Sclera
The opaque sclera is composed of tightly packed bundles of collagen fibers, and its inelastic connective tissue capsule maintains the shape of the eyeball, which is maintained by intraocular pressure and the tension of the external eye muscles. At the site of the cornescleral suture (limbus corneae) at the anterior end of the sclera, it connects with the cornea, which makes up approximately one-sixth of the area of the outer surface of the eyeball. In the place where the optic nerve leaves the eyeball, the sclera is pierced by openings like a sieve (the so-called cribriform plate, lamina cribrosa), and then it continues as the dura mater and arachnoid membrane of the optic nerve.
Uveal tract
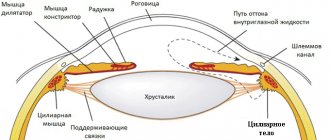
The uveal tract has a thickness of 0.2 mm, is attached internally to the sclera and consists of the iris, ciliary body and choroid. Anterior to the corneoscleral suture, it forms the ciliary body, which, in contrast to the smooth choroid, is covered with ridges, folds and processes. Its connective tissue stroma continues into the iris. The choroid is composed of lightly pigmented connective tissue and contains numerous blood vessels that nourish adjacent layers, especially the avascular outer layers of the retina.
Retina of the eye, histological specimen
Histological specimen. No. 17 Posterior wall of the eye.
Hematoxylin and eosin staining. Magnification is small and large. Find:
- sclera;
- choroid with vessels and pigmentocytes;
- retina, and in it:
- pigment layer;
- layer of rods and cones;
- outer glial limiting membrane;
- outer nuclear (granular) layer;
- outer mesh layer;
- inner mesh layer;
- ganglion layer;
- layer of nerve fibers;
- internal limiting membrane.
Additional material
- Diagram of the structure of the macula. "Histology", 1989, fig. 132, p. 345.
- Diagram of the structure of a blind spot.
- Page. Electron micrograph. Rod optic cells of the retina
- Page. Electron micrograph. Cone visual cells of the retina
VIDEO I
Situational task 01-14
Organ of vision - eye
consists of the eyeball, connected through the optic nerve to the brain, and an auxiliary apparatus, including the eyelids, lacrimal apparatus, and striated oculomotor muscles.
Functionally, there are three main apparatuses in the eyeball:
- diopter or light refractive apparatus
- button, fluid of the anterior chamber of the eye, lens, fluid of the posterior chamber of the eye and vitreous body; - accommodation apparatus
- iris, ciliary body with ciliary band - receptor apparatus
- retina.
The structure of the eyeball has three membranes: the outer fibrous membrane - the sclera and cornea; choroid - middle with the choroid itself, the ciliary body and the iris; and internal (sensory) - reticular. The eyeball also includes the lens, vitreous body and fluid of the anterior and posterior chambers of the eye.
The eye develops from several sources: the rudiments of the neural tube, ectoderm and mesenchyme (Table 1.)
Fibrous membrane
- the outer shell of the eye, performs protective and supporting functions. It is represented by an opaque sclera - a dense lamellar connective tissue that passes into the transparent cornea in the front part of the eye. At the junction of the sclera and the cornea there are small cavities that communicate with each other. This is the helmet canal - the venous sinus of the crypts.
Choroid
- the middle layer of the eye, the basis of which is loose connective tissue with blood vessels and pigment cells. This membrane is divided into three parts: the choroid proper, the ciliary body and the iris. The choroid itself plays a trophic role. There are four layers in it: the supravascular plate, the vascular plate, in the loose connective tissue of which many arteries lie. veins, pigment cells, B also separate bundles of smooth myocytes; a vascular-capillary plate with hemocapillaries of a predominantly sinusoidal type and a basal complex at the border between the choroid and the pigment layer of the retina.
Retina.
Its outer and inner layers develop from the corresponding walls of the optic cup, and the optic nerve is formed from neurites of retinal ganglion cells that penetrate the optic stalk. The lens develops from the ectoderm. The sclera and choroid are of mesenchymal origin. Mesenchyme, blood vessels and the embryonic retina take part in the development of the vitreous body and iris. The muscles that constrict and dilate the pupil are of normal origin.
Information from the situational task: (see entire task)
<�…> Retina
- This is the inner layer of the eye that provides light perception. Its visual part, located on the back wall of the eye, consists of neurons, neuroglia, pigment epithelium and blood vessels. The retina has a layered structure. It has 10 layers. The retina is divided into: an outer layer, represented by the pigment epithelium, and an inner layer - photosensitive, formed by the remaining layers of the retina and consisting of a chain of three neurons. The cell bodies of these neurons are located in the nuclear layers.
- pigment epithelium
, bordering the choroid, penetrates with its processes into the next layer of the retina - layer of rods and cones
, formed by peripheral processes of photosensory cells - outer glial limiting membrane
- outer nuclear layer
- formed by the nucleated parts of photosensory cells - outer reticular layer
- synapses between photosensory cells (their central processes) and bipolar cells (their peripheral processes) - inner nuclear layer, formed by the nucleated parts of bipolar cells
- inner reticular layer
, formed by synapses between bipolar and ganglion cells - ganglion layer
, represented by the bodies of multipolar ganglion cells - layer of nerve fibers
, formed by the axons of ganglion cells that form the optic nerve - internal glial limiting membrane
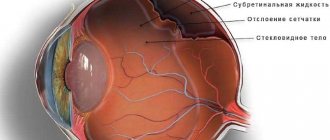
The retinal pigment epithelium performs a number of functions, without which light perception of the retina is impossible: delivery of vitamin A to photosensory cells, nutrition of the outer layers of the retina, phagocytosis of the outer segments of photoreceptors, shielding of receptors in light, preventing excessive illumination of receptors. The pigment epithelium is firmly associated with the basal lamina of the choroid on which it is located. The pigment epithelium develops from the outer layer of the optic cup. But the pigment epithelium is less firmly connected with the adjacent layer of photosensory cells originating from the inner layer of the optic cup. This circumstance explains the localization of retinal detachment at the border of the outer and inner layers of the retina. Retinal detachment leads to the death of photosensory elements.
Retina
The retina consists of a posterior light-receiving part (the visual part of the retina, pars optica retinae) and an anterior part that is insensitive to light (the ciliary part, pars ciliaris and the iris part, pars iridica). The boundary between the two parts of the retina is the serrated margin (ora serrata), which runs along the posterior border of the ciliary body. The ciliary and iris retina are simple epithelium covering the ciliary body and the posterior surface of the iris, respectively. In the place where the epithelium covers the iris, it is intensely pigmented.
The visual part of the retina covers the entire back of the eyeball and consists of two layers: the outer pigmented epithelium (pars pigmentosa) and the inner light-receiving layer (pars nervosa). The simple pigmented epithelium is closely adjacent to the choroid and contains elongated brown pigment granules. The cells of the pigment layer form processes of various shapes that extend into the nerve layer to the photoreceptors. Their main function is to feed photoreceptors. The light-receiving part of the retina contains three layers of neurons that transmit visual information. In the direction from the outer layer of the retina inwards are located:
- first order neurons , i.e. photoreceptors (rods and cones; stratum neuroepitheliale retinae); - second order neurons , i.e. bipolar cells (stratum ganglionare retinae); - third-order neurons , i.e. ganglion cells (stratum ganglionare nervi optici).
Anatomists divide the retina into 10 layers, although the boundaries between adjacent layers are very vague. The division into layers is based on the content of nerve elements in them, located at a certain depth.
Posterior wall of the eye - MGMSU named after. A.I. Evdokimova
17. Posterior wall of the eye
VIDEO
Histological specimen. No. 17 Posterior wall of the eye.
Hematoxylin and eosin staining. Magnification is small and large. Find:
- sclera;
- choroid with vessels and pigmentocytes;
- retina, and in it:
- pigment layer;
- layer of rods and cones;
- outer glial limiting membrane;
- outer nuclear (granular) layer;
- outer mesh layer;
- inner mesh layer;
- ganglion layer;
- layer of nerve fibers;
- internal limiting membrane.
Additional material
VIDEO I
Situational task 01-14
Organ of vision - eye
consists of the eyeball, connected through the optic nerve to the brain, and an auxiliary apparatus, including the eyelids, lacrimal apparatus, and striated oculomotor muscles.
Functionally, there are three main apparatuses in the eyeball:
The structure of the eyeball has three membranes: the outer fibrous membrane - the sclera and the cornea; choroid - middle with the choroid itself, the ciliary body and the iris; and internal (sensory) - reticular. The eyeball also includes the lens, vitreous body and fluid of the anterior and posterior chambers of the eye.
The eye develops from several sources: the rudiments of the neural tube, ectoderm and mesenchyme (Table 1.)
Fibrous membrane
- the outer shell of the eye, performs protective and supporting functions. It is represented by an opaque sclera - a dense lamellar connective tissue that passes into the transparent cornea in the front part of the eye. At the junction of the sclera and the cornea there are small cavities that communicate with each other. This is the helmet canal - the venous sinus of the crypts.
Choroid
- the middle layer of the eye, the basis of which is loose connective tissue with blood vessels and pigment cells. This membrane is divided into three parts: the choroid proper, the ciliary body and the iris. The choroid itself plays a trophic role. There are four layers in it: the supravascular plate, the vascular plate, in the loose connective tissue of which many arteries lie. veins, pigment cells, B also separate bundles of smooth myocytes; a vascular-capillary plate with hemocapillaries of a predominantly sinusoidal type and a basal complex at the border between the choroid and the pigment layer of the retina.
Retina.
Its outer and inner layers develop from the corresponding walls of the optic cup, and the optic nerve is formed from neurites of retinal ganglion cells that penetrate the optic stalk. The lens develops from the ectoderm. The sclera and choroid are of mesenchymal origin. Mesenchyme, blood vessels and the embryonic retina take part in the development of the vitreous body and iris. The muscles that constrict and dilate the pupil are of normal origin.
Information from the situational task: (see entire task)
<�…> Retina
- This is the inner layer of the eye that provides light perception. Its visual part, located on the back wall of the eye, consists of neurons, neuroglia, pigment epithelium and blood vessels. The retina has a layered structure. It has 10 layers. The retina is divided into: an outer layer, represented by the pigment epithelium, and an inner layer - photosensitive, formed by the remaining layers of the retina and consisting of a chain of three neurons. The cell bodies of these neurons are located in the nuclear layers.
- pigment epithelium
, bordering the choroid, penetrates with its processes into the next layer of the retina - layer of rods and cones
, formed by peripheral processes of photosensory cells - outer glial limiting membrane
- outer nuclear layer
- formed by the nucleated parts of photosensory cells - outer reticular layer
- synapses between photosensory cells (their central processes) and bipolar cells (their peripheral processes) - inner nuclear layer, formed by the nucleated parts of bipolar cells
- inner reticular layer
, formed by synapses between bipolar and ganglion cells - ganglion layer
, represented by the bodies of multipolar ganglion cells - layer of nerve fibers
, formed by the axons of ganglion cells that form the optic nerve - internal glial limiting membrane
The retinal pigment epithelium performs a number of functions, without which light perception of the retina is impossible: delivery of vitamin A to photosensory cells, nutrition of the outer layers of the retina, phagocytosis of the outer segments of photoreceptors, shielding of receptors in light, preventing excessive illumination of receptors. The pigment epithelium is firmly associated with the basal lamina of the choroid on which it is located. The pigment epithelium develops from the outer layer of the optic cup. But the pigment epithelium is less firmly connected with the adjacent layer of photosensory cells originating from the inner layer of the optic cup. This circumstance explains the localization of retinal detachment at the border of the outer and inner layers of the retina. Retinal detachment leads to the death of photosensory elements.
Manual of MGMSU in PDF format - download and read from page 21 (Sense organs. Organ of vision.) Manual of MGMSU. Private histology.
Read other manuals
Textbook “Private histology” V.L. Bykov pages from 214 to 226 for self-study
Rods and cones
The light-receiving photoreceptors, rods and cones, are located in the outermost layer of the retina, in contact with the pigment layer, and are hidden under the inner layers of nerve cells. Thus, before reaching the light-receiving cells, light must first pass through the inner layers of the retina. For this reason, the retina of the eye is sometimes called “inverted.”
Light-perceiving sensory cells number about 120 million rods (providing black-and-white vision in low light) and about 6 million cones (color vision). They form synapses on bipolar neurons of the retina (2nd order neurons), the axons of which in turn end with synapses on ganglion cells (3rd order neurons). There are significantly fewer bipolar and ganglion cells than receptor cells. As a result, impulses from several receptor cells converge on one bipolar or ganglion cell (convergent impulse conduction).
Yellow spot (macula lutea)
In the macula area, the retina is practically devoid of blood vessels and forms a depression located approximately 4 mm lateral to the optic disc. It contains the central fovea (fovea centralis), in which only cones can be found. The remaining layers of the retina in this place are moved apart, and therefore the incident light falls directly on the sensory cells, as a result of which the macula with the central fovea is the area of the clearest vision.
The fundus is normal
Diagnostics
In publications and at scientific conferences, experts note the difficulties of early diagnosis of posterior capsular fibrosis. Occasionally, its presence can be detected already during surgery (in this case it can hardly be considered a postoperative complication), but much more often the opacification is detected some time after IOL implantation. At the same time, the patient’s complaints, as well as the data of an objective study, do not allow us to clearly determine whether this is a side effect of surgical intervention, or natural (but too intense) fibrosis as a consequence of amputation of an element provided by nature, or a pathological reaction to the presence of a biocompatible, but still a foreign body, or, finally, this is a purely optical aberration caused by defects or poorly selected parameters of the lens itself (especially if it is a complex multifocal model).
Leading experts in the field call this situation “puzzling”; according to them, you can “remove the lens and not solve the problem” (if the clouding was initially of an endogenous-organic nature) or, conversely, perform repeated corrective microsurgical intervention on the capsule - and as a result you will still “get a dissatisfied patient” if the source of the symptoms is in was actually an IOL.
Fundus (fundus)
The fundus can be directly seen with an ophthalmoscope and is red-orange in color. The optic disc, where all the nerve fibers come together and exit the eye, lies on the nasal half. The central retinal artery enters the middle of the disc and divides into several branches, some of which go to the macula. The darker, wider veins join to form the central retinal vein and also exit the retina through the optic disc. An ophthalmoscopic examination allows the doctor to see the vessels and determine the condition of the retina.
How long have you been to a massage therapist? Come to massage courses. Saint Petersburg