Varicocele (from Latin varix, varicis - swelling of veins, ancient Greek kēlē - tumor). Pathology associated with varicose veins of the spermatic cord, pampiniform (or pampiniform) plexus. The danger is that the first stages of the disease are asymptomatic.
Varicoceles are classified according to the localization of the process: left-sided (occurs in 70-80% of cases), right-sided (in only 10% of cases) and bilateral. It is most often diagnosed in adolescence, but is also not uncommon during puberty. Among diseases of the genitourinary system, varicocele is detected in 35% of cases.
Reasons for the development of varicocele
Varicocele rarely acts as an independent disease caused by genetic factors. In 85% of cases, the pathology appears due to impaired blood flow, worn out or weak vein walls and insufficiency of the venous valves. However, these violations are consequences, not root causes.
Problems leading to enlargement of the veins of the scrotum area:
- Features of the anatomical structure . During the formation of the reproductive system, the organs could develop unevenly, which is why the renal or vena cava is pinched.
- Narrowing of the lumens of the veins . Due to prolonged use of vasoconstrictor drugs or due to developing atherosclerosis.
- Neoplasms, inflammatory processes in the pelvic area . A growing tumor or edematous tissue puts pressure on the veins.
- Excessive physical activity . Especially associated with carrying heavy objects in front of you.
- Chronic constipation . The mechanism of expansion is approximately the same as when lifting weights - the man strains, as a result of which blood rushes to the affected area.
Risk factors leading to the development of the disease are excess weight, impaired metabolism and hormonal imbalance in the body.
MAKE AN APPOINTMENT WITH A UROLOGIST
Klokov Andrey Nikolaevich
Urologist-andrologist, doctor of the highest category
Make an appointment
Varicocele - causes, symptoms and treatment
27.04.2020
Varicocele is called dilation of the vessels of the spermatic cord. More often, pathology develops on the left side, at the junction of the spermatic vein and the renal vein.
Varicocele sperm production and its quality, causing infertility . Varicocele is called dilation of the vessels of the spermatic cord. More often, pathology develops on the left side, at the junction of the spermatic vein and the renal vein. Varicocele is called dilation of the vessels of the spermatic cord. More often, the pathology develops on the left side, at the junction of the spermatic vein with the renal vein. It disrupts the normal development of the testicles , the ability of the testicles to rise, and respond to changes in temperature.
Symptoms of varicocele
Venous lesions may be asymptomatic. Often the problem can only be discovered during the examination due to fertility .
Varicocele appears:
- feeling of heaviness, dull pain in the testicle , worsening in the evening, in hot weather or after intense physical activity;
- scrotal sagging;
- general weakness;
- impotence.
As the pathology develops, dilated veins A testicle whose venous walls are damaged is smaller than a healthy one due to developing atrophy.
Due to blood and ischemia, the blood-testicular barrier is destroyed, cytotoxins penetrate into the seminiferous tubules, testosterone levels decrease, and spermatogenesis is disrupted.
Causes of varicocele
The pathology is most often congenital. It can also be provoked by anatomical features - valve defects in the veins of the scrotum, located slightly above the testicles . Normally, they regulate blood circulation (to the testicles and in the opposite direction), but if the blood flow is disrupted, the vessels dilate due to blood .
Varicoceles often diagnosed during puberty, when blood to the testicles increases due to rapid growth.
Risk factors:
- strength loads (weight lifting, intensive training);
- the presence of thrombophlebitis , renal hypertension, inguinal-scrotal hernia ;
- chronic constipation;
- overheating of the genitals .
Diagnostics
Dilated veins can usually be detected during examination (including during self-diagnosis) by palpation of the pampiniform plexus, while the patient must stand.
The urologist uses the so-called Valsalva maneuver: after exhaling completely, you need to take in air again and exhale, holding your breath. As a result, the pressure on the veins increases, which makes it possible to detect pathology.
Diagnostics may include Doppler ultrasound (standing and lying down), ultrasound , thermography.
Urine samples are also taken to identify protein and blood . The concentration of sex hormones and a spermogram is compiled.
Treatment of varicocele
If the pathology does not cause pain, does not negatively affect fertility and erection, and does not progress, we are limited to observation.
If there is pain, a hematoma of the scrotum or the testicle atrophies, infertility - treatment is mandatory.
Non-invasive methods include:
- minimizing physical activity (first of all, cycling and horse riding are excluded);
- taking anti-inflammatory and vasoconstrictor drugs;
- wearing thick underwear, jockstraps;
- refusal to stay in a static position (standing) for a long time;
- cold baths, compresses on the scrotum area, avoiding overheating.
In surgical treatment, the affected vein is ligated, redirecting blood flow to the superficial veins . operation requires general anesthesia. The surgeon the spermatic cord through a 5-centimeter incision slightly above the iliac region, parallel to the inguinal canal. Risks include: recurrence of varicocele , arterial , tissue infection, testicular hydrocele .
operation is less traumatic. The incision does not exceed 2 cm, during which the spermatic cord is removed and the dilated veins are cut off. Recovery is faster, the risk of relapse does not exceed 5%.
An even more gentle method is endoscopic surgery , when the thrombosed vessel is accessed through holes of minimal diameter.
Varicoceles also eliminated using microsurgical revascularization. In this case, vessel (epigastric vein takes vein ; blood flow is restored almost immediately.
Prognosis and prevention
After therapy , as a rule, after 3 months, sperm improves. In some cases, sperm parameters improve only after 6-12 months.
Preventive measures include:
- moderate physical activity (without lifting weights, if there is a genetic predisposition to varicocele );
- eliminating constipation;
- maintaining normal blood , especially with a tendency to hypotension.
At the end of puberty, it is recommended to undergo an examination by a urologist .
Refusal to treat varicocele (if indicated) is fraught with progressive testicular atrophy and infertility .
Published in Urological diseases Premium Clinic
Symptoms of varicocele
More often, a man learns about the emerging pathology during a study by reproductive specialists, when a married couple cannot conceive a child. Doctors carry out diagnostics and find a scanty spermogram, and on an ultrasound of the scrotum - dilation of blood vessels and veins.
Sometimes the patient independently consults a doctor with complaints about changes in the structure and appearance of the scrotum. Men compare the organ to a bag of worms. The veins are dilated, their branching is visible through the skin.
The most obvious sign of pathology is pain of varying intensity in the scrotum and groin area. They can be pulling, appear only during loads or constantly.
Category of suitability for recurrent varicocele
Right at the medical examination, a conscript diagnosed with grade III varicocele receives a referral for surgery. Whether to do it or not, the guy must decide on his own, but until the operation is done, he belongs to the category of limited fitness.
Read more about how eligibility categories are deciphered here.
If a young man decides to have an operation during which the veins of the scrotum are removed, it is considered that the cause of the disease has been eliminated. Then he can go to the next medical examination in the next draft and, if improvements are visible, he can be assigned to any army - there are no restrictions on service.
It is rare, but it also happens that a young man experiences a recurrence of varicocele while serving in the army. Situations are also possible when a young man with second-degree varicocele experiences an exacerbation right in the army.
In both cases, the service is “cancelled”: the documents say “unfit”, and the man can no longer repay his debt to his homeland. It is assigned category B, which means it is suitable only in wartime.
Stages of development
The most important classification of the disease according to stages of development:
- First . There are no symptoms of pathology, the expansion is not visually visible or palpable. The problem can only be determined by ultrasound.
- Second . The disease cannot be visualized. When palpated in a vertical position, the expansion is palpable, especially after exercise. When lying down, the varicocele does not appear.
- Third . The patient independently feels the dilated venous nodes in any position: lying or standing.
- Fourth . The expansion is strong, noticeable to the naked eye. The nodes do not “hide” due to changes in body position, sometimes they even hang down, increasing the size of the scrotum by 1.5-2 times.
Some doctors combine the third and fourth stages.
Varicocele: will the army take 2021 at the second stage of the disease
The second degree is not yet a reason for the patient to be unfit for service, especially if the disease is asymptomatic, and this is what happens in most cases. After the examination, the conscript is given a referral for surgery. Naturally, this will require additional tests and so on, but in the end it all comes down to the need for surgery. The disease is not yet at such a serious stage as to create any serious problems and complications, after which negative effects on other health factors may occur. Here it is more relevant to talk not about deferment, but about unsuitability for service.
After varicocele surgery, they will not immediately enlist in the army, since a certain amount of recovery time will be required even with an easy operation. The deferment after this is six months. It begins to operate after the operation, but at the end of its period the person again becomes fit for service.
Effect on male infertility
Reproductive dysfunction occurs due to the development of varicocele. Due to impaired blood supply, the following problems occur:
- The temperature of the testicles increases. Hyperthermia has a detrimental effect on the activity and viability of sperm;
- Hypoplasia, atrophy, testicular hypoxia. Tissues die, the function of producing sex hormones and cells decreases;
- Oxidation. The body's waste products (free radicals) accumulate in the testicles, poisoning them;
- Biological substances produced by the adrenal glands are released into the testicles.
Scientists have proven that due to these consequences, varicocele can provoke the development of male infertility. However, this does not mean that reproductive function is necessarily impaired in pathology. In some cases, high-quality spermogenesis remains, but in order to prevent the condition from worsening, it is important to consult a doctor.
Andrology - men's problems
This pathology occurs in 10-15% of men. Moreover, if we diagnose all infertile men, then among them, 40.3% are diagnosed with varicocele. Depending on which side is affected, nagging pain in the groin will have a corresponding irradiation. Discomfort in one or both testicles may increase with physical activity or during intimacy. Is military service possible with varicocele? In one case they can be recruited for military service, but in others not. In order to give an objective answer, it is necessary to conduct a general, thorough examination. As practice shows, targeted diagnostics makes it possible to identify diseases that are exempt from military service completely or for a certain period.
Military service with varicocele largely depends on the severity of the development of the pathology. As a rule, doctors differentiate three degrees of severity of varicocele. With the first degree of venous dilatation of the veins in the groin area, an increase in the veins of the scrotum is determined, which can be diagnosed by palpation, provided that the abdominal muscles are tense. Varicocele of the second severity is characterized by a noticeable enlargement of veins in the declared area, which is confirmed after palpation. Visualization of the problem with the appearance of nodular foci is characteristic of dilatation of the veins of the spermatic cord, third degree of severity. Young men complain of nagging pain in the groin area, discomfort and the inability to conceive a child. If necessary, the doctor may prescribe surgical treatment, after which complete recovery occurs and reproductive function is restored. But the question of whether people with varicocele are accepted into the army remains open. Moreover, it is quite difficult to give a definite answer; each case is considered individually.
With the first degree of illness, a conscript can expect to soon enter the army system and serve in the army. And all because, having appeared in adolescence, varicocele can go away on its own or under the influence of drug treatment. In the event that even if the disease remains, military service should not lead to a worsening of the condition, therefore it is not considered a contraindication.
If there is a more serious pathology, doctors may recommend surgery. The operation under general anesthesia is designed to relieve the man from the negative manifestations of the pathology. After surgical treatment, the conscript is entitled to a deferment of 6 to 12 months. After the deferment period has been exhausted, you need to prepare for military service, because with the second degree of varicocele they are taken into the army. The following recommendations can be given in this regard. Even before passing the medical examination at the military registration and enlistment office, it is advisable to visit a urologist or andrologist at the clinic. Such an examination will be more objective, because the doctor will not be interested in whether or not to draft a young man into the army. In addition, the patient’s inactivity in relation to his own health can end disastrously. There is a high probability that the pathology from the second degree will move to the third, manifesting itself with negative consequences. Then the medical commission has the right to make a decision on the conscript’s unfitness for service. If the commission makes a decision in violation of your rights, urgently contact legal assistance for conscripts - specialists will appeal the illegal decision, and it will be canceled by law.
Diagnosis of varicocele
The urologist first collects anamnesis and examines the patient. To confirm or refute varicocele, the doctor begins functional tests (tests):
- Valsalva maneuver . A patient with pathology imitates coughing, during which the abs tense, the doctor at this time probes an impulse in the area of the inguinal ring.
- Ivanissevich's test . The man lies down on the couch. The nurse or doctor presses the spermatic cord against the pubic bone at the level of the outer ring of the inguinal canal. When squeezed, the veins in the scrotum of a healthy person are not filled, but if the cord is released, they immediately fill with blood. In a patient with pathology, the veins remain visually full.
The urologist necessarily prescribes laboratory tests: blood, urine, smear from the urethra for microflora, prostate secretions. For patients over 21 years of age, laboratory technicians examine sperm.
The most reliable clinical picture is provided by ultrasound of the scrotum with a Doppler sensor. The specialist determines during the study:
- vein size;
- volume of testicles, gonads;
- quality, speed of blood flow;
- resistance (resistance to pathological factors) of blood vessels.
The doctor compares the detected size of the testicles and other structural elements with the norms according to the patient’s age.
Military service with varicocele
In general, military service is highly not recommended for those young men who have varicocele. After physical exertion, which simply cannot be avoided in the army, the disease can manifest itself in the most insidious way.
Walking in formation, running, and passing other standards speed up blood flow, which, in principle, has a beneficial effect on the condition of the body. Young people who do not have venous pathologies tolerate such physical activity quite calmly. However, for those who have been diagnosed with varicocele, a change in the usual speed of blood flow can be a very disastrous event: the disease becomes acute, which is accompanied by severe pain and swelling in the groin area.
One way or another, not all conscripts with such a pathology receive a deferment from military service. The enrollment of a young man in the army depends on the degree of development of the disease. Let's look at these forms in more detail.
Do they take you into the army with grade 1 varicocele?
The peculiarity of the first degree of varicocele is that the disease at this stage practically does not manifest itself in any way. There is no pain, and often the young man does not even suspect that he has such a pathology. As a rule, the disease is detected by ultrasound. There are often cases when the disease first makes itself felt in adolescence, but by the time conscription age approaches, it goes away on its own.
This situation involves assigning a category “B” to a young person, indicating limited suitability. A diagnosis of varicocele makes it impossible to enroll in military service in elite troops, but a conscript is still allowed to enlist in certain branches and branches of the Armed Forces.
Do they take into the army with grade 2 varicocele if they refuse surgery?
In the second degree, an enlarged vein in a relaxed state is quite difficult to detect: it is diagnosed exclusively in a standing position. Since the vascular walls are stretched to a significant extent, the young man begins to feel the first symptoms of the disease.
According to the “Schedule of Diseases”, this stage of the disease corresponds to categories “B” or “C”, where the latter means enrollment in the reserves and the further possibility of mobilization in wartime. In particularly critical situations, the conscript is entitled to a temporary deferment, so his VB is assigned category “G”. Representatives of the VVK thus give the young man the opportunity to improve his health and, in case of emergency, undergo surgical treatment.
If the young man decides not to agree to the operation, he must sign an official refusal. Subsequently, he is assigned category “B,” which automatically transfers him to the reserve. However, it should be remembered that ignoring a disease such as varicocele is fraught with many negative consequences, therefore, before signing the appropriate refusal papers, you need to carefully weigh the pros and cons.
Do they take into the army with grade 3 varicocele after surgery?
The third degree of pathology is characterized by its own characteristics: the dilated vein is visualized even with the naked eye in any position accepted by the young man. The disease at this stage of development is accompanied by quite severe pain, swelling and nodes localized in the scrotum, and a strong enlargement of the organ.
Conscripts diagnosed with varicocele of the third degree are assigned category “D”, which means they are unfit to perform military duty either in peacetime or in wartime. In addition, pathology in this form is an absolute contraindication to training in military departments. It should be noted that representatives of the IHC, in addition to the very fact of the presence of the disease, also take into account other circumstances: the conscript’s condition is registered with a urologist, cases of visiting a doctor recorded in the patient’s medical record, relapses of the pathology, etc.
After undergoing surgery, the young man is required to undergo re-examination. Most often, after the expiration of the rehabilitation period, the young man receives category “B” and is enlisted in those branches and branches of the military, service in which does not involve strong physical activity (this could be guard and radio engineering units, chemical and missile units, etc.).
Treatment of varicocele
Urologists use strictly radical methods of treatment - surgical operations. There is no conservative treatment for varicocele. More than 120 methods of getting rid of pathology have been developed.
However, in modern urology the following methods are mainly used:
- Operation Marmara. Doctors ligate the vein and use infrainguinal access for the operation. They cut through the area of the external inguinal ring without affecting the muscle fibers and fascia, compress the vein (sew it together) and connect the edges of the wound.
- Microsurgical alloying. If the spermatic cord is clearly visible, you can introduce a special binder inside that glues its walls together.
- Endovascular sclerotherapy and embolization of the left testicular vein. Using a needle, specialists insert an electric diode into the vein, which glues the walls of the vein; in addition, the doctor injects a solution of glucose and thrombovar.
- Laparoscopy. With the help of modern equipment, it is possible to carry out ligation or suturing of blood vessels through several small punctures using micro-instruments.
- Classic operation. It is used in difficult situations at the 4th stage of pathology. The doctor uses a scalpel to excise the skin in the area of the testicular vein, then clamp the vein in two places, cut it and sew the ends together.
Regardless of the type of operation, the procedure is aimed at changing the blood flow in the cluster: by blocking the access of blood in one area, the specialist makes it possible to relieve the affected veins.
Epidemiological assessment of risk factors for varicocele in adolescents
T.M. Chirkina, T.A. Dushenkova, S.V. Rishchuk, B.I. Aslanov, V.E. Mirsky, M.I. Gurova, O.K. Bulakhova
One of the widely discussed issues in modern society is the protection of reproductive health of the population. An increase in infertility in the population is associated with the development of a number of reproductively significant diseases, one of which is varicocele. In the practice of reproductive medicine, varicocele is detected in 15% of healthy men, in 35% of men with primary infertility and in 80% of men with secondary infertility [1].
The results of a number of studies have demonstrated the need for early detection of uroandrological pathology among adolescents in order to carry out timely and effective correction to prevent the development of fertility disorders in the future [2,3].
According to JT Casey et al. in persons over 15 years of age, the incidence of varicocele was 15%. It has been noted that the negative effects of varicocele are long-term and progressive: the number of sperm, their motility and morphology decreases, which can cause the development of infertility in subsequent years [4].
According to F. Vasquez et al. spermogram indicators in patients with varicocele (patients' age ranged from 14 to 17 years) corresponded to the following options: oligoasthenozoospermia was observed in 38.3% of patients; normospermia – in 28.3%; asthenospermia – in 16.7%; oligozoospermia – in 11.7%; Azoospermia – in 5%. Pathological changes in the ejaculate were determined in patients with second and third degree varicocele with approximately the same frequency [5].
A good anatomical result of surgical treatment of varicocele does not guarantee an improvement in the functional state of the gonads in the postoperative period. Thus, disruption of intratesticular blood flow persisted in 51.4% of patients with varicocele [5,6]. Studies in recent years have shown that after surgical treatment of varicocele, normospermia was diagnosed in 53.2% of cases [7].
Attempts to conduct an epidemiological assessment of risk factors for the development of varicocele have been made repeatedly by medical services in various regions. Since information about the prevalence of varicocele was most often based on clinical and laboratory examination data of men who consulted a specialist for treatment of already established infertility, the true prevalence remained underestimated [8].
The state of health in childhood and adolescence plays an extremely important role in the formation of a man’s reproductive potential. Identification of risk factors for the formation of andrological pathology in the early stages provides an opportunity, through the timely efforts of highly qualified specialists, to prevent the development of infertility in men of reproductive age.
The purpose of the study is to identify the prevalence of varicocele among adolescents in St. Petersburg and to conduct an epidemiological assessment of risk factors for its development.
MATERIALS AND METHODS
The study consisted of two sections and was a complex of several epidemiological research methods: descriptive and analytical. In the first section of the work, the epidemiological features of varicocele were identified. The material for this section was an epidemiological study assessing the intensity and structure of the epidemic process. An analysis of data from clinical examinations by a pediatric urologist-andrologist of 310 boys aged 10 to 17 years was carried out on the basis of a number of children's clinics in St. Petersburg for the period 2012-2017. The diagnosis of “varicocele” was revealed on the basis of palpation and visual examination, ultrasound examination of the scrotal organs and Doppler sonography.
The next section of the work included an epidemiological assessment of risk factors for varicocele. Using the analytical method of epidemiological assessment of the significance of the studied factors, a case-control study was conducted, followed by a statistical analysis of a questionnaire survey of the results of 222 parents of examined adolescents. All children were examined by andrologists at children's clinics in St. Petersburg. The group of “cases” consisted of 136 adolescents with varicocele. The control group included 154 adolescents of the corresponding age category who did not have varicocele. The questionnaire included questions on 52 risk factors related to the mother’s obstetric and gynecological history, previous infectious diseases of the parents, exposure to harmful environmental factors, and the presence of somatic pathology in close relatives.
RESULTS AND DISCUSSION
Of the 310 examined adolescents, varicocele was detected in 82 (26.4 per 100 examined). Varicoceles of grades 1 and 2 were the most common in the population of boys examined (Table 1).
Table 1. Frequency of varicocele in teenage boys in St. Petersburg for the period 2012-2017. (N=310)
| Clinical diagnosis | Frequency (per 100 people) | 95% CI |
| Varicocele 1st degree | 2,6 | 8,5-15,7 |
| Varicocele 2 degrees | 9,0 | 6,0-12,4 |
| Varicocele 3 degrees | 5,4 | 3,2-8,2 |
The structure of varicocele according to the degree of the disease was as follows: degree 1 varicocele was diagnosed in 45.2% of patients with an established diagnosis, degree 2 was observed in 34.1%, degree 3 was observed in 20.7% of adolescents (Fig. 1).
Fig.1. Structure of varicocele depending on the severity of the pathological process (N=82)
The high proportion of grades 1 and 2 varicocele (45.2% and 34.1%) indicates the need to diagnose the disease in the early stages in order to prevent dangerous progression of the pathological process at an older age.
We analyzed the incidence of varicocele among patients of different age categories of adolescents: 10-11, 12-14 and 15-17 years. Most often, the pathological process was diagnosed in patients over 15 years of age (Fig. 2).
Fig.2. Frequency of occurrence of varicocele in children and adolescents in various age groups in 2012-2017. (N=310)
This may be due to the fact that during puberty a number of hormonal changes occur, resulting in excessive load on the veins of the pampiniform plexus.
Most often, modern studies are focused on studying risk factors for the development of varicocele in adult men seeking treatment for infertility [8]. Much less is known about the influence of risk factors for varicocele in adolescents associated with lifestyle and chronic diseases of parents.
The results of statistical data processing are presented in Table 2.
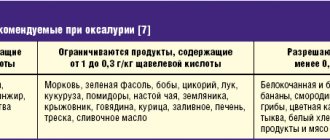
Table 2. Risk factors for the development of varicocele according to the results of an analysis of a survey of parents of adolescents (N=222)
| Risk factor | Odds ratio (OR) | 95% CI |
| Using diapers for more than 1 year | 11,9 | 1,4-4,7 |
| Ureaplasmosis in the child's mother | 5,6 | 1,4-21,5 |
| Varicocele 3 degrees | 4,2 | 1,1-17,1 |
| Varicose veins on the legs of the child's mother | 3,4 | 1,3-8,9 |
| Alcohol use by father before birth | 2,1 | 1,2-3,6 |
| Cardiovascular diseases in the child's father | 2,9 | 0,9-9,2 |
The main mechanism of influence of varicocele on endocrine function and spermatogenesis is most often associated with an increase in temperature in the scrotum.
Modern disposable diapers are now ubiquitous. The safety assessment of disposable diapers is determined by two important parameters: the frequency of their use and the contact of polymer materials with the skin. In the US, the average use is 4.7 diapers per day [9]. Studies on the effects of diaper use on infants show negative effects due to the fact that the testes and epididymis are exposed to temperatures higher than body temperature. It is known that for normal spermatogenesis, a temperature in the scrotum of about 34°C is more favorable. The use of diapers in infancy leads to a long-term increase in temperature in the appendages by 1-2°C. Unlike dry cloth diapers, modern diapers have a number of characteristics that create an increase in the temperature of the scrotum, which is unsafe. Thus, diapers used during the early stages of development may have adverse effects on reproductive potential later in life. However, in the context of evidence-based medicine, this factor requires more detailed study [10].
The results of our study showed that the use of diapers for more than 1 year has an adverse effect (OR – 2.6), disrupting the venous outflow in the pampiniform plexus of the spermatic cord in adolescence.
Today, one of the significant problems in medicine is sexually transmitted infections. Due to the peculiarities of biology, Ureaplasma urealyticum occupies a special place among the causative agents of urogenital infections. A search of scientific publications that analyzed the influence of the presence of ureplasmosis in one or both parents on the development of varicocele in adolescents showed that the pathogenesis of the disease is concentrated exclusively at the level of the individual. It has been shown that U. urealyticum has the ability to disrupt the uteroplacental barrier and causes an inflammatory reaction, being one of the causes of antenatal and perinatal infection of the fetus [11].
A study conducted among infertile men in different countries showed that the pathogen was found in 12.1-20.1% of men with varicocele, in 9.2% of patients without varicocele, in the control group of healthy patients - in 3%. In another study, asymptomatic genital U. urealyticum infection was detected in 55.7% of men with varicocele and 34.9% of infertile patients without varicocele [12].
Thus, the higher prevalence of this microorganism in patients with varicocele may be an additional negative factor that has an adverse effect on reproductive potential.
Our data also confirm the influence of ureaplasmosis in both the father and mother (OR – 5.6 and 4.2, respectively) on the incidence of varicocele development in the child.
Recent publications indicate that among patients with varicose veins of the lower extremities, varicocele is more common [13]. The reason for the connection remains unknown. The results of a study of risk factors conducted among parents of adolescents demonstrated an association between varicose veins of the lower extremities in the mother and varicocele in the child (OR – 3.4). There is an assumption that this connection is due to a genetic factor.
According to our study, we obtained significant risk factors, such as alcohol consumption by the father before the birth of the child and the presence of cardiovascular diseases, but their significance requires more detailed study in further studies.
Since the primary diagnosis of varicocele is associated with a number of difficulties caused by the lack of andrologist specialists in outpatient practice, we analyzed the staffing of children's outpatient departments (DPO) with such specialists in different areas of the city. Currently, children's clinics are staffed by 46% andrologists and 78% by pediatric surgeons. In the Vasileostrovsky, Kolpinsky and Petrogradsky districts there are completely no pediatric andrologist specialists. In 2015, in St. Petersburg, the staffing of preschool education with pediatric uroandrology specialists was also at a low level – 32% [14].
According to the order of the Ministry of Health of the Russian Federation No. 1346n “Procedure for medical examinations for minors” dated December 21, 2012 [15], the purpose of primary diagnosis is to select patients for further laboratory and instrumental examination, final diagnosis and adequate timely treatment [16,17]. It should be noted that the current state of affairs in the practical healthcare system does not provide a solution to the task.
CONCLUSIONS
The results of the study showed that the prevalence of varicocele among adolescents in St. Petersburg is high and amounts to 26.4 per 100 examined.
Varicoceles of 1 and 2 degrees were most common in the population of teenage boys (11.9 and 9.0 per 100 examined teenage boys)
Among patients of different age categories, depending on the severity of the disease, the pathological process was most often diagnosed in patients over 15 years of age (12.5 per 100 examined in the group of adolescents 15-17 years old and 9.1 per 100 adolescents 12-14 years old).
An assessment of the risk factors for varicocele in adolescence made it possible to identify the following predictors of the development of the disease: using diapers for more than 1 year, ureaplasmosis in one of the parents, varicose veins in the legs of the child’s mother. To substantiate the significance of these factors, further studies of the pathophysiological mechanism of their effects during the period of intrauterine development of the fetus are required.
Despite the implementation of health care programs in recent years, the problem of lack of andrological care for the child population remains relevant. The key to improving the quality of work of the pediatric andrological service is the creation of uniform examination principles established by regulations in the healthcare sector of the Russian Federation. It is important that an ideology is established in the minds of medical workers, in which a special place should be given to the prevention of diseases that increase the risk of developing infertility in the future.
The conducted epidemiological analysis shows that, using this approach, it is possible to determine whether a child belongs to a risk group for the formation of varicocele, which in turn indicates the need to focus attention on these groups with the involvement of andrologist specialists. In order to timely diagnose varicocele, screening examinations of children and adolescents should be carried out in educational institutions.
LITERATURE
1. Alsaikhan B, Alrabeeah K, Delouya G, Zini A. Epidemiology of varicocele. Asian J Androl 2016;18(2):179-181. doi: 10.4103/1008682X.172640.
2. Muravyova V.N., Zenin V.V., Panchenko I.A. The role of primary pediatric care in the organization of children's uroandrology service (on the example of the city of Stavropol). Urology 2014;(4):39-41.
3. Apolikhin O.I., Moskalev N.G., Komarova V.A. Current demographic situation and problems of improving the reproductive health of the Russian population. Experimental and Clinical Urology 2015;(4);4-14.
4. Casey JT, Misseri R. Adolescent Varicoceles and Infertility. Endocrinol Metab Clin North Am 2015;44(4):835-842.
5. Vásquez F, Soler C, Camps P, Valverde A, García-Molina A. Spermiogram and sperm head morphometry assessed by multivariate cluster analysis results during adolescence (12-18 years) and the effect of varicocele. Asian J Androl 2016;18(6):824-830. doi: 10.4103/1008682X.186873.
6. Sizonov V.V., Makarov A.G., Kramarov A.I., Kogan M.I. Varicocelectomy in adolescents – who should be operated on and when. Urology 2015;(2):107-111.
7. Pugachev A.G., Evdokimov V.V., Zakharikov S.V., Erasova V.I. Varicocele in adolescents: a problem of male fertility. Experimental and Clinical Urology 2010;(3):43-46.
8. Jacobson DL, Johnson EK. Varicoceles in the pediatric and adolescent population: threat to future fertility? Fertil Steril 2017;108(3):370-377. doi:10.1016/j.fertnstert.2017.07.014
9. Fahimzad A, Taherian M, Dalirani R, Shamshiri A. Diaper Type as a Risk Factor in Urinary Tract Infection of Children. Iranian Journal of Pediatr 2010;20(1):97–100
10. Ivell R. Lifestyle impact and the biology of the human scrotum. Reprod Biol Endocrinol 2007;(5):15. doi: https://doi.org/10.1186 /1477-7827-5-15.
11. Namba F, Hasegawa T, Nakayama M, Hamanaka T, Yamashita T, Nakahira K, et al. Placental features of chorioamnionitis colonized with ureaplasma species in preterm delivery. Pediatric Res. 22010;67(2):166-172. doi:10.1203/PDR.0b013e3181c6e58e.
12. Peerayeh SN, Yazdi RS, Zeighami H. Association of Ureaplasma urealyticum infection with varicocele-related infertility. J Infect Dev Ctries 2008;2(2):116-119. doi: https://doi.org/10.3855/jidc.281.
13. Al-Kandari AM, Shabaan H, Ibrahim HM, Elshebiny YH, Shokeir AA. Comparison of out-comes of different varicocelectomy techniques: open inguinal, laparoscopic and subinguinal microscopic varicocelectomy: a randomized clinical trial. Urology 2007;(69):417-420. doi: 10.1016/j.urology.2007.01.057.
14. Dushenkova T.A., Chirkina T.M., Rishchuk S.V., Mirsky V.E. Reproductive health disorders in children and adolescents of St. Petersburg. Med Almanac 2015;5(40):168-171.
15. Order of the Ministry of Health of the Russian Federation No. 1346n dated December 21, 2012 “Procedure for medical examinations for minors.”
16. Order of the Ministry of Health of the Russian Federation No. 404 dated August 12, 2003 “On the doctor - pediatric urologist andrologist.”
17. Order of the Ministry of Health of the Russian Federation No. 566 dated November 25, 2003 “On the protection of reproductive health of boys and teenage boys.”
The article was published in the journal Experimental and Clinical Urology. Issue No. 1/2018 pp. 112-117
Topics and tags
Pediatric urology
Magazine
Journal "Experimental and Clinical Urology" Issue No. 1, 2018
Comments
To post comments you must log in or register
Prevention
The main rule for preventing the disease is preventive examinations, always with the involvement of ultrasound specialists. Urologists recommend:
- Avoid diseases of the genitourinary system and prevent their development into a chronic form.
- Do not self-medicate.
- Do not disrupt the thermoregulation of the genitourinary system.
- Avoid excessive physical activity.
- Lead a healthy lifestyle.
A few words about the disease
Varicocele is a disease that is manifested by dilation of the veins of the spermatic cord. Who is at risk? The pathology can occur in a boy aged 10 to 14 years. At first it may not manifest itself in any way, but later the clinical picture will be obvious. The danger of the disease is that any physical activity can cause a worsening of the condition. The fact is that intense physical exercise leads to an increase in the intensity of blood flow through the veins. If the venous network is normal, there will be no problems. But in the presence of varicose veins, there may be complications in the form of trophic ulcers and thrombosis. Blood clots that form in the cavity of the vessel interfere with normal blood circulation. That is why various forms of pathology may be a contraindication for military service. On the pages of our website there is a comprehensive list of which diseases are not accepted into the army.
Varicocele disease and its symptoms
Varicocele is an enlargement of the veins of the pampiniform plexus of the spermatic cord in young men and adolescent boys. There are often alternative signs of pathological changes in the venous system - the appearance of varicose veins in the legs, the appearance of hemorrhoidal cones. Varicocele, in most cases, occurs on the left side, since the spermatic vein enters the renal vein at a ninety-degree angle to the left.
In the first stages, this pathological condition may not have visible and tangible manifestations and can only be diagnosed by ultrasound.
The insidiousness of this disease is expressed in the following: serious physical activity, which is practiced in the army, and uncomfortable underwear can cause a serious deterioration in the current condition. During serious physical activity, the intensity of blood movement through the veins increases, and underwear compresses the body, and only aggravates this situation. The conscript begins to experience nagging pain in the groin area, which can radiate higher. The pain will increase with exercise, and in the case of an advanced form, there is a risk of infertility.
How to undergo a medical examination
Although varicocele is a potentially “non-appealing” disease, it is not easy to get a “white” ticket with such a diagnosis.
Often doctors simply do not pay attention to this disease, considering it “not serious.” They are trying to convince the conscripts themselves of this, proving to them that they are healthy and ready to do military service.
With this diagnosis, much depends on proper preparation for the medical commission. When going there, you must have all the certificates, doctor’s reports and test results in hand.
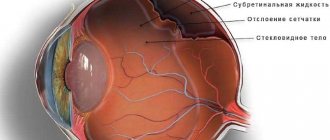
Healthy and affected varicocele vessels of the spermatic cord.
It is important that the wording in medical documents matches the terminology used in the Schedule of Diseases. For example, if the disease had several relapses, then each case should be described in detail, indicating their number and exact time. The documents must also describe the symptoms that accompany the disease: pain, hematuria, impaired spermatogenesis.
It is even better to confirm the diagnosis of “grade 3 varicocele” in an independent medical institution and provide it to the draft committee.
If you are confident in your diagnosis, but doctors refuse to accept it, then you should not be afraid to go to court or a higher authority. The draft decision will be suspended during the trial.
It should be remembered that damage to the venous system does not go well with military service. Physical activity leads to exacerbation of varicocele, and without it in the armed forces there is no way.
Military service and varying degrees of illness
It should be said right away that in most cases, varicocele and the army are completely compatible concepts. The initial stages of an illness are not considered sufficient grounds for exemption from service.
The first degree of the disease is secretive; usually young people themselves are unaware of their diagnosis. Therefore, it absolutely does not interfere with military service. Even if the disease is discovered during a medical examination, the conscript is unlikely to be able to count on category “B”.
With varicocele of the 2nd degree, the clinical picture of the disease is much more pronounced, but it is usually not a basis for a commission. According to the Republic of Belarus, with the second degree of pathology with a single relapse, they are accepted into service with category “B-3”. In this case, the choice of troops to which the conscript can be sent will be limited.
Heavy physical activity can trigger the development of the disease. Therefore, the military is not a good fit for young people with varicoceles.
To avoid conscription with the second degree of the disease, it is necessary to confirm frequent relapses of the disease and repeated requests for help from a surgeon. In this case, the young man can receive category “B” and be enrolled in the reserve.
Young men with the 3rd degree of illness have the greatest chance of being exempt from conscription. According to the Republic of Belarus, having such a diagnosis, a person liable for military service can count on the “non-conscription” category “B”. However, rarely does anyone get it right away. Usually this requires two or three calls, that is, at least one year.
Do they take into the army with recurrent varicocele?
Often, this disease can manifest itself after surgery. Recurrence of varicocele (after surgical intervention) gives the right to take a military ID and qualify for fitness category “B” in the case where the conscript himself refused further treatment. With a single relapse, varicocele does not serve as a basis for complete exemption from military service and obtaining a military ID in accordance with the state of health.