Kidney tumors
Kidney tumors account for 2-3% of all neoplasms. They are approximately 2 times more common in men than in women. Kidney cancer accounts for 5-6% of all urological diseases. The peak incidence occurs between 40 and 60 years of age. The incidence of kidney cancer increases from south to north and from east to west and in the Scandinavian countries and North America is 5-6 times higher than in Asia and Africa.
Risk factors for developing kidney cancer are excess body weight, smoking, long-term use of estrogens in men, contact with asbestos, employment in the tanning industry, and long-term hemodialysis.
Histologically, according to the classification of tumors and tumor-like formations of the kidneys, they are distinguished:
1. Epithelial tumors of the renal parenchyma:
- adenoma;
- cancer.
2. Epithelial tumors of the renal pelvis:
- transitional cell papilloma;
- transitional cell carcinoma;
- squamous cell carcinoma;
- adenocarcinoma.
3. Nephroblastic tumors:
- nephroblastoma;
- typical nephroblastoma;
- epithelial nephroblastoma;
- mesenchymal nephroblastoma;
- mesoblastic nephroma.
4. Nonepithelial tumors:
- benign (angiomyolipoma and others);
- malignant.
5. Mixed group:
- juxtaglomerular cell tumor;
- neuroblastoma and ganglioneuroma.
6. Secondary tumors.
7. Unclassified tumors.
8. Tumor-like processes:
- renal dysgenesis;
- vascular malformations;
- cysts;
- renal tubular hyperplasia;
- xanthogranulomatous pyelonephritis and malakoplakia;
- others.
Classification of kidney tumors according to the TMN system:
- T1 - the tumor is palpable, located in the center of the parenchyma, can only be detected by x-ray;
- T2 - the kidney with the tumor is palpable, but the tumor has not yet invaded the surrounding tissues;
- T3 - the tumor grows into the surrounding tissues, due to which the mobility of the organ is limited;
- T4 - the kidney and tumor are motionless, there are distant metastases.
The letter M denotes distant metastases to other organs, and N denotes metastases to regional lymph nodes. Metastases to regional lymph nodes do not occur at stage I of the process and not always at stage II. In stages III and IV, metastases in regional lymph nodes, as a rule, always occur.
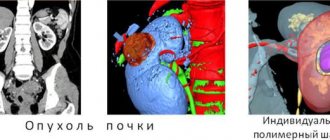
Macroscopically, most often the kidney is tuberous due to protrusion of tumor-like nodes. On a section, the tumor has a variegated color (yellow-brown, red, gray, etc.). Histologically, kidney cancer consists of light brown, granular cell alveolar, fusiform, solid tubular, polygonal and other cells.
Malignant kidney tumors metastasize by hematogenous (through blood vessels) and lymphogenous routes. Metastases are observed in more than half of patients. The first place in the frequency of metastasis of kidney cancer is the lungs, then the bones, liver, and brain. This pattern is due to the presence of a close connection between the venous system of the kidney and the main vessels of the thoracic and abdominal cavities, as well as the venous network of the skeleton.
Often, kidney cancer metastases manifest clinically earlier than the primary site of the disease. A feature of kidney cancer is the relatively frequent appearance of metastases many years (10-15 and even 20) after removal of the primary tumor. At the same time, another feature of this type of cancer is that its pulmonary metastases in some cases tend to regress after removal of the primary lesion.
In second place in frequency among distant metastases of kidney tumors are bone metastases, which are most often localized in the pelvic bones, spine, ribs, bones of the shoulder girdle, femurs, and cranial vault. Metastases to the liver are observed in the later stages of the disease.
Regional metastases of kidney cancer mainly affect the paracaval and para-aortic lymph nodes.
In addition to distant and regional lymphatic metastases, kidney cancer metastasizes outside the lymph nodes into the perinephric fatty tissue, abdominal muscles, subcutaneous fatty tissue, and into the postoperative scar. In this case, it is not tumor germination that is noted, but the presence of separate, clearly demarcated foci of metastasis. In addition to metastasis of kidney cancer, tumor thrombus spread through the renal vein into the inferior vena cava is often observed.
The clinical manifestations of kidney cancer are very diverse.
There are renal and extrarenal symptoms. The classic triad of renal symptoms of kidney cancer - hematuria, palpable tumor and pain - occurs in 10% of patients and indicates an advanced process - about half of these patients have distant metastases at the time of diagnosis. One or two symptoms from the triad are more common.
One of the most common symptoms is hematuria, observed in 50-60% of patients, and in half of them this symptom is the first sign of the disease. Hematuria is always total, occurs suddenly, against the background of complete health, and is often not accompanied by pain. The occurrence of acute pain after intense hematuria is characteristic of tumor damage to the kidneys and is associated with obstruction of the ureter by blood clots. In non-tumor diseases also accompanied by hematuria (renal stones, hydronephrosis), pain usually precedes hematuria. Another characteristic feature of hematuria in kidney cancer is its intermittent nature with a tendency to shorten the intervals between repeated bleedings. There is no strict relationship between tumor size and the intensity of hematuria. A small tumor can be a source of massive hematuria.
The second most common symptom is pain in the lumbar region, occurring in 50% of patients. The nature of pain can be very diverse, and the occurrence of dull, intense pain of a radicular nature is an unfavorable prognostic sign.
A palpable tumor is detected in 30-40% of patients, and this symptom is rarely the only one and is usually combined with other complaints.
Of the extrarenal symptoms, fever is the most common, which in 4-6% of patients may be the only manifestation of the disease. Among the general symptoms of a kidney tumor, the deterioration of the general condition as a result of intoxication of the body with metabolic products in the tumor tissue is important. In this case, general weakness, loss of appetite, and weight loss are noted. Patients with such complaints are treated for a long time for a variety of suspected diseases before the idea arises of the need for a urological examination.
Weight loss as a manifestation of the tumor process is a consequence of the toxic effects of tumor decay products on the body. Intoxication leads to a decrease in appetite, which in turn causes weight loss. Weight loss is most often a sign of an advanced blastomatous process.
An important symptom of a general kidney tumor is an increase in body temperature. This symptom is observed in 20-30% of patients with kidney cancer. Sometimes an increase in body temperature is the only manifestation of the disease. Body temperature is often around 37 °C, but sometimes reaches 38-39 °C, accompanied by chills, simulating an acute infectious disease.
The toxic effect of a kidney tumor on the bone marrow leads to inhibition of its function and the occurrence of anemia, which is evidence of an advanced tumor process. The manifestation of a kidney tumor may be polycythemia or secondary erythrocytosis. This process is explained by increased production of erythropoietin by kidney tumor tissue. The most common general sign of a kidney tumor is an increase in ESR, which may be the first and only manifestation of the disease. In 5-10% of patients with malignant neoplasms of the kidney, the disease manifests itself as arterial hypertension.
An important local sign of a kidney tumor is a varicocele. Its causes in case of a malignant kidney tumor can be:
- compression of the left renal vein or its invasion by a tumor;
- bending of the left renal vein as a result of downward displacement of the kidney;
- compression of the inferior vena cava or directly one of the testicular veins by a tumor or packets of lymph nodes affected by metastases;
- thrombosis of the inferior vena cava.
Symptoms of kidney tumor metastases are varied. Metastases of kidney cancer to the lungs are often radiographically round in shape. Sometimes metastasis of kidney cancer to the lung, especially with a solitary tumor, progresses for a long time and is not clinically manifested. This situation is convenient for its prompt removal. The first clinical manifestation of kidney tumor metastases to the lung is hemoptysis. Metastases of a solitary tumor are often disguised radiographically as bronchogenic cancer, and multiple metastases may resemble the picture of pneumonia or pulmonary tuberculosis.
Metastases of a kidney tumor to the bone are clinically most often manifested by pain, often very intense and persistent, which does not subside even with narcotic drugs. Sometimes such pain is regarded as a symptom of radiculitis, intercostal neuralgia, etc. With metastasis to the spine, lower paraplegia and dysfunction of the pelvic organs may develop. The first symptom of the disease may be a pathological fracture at the site of metastasis. The most typical localization of bone metastases is the diaphyses of tubular bones (shoulder, femur), as well as flat bones - ribs, scapula, skull. A characteristic radiological sign of metastases of hypernephroid cancer in the bone is the osteolytic type of pathological process. Features of RP include the appearance in some cases of metastases many years after removal of the primary
Diagnostics. Upon examination and palpation, only advanced kidney tumors are usually detected. Upon examination, a varicocele can be detected, and with obstruction of the inferior vena cava, dilation of the veins of the anterior abdominal wall and swelling of the lower extremities.
Palpation of the kidney - the degree of mobility of the tumor or kidney during palpation to a certain extent serves as an indicator of operability.
Laboratory diagnostic methods include general blood and urine tests, biochemical and immunological studies. General blood tests reveal changes that are specific not only to kidney cancer: increased ESR, anemia. Urine tests reveal erythrocyturia. Proteinuria and leukocyturia may be observed, especially when a kidney tumor is combined with pyelonephritis.
Of the biochemical research methods, the most widely used are the study of enzymes, proteins and protein fractions, determination of calcium content in serum, and the Danilin reaction. Characteristic nonspecific signs for primary kidney cancer are increased activity of alkaline phosphatase and a number of other enzymes in the blood serum, increased levels of alpha2-globulin (Stauffer syndrome).
Recently, immunological methods have been used to diagnose kidney cancer. Using classical methods of immunodiffusion analysis (radial immunodiffusion reaction, immunoelectrophoresis, counter immunophoresis, double immunodiffusion according to Ouchterlony, etc.), it is possible to identify profound disorders in the metabolism of serum proteins; ferritin, transferrin, albumin, etc.
It has been established that kidney tumor tissue selectively accumulates ferritin. This protein is found in tumor tissue 10-220 times higher in concentration than in normal kidneys and cancerous tumors of other organs. The level of another iron-containing protein, transferrin, in the tumor tissue of the kidney is increased 3 times. These characteristic changes occur in the protein spectrum of the blood in 80% of patients. After nephrectomy, patients showed a tendency towards normalization of these indicators, which is evidence that the changes in serum proteins described above are pathognomonic for kidney cancer.
Taking into account the data obtained, it should be considered that an immunological examination if a kidney tumor is suspected should be a mandatory stage of a comprehensive examination of the patient.
In recent years, much attention has been paid to radioisotope diagnostics of kidney tumors. For this purpose, static nephroscintigraphy (or kidney scanning) is used.
Ultrasound scanning is widely used in oncourology for the diagnosis of tumors and kidney cysts. The method is harmless, safe, does not require preliminary preparation of the patient and has high diagnostic information content.
Ultrasonograms of a tumor are composed of pictures obtained after reflection of sound from dense inhomogeneous tumor tissues, blood vessels, hemorrhages, necrotic tissues, each of which has an acoustically demarcated surface. Thus, in the presence of a tumor, the contours of the kidney are deformed, and many echo signals appear inside the tumor due to uneven absorption of sound by the tumor. Ultrasound examination (ultrasound) can detect venous thrombosis, tumor ingrowth into blood vessels, and enlarged regional lymph nodes (LN), which makes it possible to determine adequate treatment tactics.
Ultrasound scanning of the kidney plays an important role in the differential diagnosis of a kidney tumor with pyonephrosis, hydronephrosis, polycystic kidney disease, and especially with a solitary kidney cyst. On scanograms, the cyst has a capsule with an even contour, inside of which there is a zone free from echo signals.
Despite the introduction of the above methods into clinical practice, the final stage in diagnosing a kidney tumor is an x-ray examination. Various x-ray methods are used to recognize the tumor process of the kidney.
An X-ray examination of the patient begins with a survey urography, which reveals changes in the configuration of the kidney and its position, and petrification in the tumor tissue. In some cases, when it is impossible to judge the contours of the kidney from a plain radiograph, they resort to tomography or pneumo-retroperitoneum, with the help of which a more relief image of the kidney shadow is obtained.
Excretory urography makes it possible to clarify both the functional and morphological features of the kidney affected by the tumor, and, in addition, to identify the condition of the opposite kidney. The function of the tumor-affected kidney in the initial stages of the disease remains quite satisfactory. The lack of function indicates an advanced blastomatous process, significant replacement of the kidney parenchyma with tumor tissue or infiltration of the renal pedicle or compression of it by packages of lymph nodes affected by metastases.
Abdominal aortography should be the first stage of renal angiography, at which the type of vascularization of the affected kidney is determined (single, double or accessory artery), the tumor is recognized, the nature of its growth (inward or outward), its relationship with surrounding organs, the presence of metastases in the opposite kidney , liver. Depending on the nature of vascularization, kidney tumors can be divided into two groups: avascular or hypovascular and hypervascular. The first group includes adenoma, adenocarcinoma, and kidney metastases. Hypervascular include most variants of renal cell carcinoma, which have a typical angiographic picture due to abundantly developed pathological vessels in the tumor.
Signs of a tumor are: expansion of the lumen of the main renal artery, disordered pathological vascularization in the tumor mass (a cobweb-like mesh in the tumor area and accumulation of radiopaque substance in the form of “lakes”, “puddles”, premature segmental nephrogram or image of the renal vein in the early arterial phase, increased shadow tumor mass, the presence of translucent lacunae and inhomogeneity of the shadow of the mass (tumor necrosis), etc.
Serial aortography is especially informative in this regard. The serial imaging program must be designed to obtain the early arterial phase to capture signs of fistula blood supply to the affected kidney.
Selective renal arteriography should be performed if it is necessary to clarify aortographic data.
If the presence of a tumor thrombus is suspected, inferior cavography and selective renal venography are the most informative.
Differential diagnosis
The greatest difficulties arise in the differential diagnosis of kidney cancer with small benign tumors, which make up 5-9% of all kidney tumors. Of the benign epithelial tumors, adenoma and oncocytoma are of greatest importance. Of the benign epithelial tumors of the kidney, adenoma is most often detected. This tumor is rare in people under 40 years of age and is observed in men 3-4 times more often than in women. A rare epithelial tumor of the kidney is
Kidney adenoma is represented by monomorphic cells with a correctly formed nucleus. The scanty cytoplasm of cells can be light or granular, or a combination of both mentioned characteristics. The tumor is delimited from the surrounding tissue, but is not surrounded by a capsule. Adenomas may be compact or contain cysts of varying sizes. Tumor cells form tubular or papillary structures. An adenoma is capable of invasive growth and metastasis, therefore it is proposed to regard a kidney adenoma larger than 2 cm as a malignant tumor and choose the appropriate treatment method.
Kidney adenomas usually do not appear clinically and are diagnosed accidentally. Ultrasound and computed tomography do not have reliable differential diagnostic features; with angiography, the tumor is most often avascular or hypovascular. Considering the difficulties of differential histological diagnosis of adenoma and cancer, renal adenomas larger than 3 cm of any degree of atypia are classified as cancer. In turn, adenomas include tumors of grade I atypia up to 3 cm in size.
Treatment: surgical
The term “oncocytoma” refers to a well-differentiated eosinophilic granular cell tumor of the renal parenchyma, consisting of oncocytes. In some cases, all cellular elements of the tumor or part of them have sharply eosinophilic fine-grained cytoplasm, rich in mitochondria, i.e. are so-called oncocytes.
A characteristic feature of oncocytes is their loss of organ-specific features. Tumors consisting of such cells can reach large sizes and appear as a node, clearly demarcated from the surrounding kidney tissue, with a brownish surface when cut, often with a scar in the center. In the differential diagnosis of oncocytoma, one should take into account the homogeneous appearance of the tumor, the absence of foci of necrosis and hemorrhages, as well as yellow areas characteristic of cancer.
The admixture of Sudan-positive cells in oncocytomas indicates the presence of fatty inclusions in the cells and indicates renal cell carcinoma. An important feature that allows differentiating oncocytoma from cancer is the absence of mitoses even with pronounced polymorphism of the tumor.
Clinical manifestations of oncocytoma occur when the tumor reaches a large size. Symptoms are more sparse than with renal cell carcinoma. In the angiographic diagnosis of oncocytoma, the “bicycle wheel with spokes” pattern, the absence of pathological vascularization, and the presence of a capsule or pseudocapsule are considered specific. In other cases, the picture of renal oncocytoma is indistinguishable from that of kidney cancer. The final understanding of renal oncocytoma has not yet been developed; treatment consists of kidney resection or nephrectomy, which is determined by the size and location of the tumor.
The next most common benign tumor is a mesenchymal tumor - angiomyolipoma. Its frequency is 0.3-5% of all kidney tumors, occurs 4 times more often in women than in men, and is diagnosed mainly at the age of 35-65 years. The tumor consists of tissues normally found in the kidney, but present in different proportions both in tissue structure and degree of maturity, and is therefore sometimes called a hamartoma. Angiomyolipoma is represented by fat cells, proliferations of smooth muscle cells and tortuous vessels, and their ratio can be different, to the point that in some cases the tumor in its composition is close to a single component - lipoma, leiomyoma or hemangioma.
Angiomyolipoma of the kidney occurs in 80% of patients with tuberous sclerosis (Bourneville disease), a congenital hereditary disease transmitted in an autosomal dominant manner. Such patients suffer from epilepsy and retarded mental development; they often have multiple tumors of organs of ectodermal origin (brain, retina, skin) and angiomyolipomas of organs of mesenchymal origin.
There are two clinical forms of the tumor. The first is often observed in combination with tuberous sclerosis, is detected at a young age, and is characterized by multiple bilateral lesions. The second form is detected in adulthood (40-60 years); Tumor nodes are usually unilateral and can reach large sizes. The ratio of men to women in any form is 1:4.
The clinical picture is dominated by pain, which is the result of hemorrhage into the tumor, which in some cases is accompanied by a picture of hypovolemic shock and acute abdomen. Gross hematuria is rare. Alternating multiple areas containing fat create a unique combination of hyperechogenicity on ultrasound and well-defined fatty inclusions on computed tomography, specific only to renal angiomyolipoma. A final opinion regarding treatment tactics has not been formed; tactics depend on the size of the tumor, clinical manifestations, and the presence of intercurrent diseases. For small asymptomatic angiomyolipomas, apparently, we can limit ourselves to observation. For large tumors, the treatment of choice is partial nephrectomy or nephrectomy.
In difficult diagnostic cases, percutaneous puncture biopsy of a renal tumor under the control of ultrasound or computed tomography is possible, which in 70% of cases makes it possible to make a morphological diagnosis.
Fibroids most often occur in the medulla of the kidneys. It is assumed that fibromas of this localization arise from the interstitial cells of the medulla and may have the ability to produce antihypertensive substances.
Hemangioma most often occurs in the wall of the renal pelvis, but can also occur in the area of the kidney pyramids. In a removed kidney, detection of hemangiomas is difficult due to the collapse of blood vessels.
Juxtaglomerular cell tumor consists of cells of the juxtaglomerular apparatus. This tumor is renin-secreting and consists of small cells that form fields and cords with perivascular orientation of cellular elements. The morphological determination of this type of tumor is based on the detection of renin secretion and diamond-shaped inclusions in the cytoplasm during electron microscopic examination.
In case of hydronephrosis, a tumor-like formation in the hypochondrium is palpated, but its consistency is tight-elastic, the surface is smooth, and hematuria is rarely observed. The pyelographic picture of hydronephrotic transformation differs sharply from the deformation of the pyelocaliceal system by the tumor. Renal arteriograms reveal narrowing of the lumen of the renal artery and its branches.
Polycystic kidney disease simulates a tumor in the case of its asymmetric development, when only one enlarged dense tuberous kidney is palpated. Suspicion of the presence of a tumor increases with hematuria. However, polycystic disease is characterized by chronic renal failure of one stage or another, and most importantly, a pathognomonic pyelographic pattern of bilateral changes, increased branching of the calyces, compression and elongation of the pelvis. On arteriograms, polycystic disease is characterized by the presence of many round avascular areas and elongated thinned arteries.
With a carbuncle (less often an abscess) of the kidney, suspicion of the presence of a tumor usually arises in connection with a similar x-ray picture (deformation, displacement of the pyelocaliceal system, amputation of the calyces). On scintiscanograms, the manifestations of the tumor and the renal carbuncle are also similar (focal defect in isotope accumulation). In addition, all clinical and laboratory signs of an acute inflammatory process (fever with chills, leukocytosis) not only do not exclude a kidney tumor, but are also quite characteristic of its symptoms. Renal arteriography brings clarity to the differential diagnosis in these cases.
Differential diagnosis of a tumor and kidney tuberculosis is carried out in a similar way.
Differential diagnosis of a kidney tumor and a retroperitoneal tumor can be very difficult. Palpation data for these diseases are the same. Using excretory urography and retrograde pyelography (preferably in combination with pneumoretroperitoneum and tomography), in case of a retroperitoneal tumor, displacement of the kidney is detected without deformation of the pyelocaliceal system and an image of a separately located tumor is obtained. Characteristic of a retroperitoneal tumor is deviation of the ureter in the medial direction.
Wilms tumor (nephroblastoma) accounts for 1/3 of all tumors in children and ranks first among all tumors in childhood. Children aged 2-5 years are most often affected. Girls and boys get sick equally often. Nephroblastoma is the result of a violation of kidney embryogenesis in the third period - the metanephros stage. In 1899, Wilsm indicated that these tumors were of mesodermal origin. According to his opinion, some mesoderm cells do not differentiate, but grow randomly and epithelial and connective tissue elements arise from them. Tumors range from 400 g to 12 or more kilograms.
Macroscopically, Wilms tumor consists of cavities with fluid or a gelatinous mass and dense tissue that looks like fish meat. Histologically, smooth and striated muscle fibers, cartilage, nerve formations, and epithelial cells can be identified.
Based on the degree of malignancy and histological structure, Hardwick and Stones distinguish 6 types of Wilms tumors. According to the degree of tumor spread and metastasis, 4 stages of the process are distinguished:
- Stage I - tumor in the capsule;
- Stage II - the tumor has grown into the capsule and there are metastases in the lymph nodes;
- Stage III - the tumor grows into neighboring organs;
- Stage IV - there are metastases to distant organs.
Early symptoms of Williams tumor include malaise, adynamia, irritability, capriciousness of the child, pallor of the skin, subfibrile temperature, periodic abdominal pain, traces of protein in the urine, and high ESR. These symptoms are not typical and do not always suggest a kidney tumor. Only the appearance of hematuria and the detection of a tumor in the abdominal cavity indicates kidney damage. It can compress the inferior vena cava or portal vein, which causes ascites or edema in the lower extremities. Hematuria occurs in 60-65% of cases, usually in the later stages of the process. A common symptom is hypertension, which is caused by compression of the renal parenchyma by a growing tumor.
Diagnosis of Wilms tumor is based on identifying clinical signs and carrying out special research methods: survey and excretory urography allows us to identify an enlarged shadow of the kidney and defects in the filling of the pelvis and calyces, their compression. The application of retropneumoperitoneum makes it possible to more clearly see the enlarged shadow of the kidney on x-ray and tomograms. Isotope scanning and renography reveal areas of decreased isotope accumulation and an incorrect type of renographic curve. In difficult and doubtful diagnostic cases, aortography and selective renal arteriography are performed.
Differential diagnosis of Wilms tumor is made with liver diseases, intestinal tumors, genital tumors in girls, Hirschsprung's disease and other diseases.
The best results are obtained by combined treatment (surgery, radiation and chemotherapy). Tumor removal in children is performed transperitoneally. Radiation therapy is successfully combined with the use of antitumor antibiotics (actnomycin D, chrysomalin, bruniomycin), which potentiate the effect of radiation. Among the cytostatics, vicristin, cyclophosphamide, etc. are widely used.
Prognostically, a 2-3-year survival rate is noted in 40-45% of those operated on.
Forecast. With a kidney tumor, the prognosis depends primarily on the stage of the process. The worst long-term treatment results were recorded in patients with renal vein invasion and metastases.
The prognosis is especially poor in non-operated patients. As the primary tumor grows or metastases spread, their condition steadily worsens: general weakness and exhaustion increase, in many cases fever, hematuria, and severe pain are noted. Patients die from severe intoxication, cachexia, and anemia.
An important prognostic factor is the age of patients; among patients under 40 years of age, lower survival rate was observed than among older ones.
Main symptoms
For a long time, the disease can be asymptomatic. Over time, symptoms appear, the main ones being hematuria (blood in the urine), palpable swelling in the abdomen and pain. Hematuria usually appears suddenly and is short-term. Worm-shaped blood clots can often be found in the urine. You can palpate a tumor only if its size reaches 5 cm, but in overweight patients this is difficult to do even if the tumor is large. The pain is dull in nature and is noted on the affected side. In addition, the person is worried about weakness, fever, and arterial hypertension. As a result of compression of the inferior vena cava, swelling of the legs, dilation of the saphenous veins of the abdominal wall, and varicocele develop. When metastases spread to distant tissues and organs, symptoms characteristic of damage to a particular organ appear: cough and hemoptysis when the lungs are affected, pathological fractures and pain in the bones, jaundice when cancer cells spread to the liver, etc.
K. V. Puchkov: “Oncological disease is not a death sentence”
Therapeutic tactics for adrenal tumors
When identifying an adrenal tumor larger than 1 cm, it is first necessary to exclude or confirm the hormonal activity of the formation, which can manifest itself as hypercatecholaminemia, ACTH-independent hypercortisolism, and primary hyperaldosteronism.
At the second stage, to diagnose the malignant potential of a tumor, it is recommended to evaluate quantitative densitometric parameters using three-phase multislice CT:
- density of the tissue component before contrasting (native);
- density in the tissue phase of contrast (arterial and venous phases);
- density in the delayed (10 minutes after contrast administration) contrast phase (washout phase).
When obtaining high-density CT values in the native phase, contrast delays in the delayed phase - the malignant potential of the tumor should be assessed as high.
In the differential diagnosis of adrenal tumors, needle biopsy has no proven advantages and is associated with low sensitivity, specificity and a high likelihood of complications. The same thing seems to apply to such a diagnostic method as PET CT; it has been revealed that not all neuroendocrine malignant tumors of the adrenal gland accumulate a contrast agent, so this method is not specific and reliable, and can give a false-negative result.
Surgery for kidney cancer
Most medical institutions perform open removal of the entire kidney. However, for a small tumor, surgery can be performed while preserving the organ. Of course, if the tumor is large or located in the center, nephrectomy has to be performed - removal. However, in clinics in Europe and the USA, when treating kidney cancer, the “golden” standard is partial resection - removal of part of the kidney along with the tumor. And only if resection is impossible, nephrectomy is performed - removal of the kidney.
| Rice. 1. | Rice. 2. | Rice. 3. |
| Laparoscopic removal of a kidney tumor - resection within healthy tissue, suturing of the renal wound. | ||
STV: Scat. Master class by K. V. Puchkov
When performing minimally invasive surgery for kidney cancer, I always try to preserve the organ by performing laparoscopic resection. In this case, the kidney is isolated from the tissues surrounding it, then, using a special laparoscopic ultrasound sensor, the localization of the tumor in relation to the pelvis and renal vessels is specified (Fig. 1). In a favorable “surgical” situation, a kidney resection is performed - at a distance of 5-8 mm from the tumor, within healthy tissue, the formation is excised with ultrasonic scissors (Fig. 2). To suture the wound, synthetic absorbable threads are used, as well as hemostatic glue made in the USA and the PerClot hemostatic system (Italy), thanks to which the renal wound can be hermetically closed (Fig. 3).
In difficult cases, I use the V-lock suture system (Covidien, Switzerland), which is made of monofilament absorbable polydioxanone thread with notches on it. The notches are oriented in space at a given angle in one direction. This allows the thread to slide freely in one direction and be virtually unmovable in the opposite direction. Such systems fix fabrics using an anchor type and do not require tying knots. When using this suture system, there is a more thorough comparison of the edges of the wound on the uterus (which leads to even better healing) and the speed of suture formation increases by 3-4 times.
In addition, the use of anti-adhesive barriers and liquid media, as well as the use of modern compression hosiery for the prevention of thromboembolism and pulmonary embolism, can be considered a huge advantage for the prevention of the development of adhesive disease. After a year, as a rule, the site of the operation cannot be determined even with the help of ultrasound.
During laparoscopic nephrectomy
I make sure to remove all lymph nodes that may contain tumor cells. This step is extremely important, because it is impossible to exclude metastatic lesions of regional lymph nodes before surgery even using the most modern diagnostic method. If the lymph nodes affected by metastases are left, the process will progress. When mobilizing the kidney, modern ultrasonic surgical scissors are used, as well as an electrothermal dosed tissue ligation device “LigaSure” (USA) - thanks to which this stage of the operation is bloodless. The resected fragment with the tumor is removed from the peritoneal cavity in a special plastic container - this way contamination of the surrounding tissues with tumor cells can be avoided. At the same stage, an incision of about 4 cm is made on the abdominal wall.
I have extensive experience in minimally invasive surgical interventions; I have successfully performed about 500 operations for kidney tumors of various shapes - both benign and malignant. The results of the interventions are summarized in more than 20 scientific publications, which can be found in various peer-reviewed professional scientific publications, both in Russian and foreign.
I have been performing similar operations since 2000, during which time I have developed an original method of installing trocars during laparoscopic surgery on the kidney and retroperitoneum. This allows the instruments to be positioned at an optimal manipulation angle, so suturing the wound on the kidney during kidney resection and removal of lymph nodes during radical nephrectomy is easy and quick.
You can watch videos of operations performed by me on the website “Videos of operations by the best surgeons in the world.”
Patent for invention. A method for determining the optimal installation sites for manipulation trocars during laparoscopic operations on organs of the retroperitoneal space “Hand suture in endoscopic surgery”, K. V. Puchkov, D. S. Rodichenko
Knowing all the main methods of kidney surgery, having experience in successfully performing operations on cysts, benign tumors, as well as kidney cancer, I strive to select the optimal surgical treatment tactics in each specific case. The surgical techniques I use make it possible to perform operations using laparoscopic access that most surgeons perform only using open access, for example, during resection of a large cyst with a diameter of more than 10 cm or during nephrectomy for kidney cancer.
Today, my seminars on laparoscopic treatment of kidney tumors are attended by doctors - specialists from large scientific centers, hospitals of republican, regional or regional significance, as well as cadets of postgraduate education faculties.
For the development of methods of laparoscopic operations for the surgical treatment of kidney tumors, as well as other organs of the body, Professor Konstantin Viktorovich Puchkov was awarded one of the most prestigious awards in the field of surgery - “Golden Laparoscope”.