Almost all ophthalmological diseases are accompanied by refractive errors - incorrect refraction of light in the transparent structures of the eye, resulting in the inability of the visual system to focus a clear image in the intended macular zone of the retina. Depending on the severity and nature of refractive pathology (farsightedness, myopia, astigmatism, various combinations thereof), the most appropriate measures to restore vision clarity are prescribed in each individual case: optical correction, ophthalmic surgery, excimer laser therapy, hardware training, etc.
While some pathological conditions are relatively stable, others may occur with difficult to predict dynamics of refractive errors, or with such a degree that the optical power of glasses or contact lenses is insufficient to ensure an acceptable quality of life. One of these diseases is keratoconus: changes in the biochemical composition and mechanical characteristics of the cornea gradually lead to its deformation - the cornea becomes thinner, loses elasticity and, under the influence of tension, is pulled forward along the anteroposterior ocular axis. In this case, the light in front of the pupil is refracted not by a spherical shell, as is normal, but by a surface pointed in the shape of a cone apex (hence the name of the pathology). This inevitably leads to gross combined violations of normal refraction - as a rule, there is a combination of myopia and complex astigmatism - the optical parameters of which also constantly change as keratoconus progresses. If at the early stages of the process vision is still corrected with hard contact lenses, then in the future they would have to be constantly changed, however, this would not provide acceptable clarity of vision.
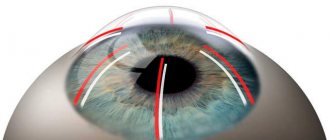
The main therapeutic goal for keratoconus is to restore the natural sphericity of the cornea. For this purpose, various approaches are practiced. One effective method is the implantation of intrastromal rings (“intra” means “inside”; stroma is the underlying transparent tissue of the cornea). In a geometric aspect, such rings should level the curvature of the corneal surface and bring it closer to a spherical shape, artificially thickening the surrounding areas that lag behind the “top”. Intrastromal rings, formed by two thin semicircular arcs, are made from transparent biocompatible synthetic material. They are durable and reliable; at the same time, they can be quite simply removed or replaced in accordance with clinical dynamics.
How do intrastromal rings work?
To a first approximation, the method can be likened to a children's pyramid, where thick rings are placed on the central axis; however, the thickness and diameter of the rings (unlike a children's toy, one or, at most, two rings are used here) are selected in such a way that the assembled “pyramid” has a spherical rather than conical profile. Calculating refraction in this case is a complex task, but still it has a solution that provides the optical system of the eye with a refraction that would be as close as possible to the standard one. It is interesting to note that the biomechanical mechanisms that “raise” the thickness of the periconal layers to the required level remain not yet entirely clear, but the empirical effectiveness of the method is beyond doubt.
Intrastromal corneal rings
These rings are implanted deep into the cornea. This operation takes little time and is practically painless. It is performed on an outpatient basis under local anesthesia using drops.
Using a layer-by-layer vacuum dissector, an arc-shaped pocket is created into which the rings are placed. A similar action is performed using a more modern femtosecond laser.
After the implantation of the tracks, additional pressure occurs, which changes the curvature of the cornea and leads to a flattening of the apex of the cone. In addition, due to the outer epithelium, a significant leveling of the cone occurs and the cornea returns to its natural shape.
Ferrara Rings have a smaller radius of curvature than Intacs (2.5 and 3.5 mm, respectively). In the first case, the likelihood of glare is much less, since they have a prismatic shape. When a ray of light hits the ring, it is reflected from it and does not penetrate deep into the eye. To reduce this effect, Ferrara Rings are placed closer to the center. Thanks to this, they can correct refractive errors of up to – 12 diopters.
After the implantation of the tracks, additional pressure occurs, which changes the curvature of the cornea and leads to a flattening of the apex of the cone.
Patients with larger pupil diameters are more likely to experience glare. In such cases, the use of Intacs rings is more justified. In most cases of implantation of intrastromal rings, their effectiveness is quite high. There is an improvement in vision both with and without correction. However, the patient groups are not yet large enough to make a clear judgment about this technique. Within 24-36 months, all patients showed improvement. However, the best results were achieved in patients with mild or moderate keratoconus.
Possible complications include failure to achieve results, development of infection, postoperative displacement of the ring, perforation of the anterior chamber and aseptic keratitis. If such changes occur, you can easily remove the rings and return the cornea to its original appearance. In approximately 10% of cases of unsuccessful interventions, lamellar or penetrating keratoplasty is performed. Pre-installation of stromal rings does not interfere with the operation.
- Interesting
Keratoplasty (cornea transplant) in Ukraine
Today keratoplasty in Ukraine is an urgent and extremely popular operation for many patients. Unfortunately, according to existing...
Indications for installation
T.N. secondary keratoconus develops against the background of iatrogenic (Greek: “caused by medical intervention”) keratoectasia, i.e. uneven deformation of the cornea due to excimer laser correction. Considering the long-proven safety of laser therapy, i.e. low probability of such complications and side effects; iatrogenic secondary keratoconus is rare in ophthalmological practice. However, it is, of course, necessary to eliminate it, and implantation of intrastromal rings is one of the ways to correct such unfavorable consequences of laser exposure.
In other cases, implantation of rings helps restore vision after injury (including post-operative trauma as a result of keratotomy) or with thinning of the cornea, which sometimes results in complex irregular astigmatism in combination with a high or very high degree of myopia (myopia).
Finally, primary keratoconus as an independent disease, especially its progressive variants, also requires optical correction, which can often only be achieved with a transparent artificial thickening around the protruding apex of the cone.
The current level of ophthalmological technology and methodology makes it possible to implant intrastromal rings without hospitalization.
General anesthesia is also not required (which eliminates possible contraindications for certain categories of patients). All manipulations are carried out “in one day”, on an outpatient basis, under reliable drip anesthesia. Corrective rings are inserted through microscopic incisions on the periphery of the cornea. The total duration of the intervention does not exceed 25-30 minutes; Due to the gentle, minimally invasive nature of the procedure, the rehabilitation period is reduced to a minimum.
Comprehensive treatment of keratoconus
Modern complex methods of treating keratoconus make it possible to slow down, stop and, if possible, correct refractive defects without the need for a corneal transplant surgery.
Relatively recently, treatment of keratoconus was limited to the patient wearing hard contact lenses until the progression of the disease caused thinning of the cornea, localized opacification, decreased visual acuity, persistent intolerance to contact correction and the inability to obtain adequate visual acuity with spectacle correction. In this situation, the need for penetrating keratoplasty (penetrating corneal transplantation) was considered the only possible and correct tactic for the surgical treatment of keratoconus.
As is known, the operation of end-to-end corneal transplantation has its advantages and disadvantages.
The difficulty of obtaining QUALITY donor material, the possibility of its rejection both in the immediate and long term, the possibility of postoperative infection, the high probability of obtaining high postoperative astigmatism and the long period of postoperative rehabilitation make penetrating keratoplasty far from the most reliable method of treating keratoconus.
The concept of modern treatment of keratoconus rests on three basic conditions:
- Slow down the progression of the disease.
- Stabilize corneal anatomy.
- Achieve the best possible visual acuity
Complex treatment of keratoconus is a professionally competent combination of the following modern techniques:
- Cross-linking of corneal collagen using RiboflavinRead more
- Implantation of INTACS intrastromal rings using the Intralaser femtosecond laserRead more
- Phakic and aphakic intraocular correction
In this video you can watch the progress of the operation - implantation of a phakic lens to a patient after the operation to implant INTACS intrastromal rings.
Cross-Linking is a new technique for treating keratoconus, widely used in European clinics, developed in Germany and Switzerland.
The procedure is recommended for stage 1-2 keratokunas with disease progression.
Using dosed ultraviolet radiation from a specially designed laser onto the stromal layer of the cornea, it is possible to slow down and sometimes even stop the progression of the disease keratoconus and avoid the need for a corneal transplant.
+ The procedure is absolutely painless,
+ Performed on an outpatient basis,
+ Takes about 90 minutes (per eye).
At the first stage of the procedure, special drops containing a photosensitive component are instilled, saturating the stromal layer of the cornea with it.
The second stage - the ophthalmologist uses a laser on the cornea saturated with this substance.
As a result of the procedure, the cornea is “cemented” and its structure is strengthened, which slows down its further thinning and arching in the center.
As a result of the procedure, the progression of keratoconus is stopped and the refraction of the eye remains stable.
After cross-linking, there is no improvement in refraction; the procedure is aimed only at strengthening the cornea, but not at optical correction of keratoconus. The cross-linking effect lasts for 4-5 years, after which in some cases it is necessary to repeat the procedure.
As a result of clinical trials of the Cross-Linking procedure conducted in 5 European countries, no pathological effect of ultraviolet radiation on the lens or retina was noted, due to dosed penetration through the cornea saturated with riboflavin.
Crosslinking of corneal collagen
The idea of using a conservative method for treating keratoconus came from a group of researchers at the Technical University of Dresden. T. Seiler and G. Wollensak, who took as a basis the principle of photopolymerization, which has long been used in dentistry (“light filling”).
As a result of scientific research, the safest and most effective technique for cross-linking (transverse “gluing”) of corneal collagen was developed, based on the effect of photopolymerization of stromal fibers under the influence of a photosensitive substance (riboflavin solution) and low doses of ultraviolet radiation from a solid-state UVA source.
It has been proven that under the influence of ultraviolet radiation and riboflavin, intramolecular cross-links of corneal collagen are strengthened with the formation of dimers of two α-chains without degradation of collagen proteins. For use in clinical practice, a device with a solid-state ultraviolet source was developed, having two tips and a power adjustment button.
Stages of the crosslinking operation
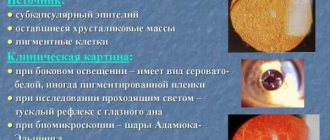
At the first stage, the cornea is de-epithelialized and 2-4 drops of a solution containing 0.1% riboflavin, 20% dextran and anesthetic are instilled. After 30 minutes, using a slit lamp with a blue filter, a yellow flash is detected in the anterior chamber (which indicates saturation of the cornea). Then, using ultrasound pachymetry, the thickness of the cornea is determined, which should be at least 400 microns.
At the second stage, ultraviolet exposure is performed. Ultraviolet radiation with a wavelength of 365 nm is focused on the cornea, with a distance from the source to the cornea of 5-6 cm. Additional riboflavin is instilled within 30 minutes at intervals of 2 minutes. After surgery, a soft contact lens is applied and topical antibiotics, anti-inflammatory drugs, and steroids are prescribed.
Studies have been conducted and it has been calculated that with standard therapeutic radiation power (3 MW/cm²), energy at the level of the deep layers of the cornea is safe for the endothelium (with a corneal thickness of more than 400 microns). However, in cases of advanced keratoconus with severe thinning of the cornea, the standard dose of exposure is detrimental to endothelial cells.
In 2013, Sergey Vladimirovich Kostenev first patented a technology for performing corneal collagen crosslinking in patients with thin corneas and using a soft contact lens without a UV block. Its meaning is to use a hydrogel soft contact lens with a thickness of 100 microns without a UV filter, which allows surgery in patients with thin corneas by increasing the overall thickness of the cornea and eliminating the damaging effects of ultraviolet radiation on the endothelial layer of the cornea.
The use of the developed treatment method makes it possible to perform the crosslinking procedure in patients with keratoconus in cases where the central thickness of the cornea after deepithelialization is less than 400 μm.
After cross-linking surgery, there was an increase in uncorrected visual acuity by an average of 1 to 2 lines and corrected visual acuity by 1 line a month after treatment. The only side effect of the Femto-KRK procedure was short-term corneal edema. It was observed in approximately 40% of cases.
Numerous experimental and clinical studies have shown the effectiveness and safety of the riboflavin-UVA-induced corneal collagen cross-linking procedure for the treatment of progressive keratoconus.