a doctor can distinguish meibomitis from barley; independent treatment of this pathology is fraught with the development of complications and transition to a chronic form.
- Ophthalmology. National leadership. - M.: GEOTAR-Media, 2014.
- S. N. Basinsky, E. A. Egorov. Clinical lectures on ophthalmology.
- Visual disability due to diabetes mellitus / E.S. Skorobogatova. - M.: Medicine, 2003.
- University of Nebraska Medical Center
Reasons for appearance
The exact causes of eye cancer have not yet been clarified, but there are several factors that influence the onset of the pathological process:
- hereditary predisposition;
- decreased immunity, chronic inflammatory diseases;
- dysfunction of the endocrine system;
- eye injury;
- influence of external harmful conditions, poor ecology;
- excess ultraviolet radiation;
- exposure to chemicals, such as acids or salts of heavy metals;
- pigment spots (nevi) on the eye shell;
- nervous stress, depression;
- smoking and alcohol;
- hepatitis B and C, HIV infection and AIDS.
Need to know! Ultraviolet rays have an aggressive negative effect on the eyes. For this reason, you should not stay in the sun for long periods of time, and you should also wear sunglasses with high-quality lenses to protect your eyes.
Prevention
Since the true causes of chalazion remain unknown, it is also not possible to develop specific preventive recommendations
Therefore, parents should pay attention to the child’s compliance with general recommendations for visual health.
Such common childhood ailments as styes, conjunctivitis, and blepharitis need to be treated promptly and correctly. If a child wears contact lenses, you need to explain to him the hygiene rules, which are strongly recommended to remove and put them on exclusively with clean hands, and store them in a special solution.
And, of course, everything needs to be done to strengthen the child’s immunity. With a strong immune system, a child is not afraid of inflammation around the meibomian gland, the body can easily cope with it, and even if a blockage occurs, it will quickly heal itself and go away without a trace or the need for treatment.
In the next video, Komarovsky talks about other possible problems with the eyes.
Varieties
All eye tumors are classified into three groups:
- appendages of the eye and eyelids;
- eyeball (intraocular);
- eye orbit.
Intraocular tumors are considered the most dangerous, as they directly damage the structure of the eye.
The most common benign tumors include:
- nevi (colloquially moles) - develop on the skin when the division of pigment cells is disrupted; they can be either congenital or acquired. There are pigment, vascular, epidermal, intradermal and mixed;
- papillomas - small formations located on the eyelid and caused by the human papillomavirus;
- keratoacanthomas - arises from the epithelial cells of the hair follicle and nearby sebaceous glands, have the shape of an oval or round node up to 10 cm in diameter. There are also multiple species with many nodules, skin-colored with horny layers in the center and raised edges in the shape of a roller.
Remember! Nevi (moles) when exposed to any factors can degenerate into a malignant formation. Several signs that should alert you: the mole is rapidly increasing in size, the color or texture has changed (cracks, asymmetry, roughness), pain and itching, inflammatory reactions.
One of the most common benign eye tumors is the pinguecula.
This growth on the eyeball is transparent or yellowish in color. Such growths appear in people's eyes in the area of the conjunctiva or cornea of the eye due to a metabolic disorder. The formation of yellow growths on the sclera is associated with an excess of fats in the body obtained from food, which the digestive organs do not have time to absorb. In addition, the following benign tumors occur:
- hemangiomas are vascular neoplasms of the conjunctiva of the eye and skin of the eyelids, multiple abnormal plexus of bright red vessels.
- keratoacanthomas - small tumors with a crater inside on the skin of the upper or lower eyelid;
- fibromas are dense, painless neoplasms that do not have a capsule, but are well circumscribed;
- fibroids (pigmented or non-pigmented) - affect the muscles of the iris and can lead to the development of glaucoma;
- Teratomas are extremely rare congenital tumors of the orbit that develop from germ cells, are detected immediately after birth and develop rapidly;
- syringoadenomas - tumor-like lesions of the sweat glands on the skin near the eyes and the skin of the eyelids, appearing as flesh-colored nodules;
- Neuromas are tumor-like lesions of the optic nerves;
- lipomas (wen) – neoplasms with lipid content that form only on the skin;
- trichoepitheliomas are congenital neoplasms (papules) from immature hair follicles that form in the fetus in the womb;
- lymphangiomas - neoplasms on the mucous membrane of the eye, growing from blood and lymphatic vessels, often bleeding;
- neurofibroma - a neoplasm most often affects children under 5 years of age, is characterized by slow but progressive growth and leads to orbital abnormalities, exophthalmos, diplopia;
- gliomas - the tumor is located both inside the orbit of the eye and inside the cranial cavity, or in two cavities at the same time. In most cases, it develops in children under 10 years of age, but it also occurs in patients over 20 years of age.
Malignant neoplasms of the eye are no less diverse.
Cancerous tumors include:
- melanomas (melanoblastomas) are the most common primary formations of the eye, developing from pigment cells that produce melanin. It usually occurs in patients over 40 years of age, more often in women;
- Meibomian gland adenocarcinoma is a tumor of the cartilage gland in the form of a small lump that develops inside the upper or lower eyelid. Usually occurs in women 55-60 years old, often grows into the conjunctiva of the eye, lacrimal chamber, and nasal cavity;
- angiosarcomas - tumors developing from the endothelium of the vessels of the eyelid, most often found in men 35-45 years old;
- retinoblastomas - found mainly in children 2-3 years old, develop in the tissues of the eye from cells of embryonic origin. They can appear in both eyes (bilateral retinoblastoma), which is genetic in nature;
- cylindromas are large tumor-like neoplasms of the orbit with gelatinous contents in the shape of a cylinder;
- hemangioblastomas - retinal cancer, orange-red neoplasms with dilated vessels and spreading to the optic nerve, threatening complete loss of vision;
- intraocular lymphomas – malignant tumors in the eyeball;
- chemodectomas and meningiomas - there are both benign and malignant;
- sarcomas are the most aggressive tumors, which are characterized by damage to any tissue of the eye and growth from one layer to another.
Would you like to receive an estimate for treatment?
*Only upon receipt of data on the patient’s disease, a representative of the clinic will be able to calculate an accurate estimate for treatment.
How to treat pathology
It is possible to treat uncomplicated meibomitis at home, provided that all doctor’s prescriptions are strictly followed. Two main methods are used:
- hardware therapy;
- drug treatment.
Usually, to stop the inflammatory process and restore the functions of the meibomian gland, a course of magnetic therapy is prescribed. The essence of this treatment is to expose the affected eye to a magnetic field that stimulates blood microcirculation. A special device creates magnetic fields that are similar in their vibrations to the natural biorhythms of the human body. Regular exposure to magnetic fields leads to the restoration of normal biorhythms in the tissues of the eye, improvement of blood supply and activation of metabolic processes. Magnetotherapy “spurs” the body to self-healing, as a result, the functions of the meibomian glands return to normal.
As an alternative to magnetic therapy, helium-neon laser stimulation can be used. The essence of the procedure is the treatment of affected tissues with a laser beam of a certain length and intensity. As a result, metabolic processes are activated at the cellular level, blood circulation and tissue regeneration are stimulated, and the functions of the visual organs are improved. Patients note that after a laser therapy session their pain, swelling and irritation decreased, and doctors recorded an increase in the body’s resistance to infection.
Drug treatment involves the use of various antiseptic and anti-inflammatory drugs. Before administering medications, the eye should be cleared of crusts and pus. To do this, use cotton sponges and swabs soaked in warm boiled water, chamomile infusion or furatsilin solution. For children, crusts can be removed with a cotton swab dipped in a solution of hypoallergenic baby shampoo.
After this, an antibacterial agent is introduced that can suppress the growth of staphylococci or other pathogens. Usually prescribed eye ointments with an antibacterial effect:
- tetracycline;
- erythromycin;
- hydrocortised.
Antiseptic ointment "Floxal" has proven itself well. In case of severe inflammation, it is recommended to lubricate the affected eyelid with 1% mercury ointment at night. If meibomitis is caused by seborrheic dermatitis, it is recommended to wash the skin of the face and scalp in the visual area daily with a medicated antiseborrheic shampoo.
Noticeable improvements usually occur on the second or third day, the full course of treatment lasts no more than five days. For heavy purulent discharge, the ophthalmologist may prescribe doxycycline. It is prescribed 0.1 mg twice a day, the course of treatment lasts 14 days, then doxycycline is replaced with standard antibacterial drugs and treatment continues until the patient recovers completely.
If the disease is caused by viruses, then antiviral and immunostimulating therapy is carried out. Folk remedies can be used as additional restoratives.
Folk remedies are a good complement to magnetic therapy and drug treatment
Symptoms
Each type of eye cancer develops differently and is characterized by different symptoms. What signs can be seen during visual inspection? If a cancerous tumor has formed externally, it is easy to identify. The following picture is observed: swollen eyelids, pigmentation at the location of the tumor and discomfort in the eye. Also, the first symptoms may be swelling, decreased vision, pain, and squint.
Important! It is necessary to pay attention to the mobility of the neoplasm: the main difference between eye cancer and chalazia or barley is spread into adjacent tissues. The cancerous tumor is motionless under the skin, does not have a capsule, and its borders are not felt.
For neoplasms on the eyelids, the symptoms depend on the type of tumor. Epithelial tumors form in the inner corner of the eyeball and in the lower eyelid area. As cancer develops, it grows onto the cartilage of the lower eyelid and further onto adjacent tissues. Squamous cell formation develops more rapidly and involves the lymph nodes in the process. Basal cell carcinoma of the lower eyelid (basal cell carcinoma) appears as a small nodule the color of healthy skin with a small depression in the middle. The edges of the nodule may be pearlescent. Symptoms do not appear in the early stages.
With sarcoma, which is localized in the eye orbit, exophthalmos (protrusion of the eye) develops in a short time, and pain is felt when the eyeball moves. The main symptom of sarcoma is swelling and increased eye pressure; in many cases, the affected eye ceases to see. With fibrosarcoma, a bluish nodule with pronounced vessels appears under the skin on the upper eyelid. Further development of the tumor leads to drooping of the eyelid (ptosis) and displacement of the eye.
With carcinoma (squamous and basal cell), seals appear on the eyelid in the shape of a small pea or lump. In an advanced stage, it can spread not only to the eyes, but also to grow into the sinuses between the nose and on the surface of the cheeks. A fairly common type, it occurs most often in elderly patients.
With adenocarcinoma of the sebaceous glands, a yellowish thickening forms. As the tumor grows, it pulls the eyelid into the conjunctiva, on the surface of which dirty pink growths appear. The tumor grows aggressively and forms metastases. In the last stage, ulcers appear that almost destroy the eyelid, and the eye often becomes displaced.
In melanoma, malignant cells affect the iris, choroid, or ciliary body. Vision gradually deteriorates, the shape of the pupil changes, black spots appear on the iris or in the patient’s field of vision. Metastases actively spread and spread to other organs. In some cases, secondary glaucoma may develop. A common type of eye cancer, symptoms appear in late stages.
With cancer in the conjunctival area, a rapidly growing dense whitish film of a pterygoid (vascular) or papillomatous form is formed, and swelling of the eyelid is often observed. One of the neoplasms of the conjunctiva is Kaposi's sarcoma. Forms in the form of flat-red foci of inflammation in the corner of the eye.
With a malignant neoplasm in the area of the lacrimal gland, the following symptoms are observed: red lumps in the inner corner of the eye, swollen eyelid, unpleasant and painful sensations in the area of the eye orbit, the eye loses mobility, displacement of the eyeball.
With retinoblastoma, there are four stages of the disease:
- The first is a neoplasm at rest and is difficult to detect. The main feature is the white pupil (“cat’s eyes”). This can cause loss of central and side vision, which is the cause of strabismus. The eyeball may become red, vision decreases;
- second – glaucoma has developed, the manifestations of which are constant tearing, painful perception of light, inflammation in the area of the iris, increased eye pressure;
- third - the main symptom is exophthalmos - displacement or protrusion of the eyeballs (“cancerous eyes”), metastases appear in adjacent tissues;
- the fourth is the most severe, metastases develop to distant organs. Severe pain in the head, intoxication and loss of strength are observed.
Types of squamous cell skin cancer
The squamous cell form of cancer is divided into subtypes - intercellular, small cell, multicellular and unicellular type. The types differ in external factors and treatment regimens used to combat the affected cells. The following classification according to TNM of the specified type of tumor is presented.
Plaque
This type of atypicality of the epidermis in its external characteristics resembles a sharply colored part of the skin. The appearance of small-sized tubercles is noticeably visible on the skin. According to tactile sensations, the affected area is rough. The skin takes on a noticeable density compared to other areas. At the same time, the rate of spread of cancer cells is high.
Over time, as the plaque type of tumor progresses, the affected tissues spread and deepen into nearby materials. Bleeding and severe pain may occur.
Squamous cell skin cancer
Nodal
According to external data, this type of cancer is similar to a large group of nodules of various sizes. A large cluster on the outer region of the covered part of the epidermis resembles a cauliflower inflorescence. The new growth feels dense. The affected epidermis is colored brown, and the top layer is lumpy.
In most cases, nodular squamous cell carcinoma forms in areas where scars are located and in places of previous injuries. Initially, cracks form on the skin. They are accompanied by painful sensations. Over time, small nodules appear.
The node in the early stages does not cause pain and has noticeable mobility. During the malignant process, the nodule increases in size, characteristic mobility is lost, and painful discomfort may occur. This form of pathology expresses a rapid process of spread. There is a deepening of the oncological tumor into the lower layers of the epidermis.
Ulcerative
This type of atypical course of the upper part of the skin appears on the surface with crater-like ulcers. Ulcers slightly above the surface of the body. The edge of the covered area is in the form of a roller, and the hearth deepens, carefully descending below.
Ulcers can grow rapidly. The development of ulcerative areas occurs in width, as well as in deeper epidermal layers. A characteristic feature of this type of squamous cell carcinoma is the manifestation of a specific odor. Such signs are a cause for concern and a subsequent full medical examination of the surface of the body. Pressing on a crater ulcer can cause discharge with bloody clots.
The above types of squamous cell carcinoma are similar in specific characteristics. There is a high rate of spread of cells with metastases. Therefore, a timely medical and hardware examination plays an important role. Fast and successful treatment depends on detecting even the slightest suspicion of an atypical change in skin condition.
Keratinizing skin cancer
- The non-keratinizing form can be presented as highly differentiated, spreading at a low speed, since the body produces a small volume of atypical tissues.
- Poorly differentiated non-keratinizing skin cancer progresses rapidly. The number of affected aggressive cells in the body is large.
- A differentiated type of skin tumor with keratinization is more difficult to diagnose. The cancerous formation does not have a distinct color, and the rate of development is high.
The main reason for the formation of malignant pathology of the epidermis may be a hereditary factor. A dangerous disease is divided into congenital and acquired. The reasons for the development of cancer are as follows:
- Damage to cell DNA as a result of the influence of certain factors, which causes mutation of the TP53 gene - p53 protein. The function of the protein is to regulate the life cycle of the cell, which effectively prevents pathogenic tissue degeneration. The TP53 gene is part of a group of key genes involved in blocking the possible formation of a malignant neoplasm.
- Impaired functioning of the immune system and protective function aimed at combating tumor growths - anticancer immunity. The human body periodically undergoes a series of cellular mutations. It is determined and destroyed by immune components - macrophages, T- and B-lymphocytes, natural destroyers. The production and performance of these cells is assigned to certain genes, where the mutation process reduces the effectiveness of anti-cancer immunity and can be passed on genetically to generations.
- Impaired carcinogenic metabolism - the problem involves mutation of genes that control the severity of the functioning of certain structures and processes aimed at clogging, destruction and accelerated removal of harmful microelements from the body.
The following factors contribute to the development of squamous cell skin cancer:
- Age – the disease rarely affects children and the younger generation. The rate increases sharply among patients forty years of age and older. And after 60-65 years, this atypical condition is observed quite often.
- Skin type - according to statistical indicators, a dangerous disease is mostly detected in people with light eyes, hair and white skin that does not tan.
- In men, the squamous typology of growth is observed 2 times more often than in women.
- Skin atypical manifestations - a malignant oncological process can progress on a completely healthy epidermis. However, in the majority, the development of atypicality is influenced by freckles, telangiectasia and genital warts, a precancerous condition - Bowen and Paget's disease, xeroderma pigmentosum - scar areas formed as a result of burns and radiation therapy. After these factors, a tumor can form even after 30 or more years. Also, the risk of creating a pathogenic area is affected by post-traumatic scars, trophic transformations of the skin (varicose veins), fistula tracts with bone osteomyelitis (metastasis is characterized by a 20% probability), psoriasis, lichen planus, pathologies with tuberculosis and systemic lupus erythematosus.
- Prolonged deterioration of immunity and decrease in the body's protective functions.
The following mechanisms are distinguished that provoke atypicality of normal cells:
- Ultraviolet radiation under conditions of prolonged and frequent exposure - sunbathing, PUVA therapy with psoralen, performed to combat psoriasis, and desensitization in the presence of an allergic reaction to solar radiation. Ultraviolet rays provoke mutation of the TP53 gene and reduce the anti-cancer immune defense of the human body.
- Ionizing and electromagnetic radiation.
- Prolonged exposure to high temperatures, burns, systematic long-term injury and irritation of the epidermis, precancerous disease of a dermatological nature.
- Local action over a long period of time of carcinogenic trace elements and harmful substances associated with the specific working conditions - aromatic hydrocarbons, soot, coal tar, paraffin, insecticides and mineral oils.
- Treatment with glucocorticoid medications and immunosuppressants, local use of products containing arsenic, mercury and chloromethyl.
- HIV and papillomavirus bacteria - 16, 18, 31, 33, 35 and 45 types.
- Poor and unhealthy diet, serious poisoning from nicotine products and alcohol-containing products.
If a person refuses treatment or delays therapy, the life prognosis is extremely negative. The probability of metastases reaches, according to average data, 15%. 85% of probable metastasis occurs in regional lymph nodes. In 15% of diagnosed cases, metastases expand into the bone structure and into internal structures and organs, especially into the lung. As a result, death is predicted.
A serious danger is represented by the possibility of developing a head tumor and damage to the face, which is diagnosed in 70% of cases. In particular, planar cancer of the epidermis of the dorsum of the nose is often recorded. Tumor formations are often located on the forehead, in the nasolabial folds, periorbital areas, in part of the external auditory canal, on the border of the lips, especially on the upper.
Keratoacanthoma of the skin
There are 4 stages of progression of squamous cell tumor of the skin:
- Stage 1 – in the early stages of the disease, a small compaction appears on the skin of the body. Symptoms are not expressed, there is no characteristic pain. The tumor body appears mobile. The size of the lesion does not exceed 20 mm in diameter. There are no metastases. The neoplasm takes on a yellowish or light brown tint. Diagnostics rarely reveals atypical cells at the initial stages.
- Stage 2 – the stage is accompanied by the formation of the first metastatic cells, often formed in the lymph nodes. The cancer cell spreads through the bloodstream to organs throughout the body. The size of the lesion exceeds the border of 2 cm. The compaction is pronounced. The color of the skin becomes richer. When pressing on the area, pain does not appear. However, the patient notes discomfort when pressing.
- Stage 3 – the development of the disease is characterized by an increase in the affected area and progressive metastasis. Nearby lymph nodes and materials from normal adjacent organs are included. Painful sensations become more pronounced when squeezed. It is possible that atypical contents may be released from ulcerative areas on the surface of the tumor body. The boundaries of the affected area are accompanied by ridges of skin compaction. The surface of the epidermis becomes covered with ulcerations.
- Stage 4 – the last stage of oncology development involves extensive metastasis of cancer cells to the lymph nodes and tissues. The pain is very pronounced. The pain becomes permanent. Often fluid is released from ulcerative lesions. Metastases penetrate into cartilaginous structures and bone tissue. As a result, nearby joints lose mobility.
Diagnostics
Diagnosis of eye cancer most often begins with a visual examination. Visual acuity, degree of refraction, the presence of strabismus are checked, and the fundus is examined.
Then a set of studies is prescribed:
- general examination;
- blood test (general and biochemistry);
- blood test for tumor markers;
- radiography;
- ophthalmoscopy;
- Ultrasound;
- tomography;
- tonometry;
- angiography;
- biomicroscopy;
- visometry;
- biopsy;
- MRI.
Diagnosis of eyelid cancer (upper and lower).
Diagnosis of upper eyelid cancer at the initial stage (at the first symptoms) is quite possible through visual examination. Since this skin cancer is externally localized, a specialist at the Sofia Oncology Center can easily determine its presence. At the same time, to more accurately identify which cancer of the lower eyelid occurs in this case, a histological examination may be necessary. The eye may also be examined using an ultrasound device.
You can contact the Sofia Oncology Center for timely detection of this neoplasm by coming to us at 2nd Tverskoy-Yamskaya Lane, building 10, we are located in the Central Administrative District of Moscow.
Complications
Correctly performed eyelid treatment leaves no traces. The duration of therapy largely depends on the complexity of the symptoms and the effectiveness of the medications used. Treatment of diseases should be continued until the disease is completely eliminated.
In cases of repeated occurrence, you should consult a specialist to check your blood glucose levels, since diabetes mellitus may be the cause. If treatment is started on time, one should expect positive prognoses. Proper use of therapy can eliminate the disease within a few weeks.
It must be taken into account that the pathology of the meibomian glands quickly develops into a chronic form. In this case, a hailstone appears on the eyelid, which spoils the appearance, causing people to experience discomfort. An abscess of the eyelid and purulent melting of cartilage tissue are a manifestation of a severe form of the disorder.
Also, inflammation of the meibomian eyelids can be complicated by developing conjunctivitis and blepharitis. Most often, this is the result of inept attempts to independently remove the pathology and irritation of the mucous tissues of the eyes with purulent masses.
Treatment
The treatment plan is drawn up individually for each patient and depends on the type of cancer, stage of the disease and tumor location. If the tumor has not extended beyond the eyelid, then surgery is performed to remove the growth.
With the help of cryodestruction, the tumor is exposed to liquid nitrogen. Due to the low temperature, the growth tissues are destroyed and peeled off.
In the case of surgery, a cancerous tumor on the eyelid is cut off along with the surrounding healthy tissue to avoid relapse.
On this topic
If the tumor is located on the edge of the eyelid or on its inside, then experts call electrocoagulation the best option for removal. During the procedure, an electric current is applied to the growth.
Chemotherapy is prescribed after the tumor is removed. In addition, drug treatment together with radiation therapy is applicable in situations where for some reason it is impossible to perform surgery on the patient.