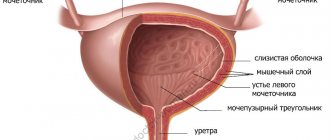
Cystoscopy is an endoscopic type of diagnosis used to examine the inner surface of the bladder. The method is invasive, as it is accompanied by the penetration of a special optical system (cystoscope) into the bladder cavity through the urethra (urethra).
As the cystoscope moves into the bladder, the mucous membranes of the urethra itself are also examined (urethroscopy).
Cystoscopy allows you to examine in detail and assess the condition of the internal covers of the urethra and bladder, identify possible pathologies and determine further treatment tactics.
In comparison with the usual X-ray or ultrasound examination, cystoscopy is the most informative diagnostic method.
Cystoscopy instruments
A cystoscope is a separate type of endoscopic instrumentation, which is a long tube equipped with a lighting system. Through the internal channel of the cystoscope, a special liquid is supplied into the bladder to irrigate the mucous membranes and additional instruments are introduced to perform various medical procedures, for example, forceps for collecting biomaterial for histology, diathermoelectrodes for removing polyps, catheters for installing them in the ureters, etc.
In urological practice I use 2 types of cystoscopes - flexible and standard rigid (rigid). Using a rigid cystoscope, the doctor examines the bladder cavity through an optical system (with the eye), and a flexible cystoscope has a video camera attached to its end, so the image is displayed on a computer monitor. The choice of one or another type of instrument depends on the purpose of the study.
Indications for cystoscopy
Which doctor prescribes cystoscopy and why?
Cystoscopy of the bladder is prescribed by a urologist to diagnose the following conditions:
- chronic cystitis with frequently recurring exacerbations (relapses);
- suspicion of urolithiasis;
- urinary disorders not diagnosed by other means;
- urinary incontinence;
- blood in the urine;
- detection of atypical cells in urine analysis;
- prolonged pain in the pelvic area;
- increased bladder activity;
- suspicion of interstitial (non-infectious) cystitis.
In addition, cystoscopy of the bladder is performed to clarify the results of standard research methods (ultrasound, x-ray, etc.) if an oncological process in the urinary tract is suspected.
The role of cystoscopy in the treatment of urological diseases
A number of therapeutic procedures are performed using cystoscopy:
- stopping bleeding;
- removal of benign and malignant tumors of the bladder;
- performing a punch biopsy;
- crushing and removing stones;
- placement of ureteral catheters;
- dissection of the stricture (narrowing of the internal lumen) of the urethra or the mouth of the ureter;
- removal of obstructions in the bladder.
Features of the procedure in men and women
The length of the ureter in women is only 3–5 cm, which is almost 6 times shorter than in men. Therefore, in women, the procedure is faster, less painful, and even, by agreement with the patient, can be performed without pain relief.
True, in ordinary life, infection penetrates into the urinary system of women just as easily. Therefore, they need cystoscopy examinations more often than men.
If during cystoscopy it becomes necessary to perform any medical procedures on the patient, the anesthesiologist will administer general anesthesia to her.
The male urethra is longer - 15–22 cm. When inserting a cystoscope, men experience pain, and anesthesia is always used. The cystoscope is inserted gently and non-violently, with a possible spasm of the external sphincter waiting for this moment. Sometimes the doctor may ask the patient to take several breathing movements. At the first stage, the penis is lifted upward and an endoscope is inserted to the level of the sphincter ring. Then the penis is lowered and the endoscope overcomes the obstacle in the form of the sphincter.
The procedure is also complicated by the fact that the cystoscope must pass through the location of the prostate. Therefore, the procedure must be carried out extremely delicately and sparingly, otherwise the device can injure the mucous membranes of the urethra, the seminal tubercle, and even temporarily impair potency.
Preparation for cystoscopy
Before the examination, the doctor conducts an explanatory conversation with the patient, during which the essence of the procedure and the features of preparation for it are revealed.
You may need to stop taking certain medications for a while: painkillers and non-steroidal anti-inflammatory drugs, aspirin and anticoagulants, insulin;
Some experts recommend taking the antibacterial drug Monural on the eve of the examination (in the evening around 10 p.m.) in order to prevent inflammatory and infectious complications after cystoscopy;
If the cystoscopy procedure is performed under general anesthesia, then you should not eat anything in the morning. Certain types of local anesthesia also require compliance with this condition;
Tests for cystoscopy:
- general urine analysis;
- biochemical urine analysis;
- blood for clotting.
They must be submitted a few days before the study.
Immediately before the procedure, it is imperative to hygienically wash the external genitalia, and if there is a lot of hair, shave it off to avoid individual hairs getting into the urethra along with the cystoscope.
Cystoscopy and contraindications for its implementation
In addition to the strict criteria for prescribing cystoscopy, there are also a number of contraindications for this procedure. They can be general and local. The following conditions are understood as general:
- Carrying a child, since the uterine walls are located in close proximity to the lining of the bladder.
- Detected renal or liver failure.
- Presence of decompensated heart failure.
Local includes an inflammatory process that occurs acutely in the bladder or urethral canal and increases the risk of worsening the development of pathology, given the possibility of damage to the mucous layers of organs during the examination. The procedure is not recommended for diagnosed prostatitis or orchitis, especially when there is an exacerbation of pathologies. Cystoscopy is refused in case of insufficient blood clotting, in case of bloody discharge from the urethra, if it is impossible to identify their etiology.
Carrying out cystoscopy
The duration of cystoscopy depends on the disease, the type of cystoscope and the qualifications of the doctor and can range from 5-10 to 45-60 minutes. The procedure is performed both in outpatient and inpatient settings.
Both therapeutic manipulations and diagnostic tests during cystoscopy are carried out in a special chair, reminiscent of a gynecological one: the patient lies on his back with his legs raised and bent at the knees. For convenience, the patient's legs are fixed on special supports.
Note: to eliminate pain during the procedure, the patient is given anesthesia. This may be a local anesthetic in the form of a solution or gel, which is injected directly into the urethra, spinal or general anesthesia.
The choice of anesthesia method is determined by the purpose of the procedure (examination or treatment) and the individual characteristics of the human body.
The patient’s external genitalia are first treated with an antiseptic, and the cystoscope tube is lubricated with sterile glycerin, which does not interfere with the transparency of the optical media. Immediately after inserting the device into the bladder, residual urine is removed from it, and then the bladder is thoroughly washed with warm furatsilin.
To assess the capacity of the bladder, it is filled with a clear solution until the patient feels the urge to urinate (the average amount of solution is 200 ml).
Next, the doctor begins to examine the bladder cavity. The examination begins with the anterior wall, then moves to the left lateral, posterior and right lateral surfaces.
Special attention is paid to the study of Lieto's triangle (the area of the bottom of the bladder). It is in this area that various pathologies are most often localized. The orifices of the ureters are also closely examined (location, number, shape, symmetry).
After removing the cystoscope, if local anesthesia was used, the patient can go home immediately. If the examination was carried out under spinal or general anesthesia, then for some time the patient remains in the hospital under the supervision of medical workers.
Features of cystoscopy in men and women
Cystoscopy in women
Women have a short urethra, so local anesthesia is usually used for diagnostic cystoscopy. When performing medical procedures that require more time than a simple examination, regional (spinal) or general anesthesia is used.
Cystoscopy in men
In men, the urethra is much longer, and the sensation when inserting a cystoscope is more painful. Therefore, male patients are given general or spinal anesthesia (regardless of the purpose of the study), and while moving the device along the urethra in order to straighten it, the penis is first raised and then lowered. This technique allows you to avoid mechanical damage to the urethral mucosa.
How is cystoscopy performed?
The procedure can be performed using a cystoscope with a rigid or flexible tube. In the first case, the doctor inserts a solid endoscope up to 30 cm long into the bladder and conducts an examination through a special optical system, looking directly through the device. During rigid cystoscopy, fluid is pumped into the bladder to flush it out of possible pus and blood. The resulting waters are then collected and sent for analysis. This type of cystoscopy is more painful and requires anesthesia.
A cystoscope with a flexible tube makes the examination almost painless. The device follows the physiological shape of organs and easily penetrates hard-to-reach places. True, the image is not as clear as when a rigid endoscope is inserted, but the video camera, which is built into the head of the device, displays the image on the monitor. When examining with a flexible endoscope, the likelihood of causing injury to the patient is minimal. In modern diagnostics, doctors prefer flexible cystoscopy.
The research takes place in the following sequence:
- The patient undresses, puts on a sterile gown and lies on his back, legs slightly apart and bent at the knees.
- The doctor explains the sequence of the procedure and what sensations the patient will experience.
- An assistant treats the patient's genitals with an antiseptic.
- The urologist performs anesthesia; for men, the anesthetic is injected directly into the urethra using a rubber tube and held in it with a clamp for up to 10 minutes. During this time, pain relief begins to take effect. For women, local anesthetic applied to the cystoscope is often sufficient.
- The doctor inserts a cystoscope through the urethra. For easy administration, it is treated with a special gel.
- Urine is forcibly removed from the bladder and washed with furatsilin. Then 200 ml of saline is injected, which straightens the bladder and allows you to examine it in detail from the inside.
- The doctor examines the walls of the organ, the color of its mucous membrane (normally it should be yellowish-pink), checks for ulcers and tumors. Particularly carefully examines the place where the opening of the urethra and ureters are located.
- The device is carefully removed.
- If general anesthesia was not used, the patient can go home. However, immediately after the procedure he should not drive himself. If general anesthesia has been administered, the person remains in the recovery room until consciousness is fully restored.
Chromocystoscopy
To obtain information about kidney functionality, diagnostic cystoscopy in adults is often combined with another procedure, chromocystoscopy.
This study requires preliminary intravenous administration of a contrast agent, after which the doctor assesses from which ureter, after what time and at what speed colored urine will be released.
If the appearance of urine with dye is detected 3-5 minutes after the contrast is introduced into the vein, then this is normal. If excretion is delayed for up to 10 minutes, renal dysfunction is diagnosed.
When is cystoscopy prescribed?
Why might cystoscopy be prescribed and when is it really necessary?
Cystoscopy allows the doctor to see the condition of the bladder with his own eyes. Therefore, it is more informative than diagnostic procedures such as ultrasound of the urinary system or cystography, and is used when the data from these studies is not enough to obtain a complete picture.
When blood is detected in the urine (hematuria), cystoscopy is a basic study: it allows you to detect, and in a significant number of cases, eliminate the source of bleeding.
Cystoscopy may be prescribed based on the results of an ultrasound scan if an ultrasound examination reveals a formation that has arisen on the walls of the bladder. Cystoscopy allows you to visually examine the tumor, remove a polyp (or small tumor), or take material for histological examination, which will show whether the formation is benign or malignant.
For urolithiasis, cystoscopy can be used to unblock the urinary canal (if the stone is obstructing the flow of urine through the urethra).
Cystoscopy in children
The examination of children is carried out according to the same scheme as for adults. But for children, special children's cystoscopes are used, the diameter of which is selected individually in accordance with the age of the child and the anatomical features of his urethra. In modern urology, even cystoscopes have been developed for newborn babies.
For very young children and overly active older children, the procedure is performed under general anesthesia. In other cases, local anesthesia is used.
Parents will be required to provide written consent for their child to undergo research.
Study in women
Typically, the test is easier for women than for men. The reason for this is the peculiarity of the urethra, short and straight.
General anesthesia is not required; a local option is used: an anesthetic is applied to the device.
Difficulties may arise if there are significant tumors in the uterus and pregnancy in its later stages, when the bladder is compressed by the uterus.
It must be understood that the procedure in the second case is performed only for health reasons: there is a high probability of provoking a spontaneous abortion.
Side effects and complications of cystoscopy
Blood in the urine after cystoscopy can be observed for 1-2 days. This is the norm. In addition, burning in the urethra and pain when urinating may also be felt for several days. Over time, these symptoms will disappear on their own.
Relatively often, patients may complain of the development of cystitis after cystoscopy. However, infection during the procedure and subsequent inflammation of the bladder are not always the fault of the doctors. This usually occurs due to insufficient cleanliness of the patient's external genitalia.
A puncture (perforation) of the bladder can occur as a result of the actions of an inexperienced doctor, for example, when collecting histological material, the doctor did not calculate the length of the needle and accidentally pierced the wall of the bladder.
In this case, there is severe pain after cystoscopy that does not go away for a long time, a decrease in the amount of urine excreted, an admixture of blood in it, an increase in body temperature, and chills. In such a situation, the patient requires urgent surgical care.
If the patient does not have any negative symptoms after cystoscopy, then he returns to his usual rhythm of life as soon as possible.
One of the most serious complications of cystoscopy is considered to be damage to the urethra, which results in the formation of a false tract. In this case, the patient is fitted with a cystostomy - a system for draining urine in addition to the urethra. Through a puncture of the abdominal wall in the suprapubic region, a thin tube (catheter) is inserted into the bladder, through which urine flows into an attached container. After qualified treatment, the process of normal urination is restored, and the cystostomy is removed.
When the procedure is contraindicated
In case of acute inflammation of the genitourinary system (cystitis, urethritis, prostatitis, orchitis), internal bleeding and obstruction of the urethra, the patient must undergo a course of treatment and wait for recovery. After which you can do cystoscopy. Otherwise, there is a high probability of causing microtrauma and aggravating the course of the disease.
The doctor will postpone the procedure if the patient:
- increased temperature or fever;
- poor blood clotting;
- signs of a viral or bacterial disease;
- injuries to the genital organs, urethral mucosa, bladder;
- chronic renal failure;
- heart attack;
- pathologies of the prostate gland and testicles.
Study in men
The anatomical features of a man (the length of the urethra can reach over twenty centimeters) cause certain difficulties in conducting the study.
The physician is required to be highly qualified and accurate. Mainly, this plays an important role at the stage when the device is inserted.
An anesthesiologist must be present during the examination, as there may be a risk of severe pain when it is necessary to administer an anesthetic drug.
Complications
After the procedure, blood discharge may appear in the patient’s urine for several days.
Not excluded:
- Burning;
- Discomfort in the urethra;
- Pain when urinating.
To quickly resolve these symptoms, you need to consume plenty of fluids during the first few days.
Among the complications that may appear after the study are the following:
- Acute cystitis;
- Damage to the organ wall;
- Bleeding;
- Injury to the urethra, some others.
Possible complications