What is an adrenal adenoma?
Adrenal adenoma is a benign tumor that arises in the adrenal cortex.
Often in everyday life, doctors use the term “adenoma” to refer to all identified tumors of the adrenal gland, unless a malignant process is suspected. This is not entirely true, since it is almost impossible to confidently establish a diagnosis of adrenal adenoma before a full examination. If an unexpected tumor was detected in a patient’s adrenal gland by ultrasound or computed tomography, then it is recommended to use the special term “incidentaloma” (from the word incidental - random), i.e. accidentally discovered adrenal tumor. Incidentalomas can be structurally adrenal adenomas, pheochromocytomas, cysts, lipomas, myelolipomas, hemangiomas, teratomas, neurofibromas, adrenal cancer, sarcomas, metastases of other tumors to the adrenal gland. That is why, when a patient is diagnosed with an adrenal tumor, the doctor is simply obliged to refer the patient to a specialized center for endocrinology and endocrine surgery, where he will undergo a thorough examination. Only after a thorough examination and exclusion of the malignant nature of the adrenal tumor is it legitimate to use the term “adrenal adenoma”. On average, among incidental adrenal glands, hormonally inactive adenomas predominate, accounting for about 98%; adrenocortical cancer occurs in no more than 1% of patients. Incidentalomas of the adrenal glands can be detected in every 20th person on Earth (according to other sources - in every 10th).
An adrenal adenoma can be hormone-producing (i.e., producing certain hormones) and hormonally inactive (i.e., not producing any hormonal substances). Hormone-active adrenal adenomas are divided into corticosteromas (produce cortisol), aldosteromas (produce aldosterone), and androgen-producing adenomas or androsteromas (produce androgens).
Classification
There are three histological forms of adenoma: adrenocortical, pigmentary and oncocytic.
Under a microscope, they are all surrounded by a capsule of connective tissue, but differ from each other in color, cell shape and content. In most cases, adrenocortical adenoma occurs - a large single node with a diameter of 30-35 mm and weighing up to 40 g. It is one-sided and has a uniform yellow-brown color. Pigmented adenoma is less common, but has high functional activity. The mass of the tumor is no more than 35 g, the diameter is 3 cm. A distinctive feature is the dark color, indicating the presence of lipofuscin granules (brown pigment) in the cells.
Oncocytic - functionally inactive, has a reddish color and consists of large cells, therefore it gives the impression of granularity.
Adenomas can be hormonally active or inactive. Depending on this, the following types are distinguished:
- androsterome - produces androgens;
- corticoestroma - releases estrogens into the blood;
- corticosteroma - produces cortisol;
- incidentaloma - hormonally inactive.
According to another classification, adrenal adenomas are divided into those with a typical or atypical appearance. Typical tumors are homogeneous with low density and less than 3 cm in size. Adrenal microadenoma is a benign neoplasm no more than 10 mm in size. Atypical are adenomas whose size is more than 3 cm. With a diameter of 4 to 6 cm, the probability of malignancy is 7%, and with a size of more than 6 cm - 85%.
Symptoms of adrenal adenoma
Symptoms of an adrenal adenoma may be related to the size of the tumor or the production of hormones by the adenoma. Most often, adrenal adenomas are small in size (up to 4-5 cm), so they do not cause direct symptoms of compression of surrounding organs. In order for a tumor to be felt by the patient, compress the inferior vena cava, or cause any other problems, it must be 10 cm or more in size, and such adenomas almost never occur.
Hormonally inactive adrenal adenomas may not be accompanied by any symptoms at all. Such adenomas are most often discovered completely by accident, during an ultrasound or computed tomography scan of the abdominal cavity for any reason. Considering that in recent years the use of computed tomography has become widespread, and the quality of tomographic equipment in specialized centers has become very high, a significant number of patients with adrenal tumors have appeared - so significant that even the very idea of total removal of all adrenal tumors began to be perceived as unrealistic and unwise . There are so many patients with adrenal tumors that surgeons are simply not able to operate on them all, not to mention the fact that not all patients benefit from tumor removal.
Hormone-active adrenal adenomas, on the contrary, cause the patient a variety of very diverse symptoms, the specifics of which are determined by what hormone the adenoma produces.
Corticosteromas
(adrenal adenomas that produce cortisol) cause the patient to develop a number of symptoms referred to collectively as “Cushing’s syndrome” (as opposed to Cushing’s disease, which is caused by excess production of the hormone ACTH in the pituitary gland). Itsenko-Cushing syndrome occurs more often in women. Typical age is 20-40 years.
The main symptom of cortisol-producing adenoma is obesity
(observed in 90% of patients), and obesity has a specific, so-called Cushingoid type - fat is deposited on the chest, abdomen, neck and face. The patient develops a typical round face. Very typical is thinning of the skin and disappearance of subcutaneous fat on the back of the hand.
In the vast majority of patients, muscle atrophy
, which is most pronounced in the area of the shoulders and legs. The muscles of the buttocks atrophy, which, in combination with atrophy of the leg muscles, leads to difficulty getting up and difficulty moving due to increased load on the legs. In patients, the muscles of the anterior abdominal wall atrophy - this leads to the appearance of hernias and protrusion of the abdomen (“frog belly”).
A very characteristic symptom is atrophy and thinning of the skin
. One of the most clearly visible symptoms of hypercortisolism is the appearance of striae - purplish-red or purple stretch marks on the skin. Most often, stretch marks are found on the abdomen, inner thighs and shoulders, and on the mammary glands. The occurrence of small hemorrhages in the subcutaneous tissue is typical.
The most important and very common complication of cortisol-producing adrenal adenoma is osteoporosis.
– weakening of bone tissue associated with loss of mineral salts. Patients may notice a sharp decrease in the height of the vertebral bodies with the development of compression fractures. Osteoporosis can also be detected by densitometry. The development of osteoporosis leads to severe fractures, the most dangerous of which are hip fractures and spinal fractures.
Dysfunction of the nervous system is common - depression
, inhibition, but the appearance of psychotic reactions is also possible.
Steroid-induced diabetes mellitus occurs in 10-20% of patients with corticosteroma
, which is treated with diet and taking tableted hypoglycemic drugs.
Hirsutism often occurs in women with the development of Cushing's syndrome.
(excessive body hair growth) and
amenorrhea
(menstrual irregularities).
Aldosteroma
– adrenal adenoma that produces aldosterone. Leads to the development of primary hyperaldosteronism (PHA, Conn's syndrome). Most often, aldosteroma is small in size (up to 3 cm) and is not malignant. The production of aldosterone by the adrenal adenoma leads to sodium and fluid retention in the body, as a result of which the patient’s circulating blood volume increases and blood pressure rises. The main symptom of aldosteroma is an increase in blood pressure. Patients also develop increased loss of potassium in the urine, resulting in symptoms of decreased potassium levels in the blood (muscle weakness, cramps).
Androsteroma
(adrenal adenoma that produces androsterone, a male sex hormone). This tumor is also called virilizing adrenal adenoma, since it causes the appearance of virilization, i.e. the appearance of some signs characteristic of men in women. Women develop emphasized muscles, their voice becomes rougher, body hair begins to grow, and facial hair begins to grow, forming a beard and mustache. The size of the mammary glands decreases, the menstrual cycle is disrupted. There is an increase in the size of the clitoris. In men, the symptoms of androsteroma are most often invisible, which explains the often late diagnosis of this tumor.
Healthy foods for sick organs
The synthesis of hormones of the cortical and medulla of the adrenal glands occurs in the presence of the following components of the diet:
- vitamin E: vegetable oil, wheat germ, nuts, sunflower seeds;
- pantothenic acid (vitamin B 5): egg yolk, bran, peas, avocado, cheese;
- omega-3, -6, -9-unsaturated fatty acids: fish oil, seafood, broccoli, chia and flax seeds, walnuts;
- potassium, sodium, magnesium, iodine: kelp, sea salt, pink Himalayan salt;
- vitamin C: rose hips, black currants, sweet peppers, kiwi;
- tyrosine: turkey, pumpkin seeds, bananas, legumes, hard cheese.
Potassium in foods
It is important not only to provide the body with healthy foods, but also to minimize or eliminate those that disrupt hormonal balance:
- canned, smoked, industrially processed food with dyes, flavors and flavor enhancers;
- fast food, crackers with spices, chips, instant soups;
- ready-made sauces, juices, nectars;
- sweet soda, alcohol, energy drinks;
- coffee, especially instant coffee;
- margarine, sour cream and cheese products;
- shelf-stable yoghurts with sugar.
Junk food is the cause of many diseases
Adrenal adenoma - diagnosis
If the presence of an adrenal adenoma is suspected or if an adrenal tumor is accidentally detected during ultrasound or computed tomography, doctors are faced with two main tasks: to determine the structure of the tumor (benign tumor - adrenal adenoma or malignant tumor - adrenocotic carcinoma) and determine the presence or absence of hormonal activity of the detected tumor.
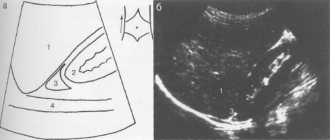
, computed tomography with intravenous contrast enhancement is most often used
. Computed tomography of the adrenal glands if an adenoma is suspected should be performed on a high-quality tomograph (optimally multislice, with a number of slices of 64 or 128). Initially, the size of the adrenal tumor and its density (the so-called native density) are assessed. Subsequently, the patient is given intravenous contrast and images are taken in the arterial and venous phases, as well as delayed images. Benign adrenal adenoma is characterized by a low native density, followed by active accumulation of contrast and its rapid and complete washing out from the tumor. On computed tomography, an adrenal adenoma is characterized by clear contours, usually small in size (up to 3-4 cm), although larger adenomas can also occur.
, magnetic resonance imaging can be used for diagnostic purposes.
, although it has less diagnostic value compared to computed tomography.
Biopsy of adrenal adenoma
is performed very rarely due to its traumatic nature and low diagnostic significance. The main purpose of an adrenal biopsy is to exclude metastatic damage to the adrenal gland by tumors of other organs.
The hormonal activity of an adrenal adenoma is assessed through a series of laboratory tests. Among the most informative studies, the following should be mentioned.
Determination of cortisol in daily urine
allows you to assess the basal production of cortisol by the adrenal glands. It is important to remember that determining the level of cortisol and ACTH in the blood does not clearly determine the hormonal function of the adrenal glands due to significant fluctuations throughout the day.
Small dexamethasone test
allows us to identify even mildly expressed signs of Itsenko-Cushing syndrome in the patient. When conducting a test on the first day, the patient's blood is taken in the morning to measure cortisol levels. At 24 hours of the same day, the patient takes a dexamethasone tablet at a dosage of 1 mg. The next morning, the patient is given a blood test for cortisol. Normally, the level of cortisol in the morning of the second day decreases by more than 2 times compared to the first day. In the absence of suppression of blood cortisol levels, we can conclude that there is an autonomous uncontrolled production of cortisol.
Large dexamethasone test
is carried out to distinguish between a cortisol-producing adrenal tumor (Cushing's syndrome) and an ACTH-producing pituitary tumor (Cushing's disease). For a large dexamethasone test, the patient takes 8 mg of dexamethasone in the evening. If a patient has a cortisol-producing adrenal adenoma, cortisol levels do not fall after a large dexamethasone test. In the presence of an ACTH-producing pituitary adenoma (Cushing's disease), the blood cortisol level decreases by 50% or more.
Blood test for renin, aldosterone, chromogranin A, ACTH, blood ions, calcitonin, parathyroid hormone
– another mandatory component of the survey.
Causes
Adrenal adenoma in women or men is not recorded very often. Why does the disease develop at all? There may be several reasons for this:
- some patients have a genetic predisposition to this type of tumor;
- the patient does not struggle with his excess weight;
- some hormonal changes may explain the appearance of adrenal adenoma in women;
- addiction to alcohol or smoking;
- the presence of other somatic diseases associated with problems in the body’s hormonal system (hypo- and hyperthyroidism, damage to the pituitary gland, diabetes mellitus).
Treatment of adrenal adenoma
If you are confident in the benign structure of the adrenal adenoma and its small size, as well as in the absence of hormonal activity of the adenoma, there are no indications for treatment. Such adrenal tumors are the most common and require only observation with periodic (at least once a year) computed tomography of the adrenal glands without contrast and blood sampling for cortisol and a number of other indicators. If during observation the adrenal adenoma does not grow in size and does not show signs of hormonal production, there are no indications for treatment at all.
In cases where the hormonal activity of the adenoma is established, or the adrenal adenoma is large in size (more than 4 cm), indications arise for its surgical removal. Surgery to remove an adrenal adenoma should be performed only in a specialized center for endocrinology and endocrine surgery, which performs at least 100 operations on the adrenal glands annually. Only in a specialized center is it possible to perform surgery for adrenal adenoma with minimal trauma and maximum quality.
Now there are three main methods of performing operations on the adrenal glands: open, laparoscopic, retroperitoneoscopic (lumbar). The most widespread is the open method of performing operations on the adrenal gland, in which access to the adrenal gland is carried out through a skin incision up to 20-30 cm long, with the intersection of the muscles of the anterior abdominal wall, diaphragm, and chest wall. This approach is familiar to surgeons, but at the same time it is the most traumatic.
|
|
The second most commonly used method of surgery to remove adrenal adenoma is laparoscopic, performed endoscopically through punctures in the anterior abdominal wall. The instruments are passed through the abdominal cavity, into which carbon dioxide is injected to create a cavity. The morbidity of this approach is less than that of the open one, but still remains quite high. With laparoscopic access, the peritoneum covering the intestines and abdominal organs is injured, which can cause the development of adhesions in the future. Also, laparoscopic surgery cannot be performed after previous operations on the abdominal organs.
|
|
The most modern and least traumatic method of performing surgery on the adrenal gland for adenoma is retroperitoneoscopic (lumbar extraperitoneal) access, in which endoscopic instruments are inserted through skin punctures in the lumbar region. With a lumbar approach, an endocrinologist surgeon performs the operation extraperitoneally, without penetrating the peritoneal cavity. With the lumbar approach, either three punctures are made on the skin (in traditional retroperitoneoscopic surgery - CORA) or one incision about 2-3 cm long (in single access retroperitoneoscopic surgery - SARA). The morbidity of the lumbar approach is so low that the patient can eat in the evening, and discharge from the hospital after surgery is possible within 2 days. The cosmetic result of this operation is simply amazing - small stitches on the lower back are practically invisible to others.
|
|
There is another way to remove an adrenal adenoma - robotic surgery. Robotic surgery is performed using the same access as laparoscopic surgery; the same number of instruments is inserted into the abdominal cavity. The disadvantages of robotic surgery are similar to those of laparoscopic surgery, but the convenience of the operation for the surgeon is much higher. An additional disadvantage of robotic surgery is the length of time it takes to set up the instruments—it takes 30-40 minutes to “dock” the robot to the assistant.
|
The Northwestern Center for Endocrinology is currently the Russian leader in performing operations to remove adrenal adenoma. Every year, the center performs more than 100 operations on the adrenal glands, the vast majority of which are performed using a low-traumatic lumbar approach. The average length of hospitalization for a patient at the center for adrenal surgery is 4 days.
Most operations at the Northwestern Endocrinology Center are carried out according to the federal quota, i.e. for free. Residents of the CIS countries and other countries can receive treatment for a fee, while the cost of a full cycle of treatment for adrenal adenoma is about 80 thousand rubles.
For treatment at the North-Western Endocrinology Center, you must consult a surgeon-endocrinologist of the center with all available examination results. Consultations for patients with adrenal adenoma are carried out by endocrinologist surgeons of the North-Western Endocrinology Center in the following branches:
— Petrograd branch
(Kronverksky pr., 31, 200 meters from the Gorkovskaya metro station, tel. 498-10-30, from 7.30 to 20.00 seven days a week);
— Primorsky branch
(Savushkina street, 124, building 1, 250 meters to the right from the Begovaya metro station, tel. 565-11-12, from 7.00 to 21.00 on weekdays, from 7.00 to 19.00 on weekends);
— Vyborg branch
(Vyborg, Pobedy Ave., 27A, tel. (81378) 36-306 from 7.30 to 20.00 seven days a week).
Registration for surgery
To sign up for surgery to remove the adrenal gland, you need to consult with a specialist at the North-Western Endocrinology Center with all the examinations you have. The center specialist will study the available medical documentation and, if necessary, conduct additional research. If the diagnosis is confirmed and there are indications for surgery, you will be hospitalized at the center for removal of the adrenal gland using the most modern technologies. Surgeries on the adrenal glands are performed free of charge at the center.
.
Consultations for patients with adrenal adenoma are carried out:
| Sleptsov Ilya Valerievich, Endocrinologist surgeon, Doctor of Medical Sciences, Professor of the Department of Surgery with a course in surgical endocrinology, member of the European Association of Endocrine Surgeons | |
| Rebrova Dina Vladimirovna, Endocrinologist, Candidate of Medical Sciences. Assistant at the Department of Endocrinology named after Academician V.G. Baranov, North-Western State Medical University named after I.I. Mechnikov. Member of the European Society of Endocrinologists, International Endocrinological Society, St. Petersburg Association of Endocrinologists. | |
| Fedorov Elisey Alexandrovich, Surgeon-endocrinologist of the highest qualification category, Candidate of Medical Sciences, specialist at the North-West Center for Endocrinology. One of the most experienced surgeons in Russia performing operations on the adrenal glands. The operations are performed using a minimally traumatic retroperitoneoscopic approach through lumbar punctures, without incisions. | |
| Chinchuk Igor Konstantinovich , Endocrinologist surgeon, oncologist, candidate of medical sciences, member of the European Thyroid Association (ETA). Performs endoscopic operations on the adrenal glands. Retroperitoneoscopic approach. More than 350 surgical interventions per year, half of which are endoscopic. |
Consultations are carried out in outpatient branches of the center:
- Petrograd branch
(St. Petersburg, Kronverksky pr., 31, 200 meters from the Gorkovskaya metro station, telephone for appointment, from 7.30 to 20.00, daily);
— Primorsky branch
(St. Petersburg, Savushkina st., 124, building 1, 250 meters to the right from the Begovaya metro station, telephone for appointments from 7.00 to 21.00 on weekdays and from 7.00 to 19.00 on weekends).
For consultation, please bring all available examination results.
Kinds
Identified adrenal adenoma in men or women should be classified. First of all, the doctor classifies the pathology as a hormone-producing or non-producing type.
Tumors that do not produce hormones are more common. They are also called "silent".
If the growing tissues release any substances, it is necessary to determine their nature. Based on the detection of the secreted hormone, they are distinguished:
- corticosteromas, which produce various glucocorticosteroids;
- corticoesteromas producing estrogens;
- aldosteromes, which produce mineralocorticoids;
- androsteromes, which, in contrast to corticoesteromes, produce male sex hormones;
- mixed, highlighting several different products at once.
Additionally, all adrenal adenomas are divided into pigmented, oncocytic or adrenocortical adenomas.
ATTENTION PATIENTS!
Currently, the North-Western Endocrinology Center provides free surgical treatment for patients with adrenal tumors
. Treatment is carried out within the framework of the compulsory medical insurance program or the SMP program (specialized medical care).
To obtain free hospitalization for out-of-town patients
you must send copies of documents (passport: page with photo and basic data, page with registration; compulsory health insurance policy, SNILS, results of existing examinations - a detailed list is presented below) to the address
Questions about hospitalization can be asked to the responsible administrator, Valentina Petrovna Kleshnina, by calling +7 900 6291427 (weekdays, from 9 a.m. to 5 p.m.).
Package of necessary examinations
should include the following list (if there are no results from the listed studies, they must be performed in any case):
- CT or MRI of the abdominal cavity, if there is only an ultrasound report, then it is necessary to perform a CT scan of the abdominal cavity without contrast, indicating the native density of the adrenal tumor (if necessary, print this item and show the CT scan to the doctor before the study).
The following laboratory parameters must be determined:
- Aldosterone, renin, potassium in the blood, in case of taking diuretics, they must first be discontinued for three weeks (tests are taken in the morning from 8 to 9 am, sit for 15 minutes before taking the tests), after taking these blood tests, resume taking your previous medications;
- Analysis of 24-hour urine or blood for total metanephrines;
- Performing a test with 1 mg of Dexamethasone (in the evening, at 23:00, take 2 tablets of Dexamethasone, in the morning of the next day - from 8 to 9 in the morning, determining the level of cortisol in the blood), the analysis is taken separately from the others, in the last place.
You must also provide information
about the normal level of blood pressure in the patient (working blood pressure), if the pressure increases, indicate the maximum blood pressure numbers, how long ago the increase has occurred and how often rises in blood pressure occur.
To carry out the above examinations, there is no need to go to the hospital; they can be performed at your place of residence or in the nearest laboratory.
For patients from St. Petersburg
It is advisable to apply for a face-to-face consultation before entering the clinic (make an appointment by phone (812) 565-11-12, Primorsky branch of the center, address: Savushkina St., 124, building 1, make an appointment by phone (812) 498-1030, Petrograd branch of the center, address: Kronverksky pr., 31).