Which method of diagnosing an aberrant artery to choose: MRI, CT, angiography
Selection method
- Often, an aberrant artery is diagnosed accidentally
- CT may be considered as the method of choice.
Is MSCT of neck vessels informative for aberrant carotid artery?
- Soft tissue structure in the hypothymlanic region
- Absence of a vertical segment of the ICA
- Expansion of the tympanic tubule
- A defect is visualized in the bone plate between the middle ear cavity and the horizontal segment of the carotid canal.
What conventional and MR angiography will show
- The ectopic vessel narrows at its entry into the base of the skull
- This vessel (aberrant ICA) is located laterally and posteriorly compared to the typical location.
The invention relates to medicine, specifically to urology, and is intended for surgical treatment of hydronephrotic transformation of the renal pelvis.
The blood supply to the kidney is provided by the renal artery, which, as a rule, before entering the kidney, is divided into the posterior and anterior branches of the segmental arteries. Both, in turn, branch in the renal tissue into terminal arteries. But there are cases when segmental arteries begin directly from the aorta, and then from 1 to 2-3 or more vessels go to the kidney. Multiple arteries can supply 20-50% of the renal parenchyma, so their ligation steadily leads to disruption of the nutrition of the corresponding segment of the organ. The presence of both single and multiple renal arteries in humans is the result of intrauterine growth retardation. In urology, the greatest clinical significance is the lower polar aberrant (lat. aberrantis - deviating) vessel, found in 70.8% of cases, starting close to the main renal artery, then going, bending, according to the periphery of the renal pelvis, crossing and compressing the ureteropelvic segment, being the cause of its stenosis - 18-25% of cases (1).
There is a known method of fibromuscular transposition of the lower-polar functioning vessels of the kidney (2), which includes displacement of the lower-polar vessels in the horizontal plane back by placing between them and the ureteropelvic segment a muscle flap on a feeding pedicle, cut from the psoas major muscle, the free end of the muscle flap is placed in its original place in muscle and sutured with catgut. The inferior polar vessel, laid in this way, is located in a muscular coupling - muscle tissue is located between it and the pelvis. However, this method also has a number of significant disadvantages. With mechanical damage to striated muscle tissue, which is the psoas major muscle, a process of degenerative degeneration develops with its spread beyond the direct action of the altering agent, the so-called Zenker necrosis [Zenker, 1864]. As a result, muscle fibers lose structural stability and fuse into homogeneous, dense scar tissue (3). These subsequently developing cicatricial changes in the muscle flap create additional conditions for obstructing the outflow of urine from the pelvis, can narrow the aberrant lower polar artery located between them and disrupt the blood supply to the corresponding segment of the kidney.
The closest to the claimed invention is a method for the treatment of hydronephrosis with additional lower polar vessels, including mobilization, fixation of vessels to the fibrous capsule, while cutting out a flap from the fibrous capsule, one end of which is fixed to the kidney, the second is cut off and brought under the mobilized vessels, which are moved proximally to the pelvis -ureteric anastomosis, the free end of the flap is fixed with a clip to the fixed area of the flap. (4). This method is adopted as a prototype.
The disadvantages of this method are: cutting out a flap of the fibrous capsule of the kidney with an area of 8 cm2 entails disruption of the vascular and neural anastomoses of the capsule with the renal cortex, which are actively involved in the regulation of intrarenal pressure (5). Dense adhesions form between the decapsulated area of the kidney and the tissues surrounding the kidney, which grow into the kidney and compress the renal cortex (6). The fibrous capsule of the kidney has minimal mechanical strength, which is subject to individual and age-related fluctuations (7), which makes it possible to rupture even with slight mechanical stress (8).
The problem to be solved by the invention is the creation of a method for transposition of an inferior polar aberrant vessel from the ureteropelvic segment of the kidney with hydronephrosis using a peritoneal flap on a pedicle.
This objective is achieved through the proposed method of transposition of the lower polar aberrant vessel of the kidney during hydronephrosis, including displacement of the lower polar aberrant vessel upward from the place where it flows into the kidney with a maximum distance from the pelvic-renal segment and fixing it using a peritoneal flap, while mobilizing the anterior surface of the kidney , pelvis, ureteropelvic segment and aberrant inferior polar vessel, a flap is formed on a pedicle from the parietal peritoneum of the lateral canal of the abdominal cavity, the flap is passed under the aberrant inferior polar vessel and, in a tense state, is fixed to the fibrous capsule of the kidney on the anterior surface of the kidney.
In the claimed method, compared to the prototype, the displacement of the lower polar aberrant vessel of the kidney is performed with a flap of parietal peritoneum cut from the lateral canal of the abdominal cavity. This makes it possible to exclude microcirculation disorders in the capsule and cortical layer of the kidney, as well as massive scarring in the perinephric space due to the absence of regional decapsulation of the kidney.
In urological clinical practice, it is known to use the peritoneum to close kidney wounds and fix the kidney in case of nephroptosis. In the proposed method of transposition of an aberrant inferior polar vessel, a peritoneal flap is used for the first time.
A specific example of the implementation of the proposed method is illustrated by the diagram (Fig. 1).
The pelvis 1, the ureteropelvic segment 2 and the aberrant lower polar vessel 3 are mobilized. A flap on the feeding pedicle 4 is cut out from the parietal peritoneum from the lateral canal of the abdominal cavity. The free end of the peritoneal flap 4 is passed under the aberrant inferior polar vessel 3, which is moved upward from the ureteropelvic segment 2. In a taut state, the flap is fixed to the fibrous capsule of the kidney with 5 sutures. The use of the proposed method in urology makes it possible to have a positive effect on the elimination of an external obstacle in the form of an arterial vessel on the ureteropelvic segment without crossing the vessel and the threat of disrupting the blood supply to the area of the renal parenchyma.
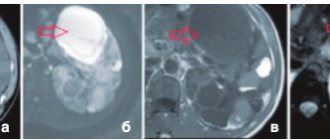
Example (illustrated with photographs: Fig. 2-5). Patient Sh., 54 years old, was admitted to the department with a diagnosis of right-sided hydronephrosis, renal colic. After performing multislice computed tomography, the presence of an aberrant vessel was revealed in the area of the ureteropelvic segment of the right kidney (Fig. 2, indicated by an arrow) with the development of hydronephrosis (Fig. 3, indicated by an arrow). Surgical treatment was performed. After right-sided intermuscular lumbotomy, the anterior surface of the kidney and the anterior surface of the pelvis with the ureteropelvic segment were mobilized, and the presence of an inferior polar aberrant arterial vessel lying on the segment was established. The pelvis is hydronephrotically changed. The aberrant vessel was mobilized to increase mobility from the point of entry into the kidney and from the edge of the pelvis by 2 cm. From the lateral canal of the abdominal cavity, 2 cm above the antimesenteric edge of the colon, a flap of parietal peritoneum 8 cm long and 1.5 cm wide was cut out. The base of the flap is in the area of the diaphragm. The abdominal wound is sutured. Provisional holders were placed on the free end of the peritoneal flap. The flap was passed under the aberrant vessel and, under tension, was fixed with sutures to the fibrous capsule of the kidney on the anterior surface in the area of the upper pole. The aberrant vessel was displaced by a flap from the ureteropelvic segment by 1.5 cm in the upper direction and was located on the anterior surface of the pelvis. The postoperative period proceeded without complications. At further follow-up after 2 years, multislice computed tomography was performed. On the radiograph in the arterial phase, the radius of curvature of the aberrant vessel (Fig. 4, indicated by an arrow) has changed to a larger one when it is in a transposed upper position. On the radiograph in the excretory phase, there is a filling of the ureteropelvic segment with a contrast agent with a decrease in the degree of dilatation of the pelvicalyceal complex (Fig. 5, indicated by an arrow).
Using the proposed method, surgical treatment was performed in 6 patients with good clinical results.
This method is recommended for the surgical treatment of hydronephrosis caused by an aberrant inferior polar vessel.
INFORMATION SOURCES
1. Coachman. Surgery of hydronephrosis and ureterohydronephrosis / J. Kucera. - Prague: State Publishing House of Medical Literature, 1963. - 221 p.
2. Zhila V.V. Transposition of the lower polar vessels of the kidney in hydronephrosis / V.V. Zhila, P.S. Chernenko // Materials of the Fourth Congress of Urologists of the Ukrainian SSR (September 4-6, 1985) / Congress of Urologists of the Ukrainian SSR. - Kyiv, 1985. - P. 222-223.
3. Studitsky A.N. Experimental muscle surgery / A.N. Studitsky. - M.: Medicine, 1959. - 338 p.
4. RF Patent No. 2233126, priority 05.05.2003, Mcl. A61B 17/00. Accepted as a prototype.
5. Kupriyanov V.V. On the importance of the circulatory and lymphatic beds of the fibrous capsule of the kidney / V.V. Kupriyanov // Experimental surgery and anesthesiology. - 1965. - No. 3. — P. 48-51.
6. Volkova P.A. The fate of a fixed kidney / P.A. Volkova // Scientific notes of the Leningrad Medical Institute. - 1959. - T. 3. - P. 359-364.
7. Kuznetsov N.N. Microscopic structure and age-related changes in the human kidney capsule / N.N. Kuznetsov, B.P. Khvatov // Urology. - 1939. - No. 4. — P. 17-22.
8. Chukhrienko D.P.
Nephroptosis / D.P. Chukhrienko, A.V. Lyulko. - Kiev: "Zdorovya", 1969. - P. 113. A method of transposition of the lower polar aberrant vessel of the kidney during hydronephrosis, including displacement of the lower polar aberrant vessel upward from the place where it flows into the kidney with a maximum distance from the ureteropelvic segment and fixing it with peritoneal flap, characterized in that they mobilize the anterior surface of the kidney, pelvis and aberrant inferior polar vessel, form a flap on a pedicle from the parietal peritoneum of the lateral canal of the abdominal cavity, the flap is passed under the aberrant inferior polar vessel, and by tensioning it the vessel is moved upward from the ureteropelvic segment and in a taut state, the flap is fixed to the fibrous capsule of the kidney on the anterior surface of the kidney.
What would the attending physician want to know?
- When planning surgical intervention in this area, the operating surgeon must be aware of the presence of an ectopic vessel in the surgical field.
Physiological (a) and ectopic (b) variants of the structure of the ICA (cited from: Lo et al; with modifications).
a Normally, the petrous part of the ICA consists of vertical and horizontal segments. The inferior tympanic artery, arising from the ascending pharyngeal artery, passes through the tympanic canal and in the region of the promontory (promontorium ) forms an anastomosis with the carotid tympanic artery, which, in turn, passes through the carotid tympanic canal.
b With aplasia of the cervical segment of the ICA, compensation of blood circulation is carried out by increasing the intensity of blood flow through the dilated inferior tympanic and carotid tympanic arteries. The vertical segment of the carotid canal is absent.
What violations can be detected?
There are not so many methods that allow timely detection of various kidney diseases in the early stages. This is due to the fact that at the initial stages of disease development, renal dysfunction does not yet make itself felt with obvious symptoms and the presence of significant foci of damage to the tissues of internal organs. The condition of each kidney directly depends on the state of the lumens of blood vessels and blood flow parameters. One of the most important indicators of the functioning of internal organs is the condition of the walls of blood vessels. The volume and speed of blood pumped by the kidney are also closely related to it. Dopplerography of renal vessels can reveal signs of circulatory disorders at an early stage, when disruptions in the functioning of internal organs have not yet begun and there are no foci of destructive lesions in the renal tissue. Particularly difficult in modern medicine is the identification of thrombosis in organs, spasms and constrictions of the renal vessels. Ultrasound scanner copes with all the listed tasks.
In what cases can this type of diagnosis be prescribed? If there is a suspicion of renal pathologies. Deviations in the functioning of internal organs are usually indicated by:
The listed symptoms are associated with the condition of the arteries of the internal organ, whose malfunction leads to irreversible pathologies. The state of the vascular system of each internal organ also depends on the person’s age. This factor must be taken into account when assessing the condition of the intrarenal arteries.
Return to contents
What diseases have symptoms similar to aberrant internal carotid artery
Dehiscence (non-fusion) of the jugular bulb
— Protrusion of the jugular bulb into the middle ear cavity is determined
— Increase in the size of the jugular fossa
— Defect at the base of the hypotympanic area
Tumor of the tympanic glomus
— Focal effect of soft tissue space-occupying formation in the middle ear cavity
Tumor of the jugular glomus
- Widening and erosion of the jugular fossa and, in rare cases, also of the petrous bone
Cholesterol granuloma
— Effect of soft tissue space-occupying formation with destruction of surrounding bone structures
— TI-weighted imaging typically shows increased signal intensity
Presentation
This condition is usually asymptomatic.[1] The aberrant artery usually arises just distal to the left subclavian artery and crosses the posterior portion of the artery. the mediastinum on its way to the right upper limb.[2] In 80% of individuals it passes beyond the esophagus.[2] This course of this abnormal vessel can lead to the formation of a vascular ring around the trachea and esophagus. Dysphagia due to an abnormality of the right subclavian artery is called dysphagia lusoria, although it is a rare complication.[2][3] In addition to dysphagia, an aberrant right subclavian artery may cause stridor, shortness of breath, chest pain, or fever.[1] The aberrant right subclavian artery can compress the recurrent laryngeal nerve causing paralysis of this nerve, which is called Ortner's syndrome.[4]
An aberrant right subclavian artery often arises from a dilated segment of the proximal descending aorta, called Kommerell's diverticulum (named after the German radiologist Burkhard Friedrich Kommerell (1901–1990), who discovered it in 1936).[5][6] It is also known as the Lusorian artery
.[1][3]
Tips and mistakes
Due to the similarity of imaging results, in some cases a glomus tumor or any other tumor of the middle ear cavity may be misdiagnosed, which is associated with significant risks in terms of treatment tactics.
Aberrant ICA. Unenhanced CT (bone window), axial projection (a), MRA in M1P mode with contrast (b) and DSA (c). The horizontal segment (arrowheads) of the ectopic right ICA protrudes into the middle ear cavity without evidence of cortical covering (a). The vertical segment (bifurcated arrow) is narrower than on the opposite side (b, c) because the ectopic vessel enters the petrous bone through the tympanic canaliculus.
What result can the research give?
The most objective result of the study is obtained if the patient is on the right or left side during diagnosis. Ultrasound scanning of each artery is reflected as a single graph on the monitor. To correctly assess the condition of this element of the internal organ, doctors scan and change the resistance index in the middle, distal and proximal third of the arteries. This indicator is very important, because it makes it possible to get an idea of the processes occurring inside the organ. If the patient's kidneys are functioning within normal limits, the resistance indices in the middle, distal and proximal third of the arteries between the two paired internal organs will be slightly different from each other.
The part of the organ that experts examine plays a role here. When arteries are diagnosed, segmental and interlobar research results are much easier to obtain, which is associated with the very physiology of the structure of the internal organ.
The index is not a constant value. It changes, just like the arteries of the internal organ themselves. An index change occurs if:
Excessive acceleration or deceleration of blood circulation is equally dangerous. The narrowing of the artery leads to increased blood circulation. If blood moves at a speed higher than normal by 20 cm/s or more, then this may be one of the signs of stenosis. Another symptom of this disease is turbulence inside the renal arteries, which can also be detected by ultrasound. In such cases, there is a significant difference in the index between the right and left kidneys. The indicator is significantly lower than what should be typical for a patient according to his age group. If the poststenotic segment of the vessel is disturbed, the condition of the renal arteries will indirectly indicate the presence of this pathology. This pathology is directly related to the main symptom of stenosis (increased blood flow in the renal arteries over 200 cm/s). At the same time, a person begins to have problems with his heart.
References
- ^ a b c d e
Mahmodlou, Rahim;
Sepehrvand, Nariman; Khatami, Sanaz (2014). "Aberrant right subclavian artery: a life-threatening anomaly that should be considered during esophagectomy." Journal of Surgical Technique and Medical History
.
6
(2): 61–63. Doi:10.4103/2006-8808.147262. PMC 4290042. PMID 25598945. - ^ a b c d
Cow, Thomas;
Sinzig, Marietta; Gasser, Johann; Forester, Gerald; Rabich, Egon; Seledin, Stefan; Eicher, Wolfgang; Illiasch, Herbert; Hausegger, Klaus Armin (2007). "Development and anomalies of the aorta." Seminars in Interventional Radiology
.
24
(2): 141–152. doi:10.1055/s-2007-980040. PMC 3036416. PMID 21326792. - ^ a b c d
Chaoui, R;
Rake, A; Heling, K.S. (2008). "Four-vessel aortic arch: aberrant right subclavian artery." Ultrasound in obstetrics and gynecology
.
31
(1): 115–117. Doi:10.1002/uog.5240. PMID 18098341. - Bickle, I. C.; Kelly, B.E.; Brooker, D.S. (2002). "Ortner's syndrome: radiological diagnosis." Ulster Medical Journal
.
71
(1):55–56. PMC 2475354. PMID 12137166. - Saint-Amand, Maxim. "Commerell's Diverticulum (Right Aberrant Subclavian Artery)." Radiopedia
. Retrieved November 17, 2021. - Jha, Praveen. "Commerell's diverticulum." Radiopedia
. Retrieved November 17, 2021. - Kouchoukos NT, Masetti P (April 2007). "Aberrant subclavian artery and Kommerell aneurysm: surgical treatment with the standard approach." Journal of Thoracic and Cardiovascular Surgery
.
133
(4):888–92. Doi:10.1016/j.jtcvs.2006.12.005. PMID 17382621.
Images
- Aberrant subclavian artery on axial computed tomography. (1) trachea, (2) esophagus, (3) aberrant subclavian artery.
- Aberrant right subclavian artery on angiography.
- Ribbon imprint of the esophagus caused by an aberrant subclavian artery. Below (arrows) there is a narrowing of the esophagus by a tumor that is causing problems with swallowing.
- Aberrant subclavian artery on swallowing study: posterior esophageal depression.